Has menopause come up in conversation at your annual gynecology visit? Surprisingly, studies indicate gynecologists and family practitioners can often overlook or be less than confident discussing this natural stage of life. Many doctors admit they’re ill-informed about menopause, never receiving sufficient formal training during medical school and residency.
Although there have been improvements in the opportunity to enhance such education, it is critically important for women to become well-versed. Gynecological changes are just one part of the menopause transition. Menopause can impact a woman physically, mentally, and emotionally. And often sooner than you may think. That’s why women need to take action, even before menopause symptoms begin, especially if their doctors are not talking about it.
Why your doctor may not know about menopause
Annual well-woman+ gynecology visits typically focus on cervical cancer screenings, breast exams, mammograms, and conversations about sexual health and birth control if you’re not trying to conceive.
Unfortunately, the conversation doesn’t always shift to menopause once you’re in your 40’s and of “advanced maternal age.”
Physicians typically have more experience and education in pregnancy and childbirth than in the management of the menopause journey.
For years, the vast majority of OB/GYNs have told researchers they did not receive training in menopause medicine. In a Johns Hopkins survey, 7 out of 10 said they would have liked that.
A study published in 2023, shows this knowledge gap is still there. Only 1/3 (31.3%) of OB/GYNB program directors reported having a menopause curriculum. There’s not standardized curriculum or tools and only 29.3% of trainees (residents) spent time in a menopause clinic.
The lack of training combined with the unique nature of every woman’s menopause journey makes it more difficult for doctors who haven’t received adequate training to identify and address a woman’s menopause symptoms and offer the best treatment for her individual circumstances.
How to talk to your doctor about menopause
Just because your doctor may not have adequate training doesn’t mean they won’t listen. Doctors care and want to help. That’s why most wanted to become physicians in the first place.
Interestingly, the vast majority of women in the pausitive health menopause survey were extremely satisfied or somewhat satisfied with the care they received from their primary care practitioner (PCP) or OB/GYN.
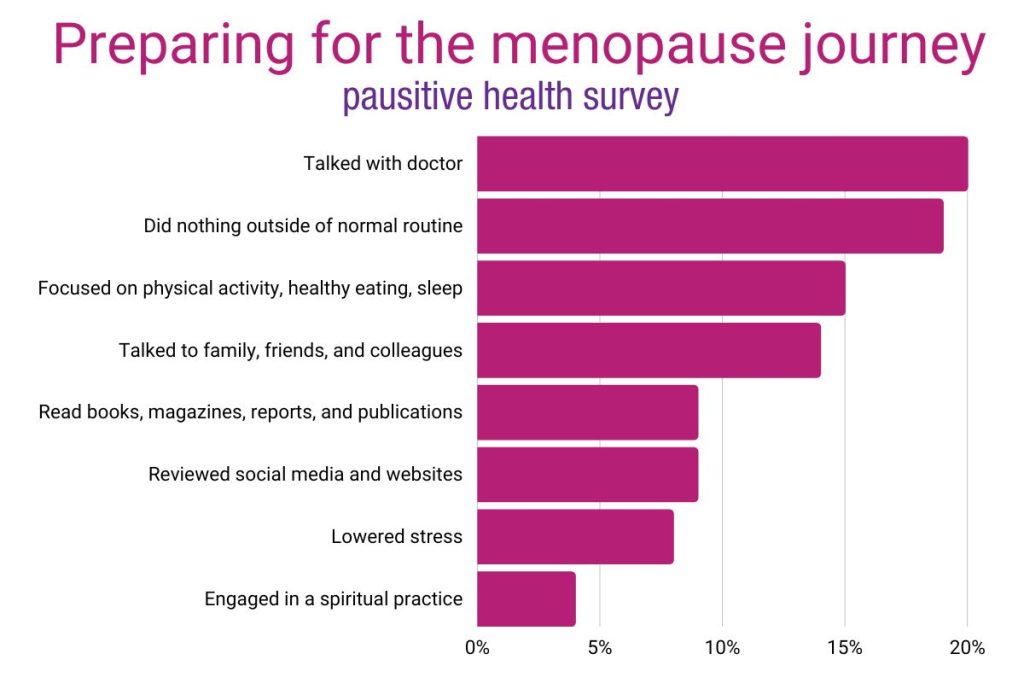
But, the reality is the majority of women+ are not asking them their doctor for help. In the pausitive health survey, only 20% of women talked with their doctor.
The few women who talked to their doctor and were not satisfied, indicated their doctor:
- Did not listen to their concerns.
- Only offered a prescription.
- Provided no solutions.
- Had a lack of knowledge about menopause.
Again, this was a small number of women.
Knowledge is power. Understanding your doctor may or may not have the formal training is a first step in taking action.
Think about the care you’re receiving and re-evaluate whether your doctor is the best one for you, given the life cycle you’re in.
Have You Asked Your Doctor These Questions?
Download this list of questions and take them to your next doctor’s appointment.

"*" indicates required fields

Planning for menopause should be like pregnancy planning
Like a pregnancy, every woman has a unique menopause transition. It’s a transition because menopause is a gynecological event that refers to the point at which you have had 12 consecutive months without a period.
However, the transition into and out of that moment can last seven to ten years, and women may experience physical, mental, and emotional changes during that time.
Like pregnancy, there are common symptoms that doctors should discuss with their patients.
Up to 80% of women experience hot flashes. In a pausitive health menopause survey, it was the most common symptom.
Women+ also reported experiencing fatigue, night sweats, mood swings, sleeplessness, loss of libido, brain fog, and weight gain.
Some of these symptoms can be managed with lifestyle adjustments. It’s never too late to make those, but starting before symptoms hit, sets you up for a more manageable transition.
Just like you plan for pregnancy, women should prepare for menopause. Actions you do or do not take today can impact you ten years from now! Whether they are for better or for worse is up to you.
For example, if you’re starting menopause ten pounds heavier than you should be, what happens when your metabolism slows during menopause? Will you gain ten more pounds? Ten pounds can quickly become twenty pounds or more.
If you’re overweight, you may also experience more symptoms. In a sample of 1776 women in the SWAN, a higher percentage of body fat was associated with increased odds of hot flashes or other vasomotor symptoms like night sweats.
Menopause symptoms vary from woman to woman, just like in pregnancy.
But, there’s no doubt the healthier you are, the better off you’ll be. Focusing on the basics – healthy eating and physical activity – can go a long way.
Doctors should help women plan for menopause as they help women prepare for pregnancy. If that’s not happening, it may be time to find a doctor with more training and expertise. If you chose your OB/GYN years ago, are they still the best fit to support you through menopause?
The answer may be no because, as studies have shown, many don’t have adequate training in menopause.
Finding a menopause doctor
Some doctors specialize in menopause care, but the number of certified menopause doctors with The Menopause Society is small compared to practicing OB/GYNs.
It’s also not a board certification. However, it’s a step in the right direction with doctors who have taken additional training and passed a competency exam on menopause.
Find a Certified Menopause Practitioner near you or member of The Menopause Society..
While the members may not have the certification, they are interested in providing healthcare for women in the menopause transition.
Menopause is also becoming a specialty for hospital systems. Major hospital systems like the Menopause and Midlife Clinic at Brigham and Women’s Hospital in Boston and Northwestern’s Center for Sexual Medicine and Menopause in Chicago launched clinics focused on comprehensive care during midlife and the menopause transition.
Find a team of advocates
When it comes to menopause, you may need a different approach to healthcare than you’ve sought before.
While you’re treating one life event during the menopause transition, you may seek the advice of several experts who holistically care for your health.
I wish menopause was not so difficult and that all points could be solved by one doctor.
respondent, pausitive health menopause survey
In the pausitive health survey, women said they sought the advice of other healthcare providers – psychiatrist, acupuncturist, endocrinologist, neurologist, dietician, urogynecologist, personal trainer, and dermatologist – in addition to their primary care doctor or gynecologist.
That was a source of frustration for one woman in the pausitive health survey who wanted one doctor to solve it all.
The menopause transition impacts every woman differently. Consider experts who look at your health holistically and surround yourself with the most supportive team of experts who support you in managing your symptoms – with or without hormones.
While hormone replacement therapy is commonly prescribed, there are dozens of non-hormonal options to manage symptoms.
Seek out alternatives
Your doctor is one source of information, but there are other reliable sources of menopause information.
In the pausitive health survey, no one way stood out as the predominant preparation method.
Interestingly, nearly 40% of the women either talked to their doctor or did nothing. Talk about two extremes!
If you do nothing, it will be difficult to make a change for the better, which is what pausitive health is all about. Just being here, means you’re ready to do something and make a change.
Others talked to friends and families, lowered stress, or read books.
You don’t have to do what everyone else is doing. Take hormones for instance. They work great for some women, while others want to avoid them, or can’t take them. Know that you have options in those situations too.
There are dozens of non-hormonal treatment options that can help you and there are even non-hormonal medications.

Take action – you’re your own best advocate
Don’t underestimate the value of caring for yourself. After all, the menopause transition can last 7 to 10 years.
Do you want the best advocate(s) on your side for the next decade?
Knowledge is power! The menopause journey is a perfect time to become a “healthcare rebel.”
Many of the survey respondents were not aware of the offerings that are now becoming available to help educate and address the physical and emotional health issues many women experience during he menopause journey and beyond.
Today’s women are aging in an exciting time in the healthcare industry. There’s an entire segment – FemTech – dedicated to solving longstanding health issues for women.
While your local gynecologist or general practitioner might be the person you’ve always sought out for care, there are new and exciting ways to connect women with other menopause experts to get the support you need.
Think of menopause like pregnancy. Preparation goes a long way to increasing the likelihood of the best outcome possible in your given situation. And, like with many pregnancies, it represents a new stage which can be filled with excitement, joyous moments, and a lot more life to be lived. It’s time to make your health and well-being a priorities.
Gynecologist Develops Menopause Guide for Physicians | Johns Hopkins Medicine
What Do Ob/Gyns in Training Learn About Menopause? Not Nearly Enough, New Study Suggests | Johns Hopkins Medicine
Allen J, Laks S, Zahler-Miller C, Rungruang B, Braun K, Goldstein S, Schnatz P. Needs assessment of menopause education in United States obstetrics and gynecology residency training programs. Menopause ():10.1097/GME.0000000000002234, August 8, 2023. | DOI: 10.1097/GME.0000000000002234
Green R, Santoro N. Menopausal Symptoms and Ethnicity: The Study of Women’s Health across the Nation. Women’s Health. 2009;5(2):127-133. doi:10.2217/17455057.5.2.127
Find a Menopause Practitioner | The Menopause Society
Menopause and Midlife Clinic | Brigham and Women’s Hospital
Center for Sexual Medicine and Menopause | Northwestern Medicine
Be a Healthcare Rebel: How to Get the Best Medical Care | PeopleTweaker
You may also like…

5 Ways Medical Gaslighting Can Make Your Menopause Journey More Difficult
Do you feel like your doctor dismisses your menopause symptoms? Medical gaslighting can leave you feeling crazy and make menopause harder.

Non-Hormonal 101
95% of women… would try hormone alternatives before HT. Source: Women’s Health Concern Non-Hormonal Options 101 How are you managing your menopause symptoms? You have choices, both hormonal and non-hormonal. It’s your body, and you have the power to select (in consultation with your healthcare provider) the option(s) that’s best for your situation. Some women

Women of Color
Extremely challenging…. is how 25% of both Black and Hispanic women and Latinas described their menopause symptoms in a pausitive health survey. Only 12% of white women and 7% of Asian women used the same description. Women of Color: The Many Shades of Menopause For many women of color in the United States, the menopause

