Symptoms
You are not alone! Approximately 85% of women report menopause symptoms.
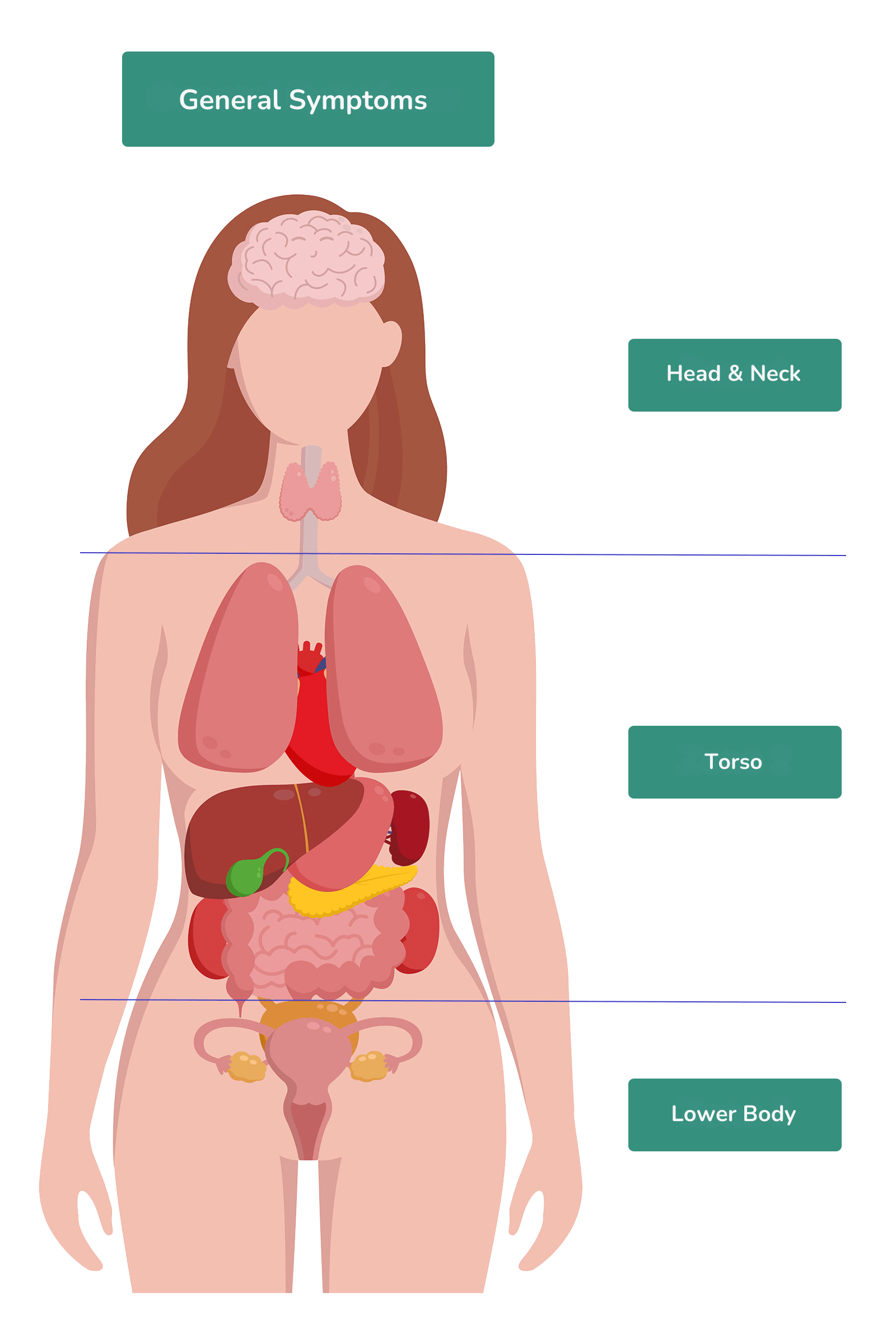
The menopause journey can impact you from head to toe. Sometimes, it’s a specific area and other times, you’re feeling it all over like itchy skin or muscle aches.
With a seemingly endless list of symptoms that could be related to the menopause journey, it can be challenging to sort things out. That’s why we’ve broken the body up into 4 parts to help you better understand why you feel the way you do and actions you can take to help manage your menopausal symptoms.
You can choose an area of the body where you’re having symptoms or keep learning here about general or full-body symptoms like:
- body odor
- cold flashes (not a typo!)
- fatigue and exhaustion
- hot flashes or night sweats
- muscle and joint aches and pains
- skin and nails
- sleep
Need help with another menopausal symptom? Choose another area of the body.
Talk to Your Doctor
Discuss your symptoms with your healthcare practitioner. While many often are associated with the menopause journey, some can also be a sign of a more serious health condition.
Also, ask about the best ways to address symptoms in your particular situation. Remember, there are lots of potential options, including medications and OTC products (including hormone therapy and hormone-free medications) as well as non-hormonal techniques.
General Symptoms
Body odor
This “stinky” menopause symptom is less common, but it’s bothersome for the women+ in the pausitive health survey who told us they have to deal with it.
During the menopause journey, some women+ notice their overall smell changes or they notice a change in a body part. This may be their armpits, skin, vagina, or urine. The smell can be unpleasant, ranging from tangy to dead fish!
Take action to improve how you smell and feel.

Feeling Stinky? What Causes Menopause Body Odor And How To Smell Better
Have you noticed a new body odor during menopause? It can be overall, in your armpits, or your vagina. Learn about the cause and solutions.
Cold flashes
For many of the same reasons women experience hot flashes, a woman+ can experience a cold flash. It’s a sudden rush of a cold sensation throughout your body, but women say it feels different than that cold feeling you have when you’re not feeling well.
Cold flashes during the menopause journey can happen during the day or night.
Like hot flashes, women can manage cold flashes with:
- non-hormonal techniques
- non-hormonal medications
- hormone therapy
- wearable devices
- lifestyle changes

10 Ways To Beat The Chill During A Menopause Cold Flash
Are you having cold flashes? It’s a menopause symptoms, and yes we mean cold – not a hot flash! Learn how to beat the chill.
 Fatigue and exhaustion
Fatigue and exhaustion
Are you feeling tired all the time? Fatigue can be physical and/or mental and involves feeling severely tired, no matter how much sleep and rest you get.
Exhaustion is a situation in which you feel extreme fatigue.
Of course, we all feel tired from time to time, but what makes fatigue different is the inability to get through the day. It can affect your mood, ability to focus and concentrate, exercise, or your daily routine.
Causes of fatigue
There are many potential causes of fatigue, including the menopause journey. For example, menopausal symptoms like sleeplessness, hot flashes and night sweats (which can lead to problems with sleep or make pre-existing issues with sleep worse), or the mental energy exerted to try to compensate for brain fog can lead to fatigue or exacerbate it.
And for the majority of women+ who embark on the menopause journey during midlife, pressures from work and juggling life at home, which may include taking care of children and aging parents, can be draining, both physically and mentally.
While fatigue and exhaustion can be a symptom of the menopause journey for women+, talk with a doctor or other healthcare professional, as there are other medical reasons for fatigue. They include:
- not getting enough high-quality sleep
- being chronically dehydrated
- chronic fatigue syndrome (CFS)
- fibromyalgia
- thyroid disease
- chronic pain
- cancer and cancer treatment
- anemia
- chronic conditions like diabetes, COPD, congestive heart failure, liver disease, kidney disease
- autoimmune conditions
- depression and anxiety
- poor nutrition, eating disorders, being underweight
- sleep disorders like sleep apnea and narcolepsy
- medication
- infections
- long COVID
It’s important to find out the root cause of your fatigue and exhaustion in order to know the best way to proceed.
For example, although it may seem counterintuitive, regular exercise can often help. But if you have long COVID, some types of exercise are better than others, and vigorous exercise can make things much worse or even cause a major setback.
Ways to energize your body and refresh your mind
You can do several things to regain energy and help get over fatigue and exhaustion during the menopause journey. These steps may also help you manage other menopause symptoms.
- Use food to fuel your body. Focus on foods rich in vitamins a woman’s body needs during menopause. Energy-rich foods include fruit, vegetables, fish, chicken, and whole grains. And avoid spicy foods, caffeine, and alcohol, as they may trigger hot flashes and also negatively impact sleep.
- Get enough good-quality sleep. Figure out why you can’t sleep. Are you experiencing restless leg syndrome or leg pain at night? Find the source of your sleep issues. Then, think about creating or revamping your sleep routine. You can also learn ways to relax your mind and body before bed. Taking a quick nap might also help, but avoid more than 20-30 minutes. Longer than that, you may awake feeling groggy rather than refreshed, which also disrupts your sleep later.
- Drink lots of water. It hydrates your body.
- Get exercise. Even a walk outside can refill your cup and energize you enough to make it through the day. Gradually add more exercise as you chip away at fatigue and exhaustion.
- Prioritize so you don’t feel overwhelmed and can feel like you accomplished something each day rather than wading through an endless To-Do list. And sometimes the best action you can take is to surrender and accept the reality that there is only so much anyone can get done in a day.
- Learn coping skills to help manage stress. You can start by relaxing your mind and body with techniques that include meditation, guided imagery, and yoga nidra. Then, make it a priority to de-stress with some self-care.
- If you’re an extrovert, socialize with friends and family. It’ll help you tap into energy to help alleviate your fatigue.
- If you’re an introvert, take some “me” time to focus on recharging your tank.
- Get help from your healthcare provider. If hot flashes, night sweats, sleeplessness, depression, anxiety, or other menopausal symptoms contribute to or are the root cause of your fatigue, you have options. Speak with your doctor about hormonal and non-hormonal possibilities and come up with a plan that is effective for you.
The menopause transition is a journey that lasts up to 10 years for most women+. Don’t spend it exhausted and suffering in silence. It’s time to make a change for the better!
Hot flashes and night sweats
Hot flashes tend to affect Black and Hispanic women+/Latinas more than other racial groups, and Black women often experience them with more intensity/severity and a longer duration during the menopause journey.
Hot flashes are a component of symptoms referred to as vasomotor symptoms or VMSs. VSMs include hot flashes, night sweats, and palpitations.
Women+ typically feel hot flashes mostly in the head, neck, chest, and upper back. They can also cause sweating or flushed skin (redness in the face especially).
Some ways to manage hot flashes
Hot flashes can last for years and there is also a potential relationship between having more hot flashes and night sweats and the risk of stroke and dementia, so it’s important that you look for treatment options. These can include:
- changing the foods you eat
- reducing or eliminating the consumption of caffeine, alcohol, and other trigger foods
- cognitive brain therapy
- wearable devices (like the Thermaband and the Embr Wave)
- herbal remedies
- non-hormonal medications
- hormone therapy

Clear Your Mind: 5 Potential Herbal Remedies for Menopausal Brain Fog
Menopausal “brain fog” (or menofog) is a real thing, but it doesn’t have to be the end of the road. While treatment options are lacking, herbs hold promise.

Hormone-Free Hot Flash Relief: 12 Non-Hormonal Medications To Try
Want to beat the heat from hot flashes hormone-free? Try these non-hormonal hot flash medications that are FDA-approved or used off-label.

Black Women and Menopause: Why Symptoms Can Be Longer and More Severe
As a Black woman, menopause symptoms, including hot flashes, can be longer and more severe. Learn why and what you can do.
 Muscle aches and pains
Muscle aches and pains
Are you feeling achy or stiff all over? There could be many reasons, one of which might be the menopause journey.
New research shows that muscle aches and pains can be more common in women+ in midlife during this stage of life, with up to 70% reporting this symptom. There’s even a name for it now – the musculoskeletal syndrome of menopause (MSM).
It can include:
- frozen shoulder – inflammation of the shoulder capsule (adhesive capsulitis) that can “freeze” your shoulder making it hard to move your arm.
- ligament or tendon injury
- osteopenia (bone thinning) or osteoporosis (bone loss)
- loss of muscle mass and strength (sarcopenia)
- joint pain
The hormonal changes during the transition (volatile and falling levels of estrogen and progesterone) impact muscles and joints because estrogen receptors are all over the body.
Then, there is the wear and tear on the body as one ages. In addition to preexisting conditions, you may have arthritis, fibromyalgia, lupus, and sickle cell disease.
And being sedentary, depressed, stressed, or anxious can also lead to muscle and joint aches and pains or make them worse.
Chronic pain
Some studies suggest that women who have a heavy burden of menopause symptoms are more vulnerable to chronic pain. If you have severe menopause symptoms, the stiff, achy muscles and joints can become more than a nuisance and evolve to issues with chronic pain. This may also be the case if you’ve had chronic pain at another point in life or leading up to menopause.
Chronic pain is defined as persistent or intermittent but lasting more than 3 months.
Up to 85% of patients with chronic pain also have depression. During menopause, the risk of depression increases, starting in perimenopause.
So, don’t ignore your pain and what your body tells you.
Sleep apnea and chronic pain
Do you have sleep apnea or do you suspect you do?
Sleep apnea leads to insufficient oxygen getting to your body and can also lead to general inflammation. It also results in an increased risk of hypertension (high blood pressure), heart disease, and stroke. These are all conditions for which the risk is already increased during the menopause journey.
Unfortunately, women+ are also at greater risk of sleep apena during menopause due to the hormonal transition which occur during this stage of life.
A study published in 2022 in Menopause, The Journal of The Menopause Society, found a significant association between sleep apnea and chronic pain among postmenopausal women.
If you haven’t been tested for sleep apnea and have severe joint pain and fatigue, researchers believe testing is warranted for sleep-disordered breathing.
So, what can you do about the pain?
First, check with your healthcare provider to help determine the root cause of your aches and pains, particularly if they are sudden and/or severe. That can provide information to guide the actions you can take, including both hormonal and non-hormonal options.
In general, physical activity can be a good place to start in many instances, often regardless of the cause of the discomfort. Moving your body improves blood flow, strength, flexibility, balance, your posture, and lubrication of the joints.
It also has the extra bonus in many of having a positive impact on depression, stress, and anxiety, all of which are more common during the menopause transition. And don’t forget to get enough good-quality sleep and find ways to relax your body and mind, like meditation, guided imagery, body scans, and paced breathing.
Check out these exercises designed with menopausal women+ in mind. But be sure to make sure your healthcare practitioner has provided advice regarding the type and levels of activity that will be safest for you, particularly if you have been sedentary for a long time or have underlying medical conditions.
Also, take a look at your weight. It’s common during the menopause journey to put on extra weight, especially in the midsection. It can put extra pressure on your joints and muscles, which can cause them to hurt. And having a lot of internal fat in your abdomen sets up inflammation in the body, which can contribute to aches and pains. Having and maintaining a healthy weight will serve you well both now and for the rest of your life.

What You Need to Know About the Musculoskeletal Syndrome of Menopause
Feeling new joint pain even though you don’t have an injury? Musculoskeletal syndrome of menoapuse can cause aches and pains. Get treatment.

Yoga For Lifelong Strength: 5 Yoga Types To Power Through Daily Life
Yoga can provide lifelong strength. Learn about 5 yoga types and the benefits so you can power through daily life.

Discover Inner Balance: 8 Yoga Poses To Help Manage Menopause Symptoms
Yoga can improve your emotional and physical well-being during menopause, easing symptoms like hot flashes and sleeplessness. Try these yoga poses. for menopause.
 Skin and nails
Skin and nails
Is your skin dry and itchy? 72% of women in menopause reported skin changes in a 2018 survey.
Are your nails brittle? 19% of women younger than 60 report brittle nails, and the number rises to 35% after age 60.
The natural drop in estrogen levels impacts collagen in your skin. That leaves it dry and itchy. Moisturize, moisturize, moisturize.
Falling estrogen levels can also be a culprit when it comes to your nails. Nails are made of a protein called keratin. The drop in estrogen levels during the menopause journey weakens the keratin layer and can make them brittle and easy to break.
How to prevent brittle nails
There are things you can do to help your nails.
- Limit the use of nail polish remover with acetone and harsh chemicals, which can be very drying and exacerbate the situation.
- Protect your nails (and hands) with gloves when washing dishes and other activities where they may be exposed to hot water and chemicals.
- Avoid gel nail extensions and acrylic tips, as they can be damaging and make brittle nails worse.
- Don’t file the surface of your nails.
- Moisturize.
Several supplements may be worth discussing with your healthcare provider, including:
- biotin – may help strengthen your nails and help them grow. You can also get biotin from foods like liver, eggs (the yolk), salmon, legumes (e.g., lentils, peanuts), soybeans, yeast, salmon, avocado, sweet potato, nuts, and seeds.
- zinc – helps promote healthy growth. It can be found in fish, beef, poultry, black beans, almonds, and eggs.
Although most people get enough protein, the amount you need to eat increases as you age and lose muscle mass. Keep an eye on your intake to help ensure your consumption is adequate, especially if you have been sedentary and start a vigorous exercise. Eat these lean protein foods to help during the menopause journey.
Your doctor may also check for conditions like iron deficiency and thyroid disease. (You’ll need to stop taking a biotin supplement prior to thyroid testing because it can interfere with the accuracy of the bloodwork.)

Menopause Hair Loss 101: What Causes It and 7 Ways To Support Hair Growth
Are you experiencing hair loss, changes in texture, or an itchy scalp? Find out why this is happening and how to manage this menopuase symptom.

Menopause Acne?! Why It Happens and How To Treat Your Skin
Do you have pimples on your face or torso in your 40s and 50s? Learn why menopause acne happens and how to treat it.
Sleep
How many times have you slept consistently for 8 hours? It’s one of the most common menopause symptoms – falling asleep, staying asleep, and falling back asleep.
Hormone fluctuations can jolt you awake as well as symptoms. Perhaps you wake up in the middle of the night with night sweats, cold flashes, leg pain, or restless leg syndrome.
Falling back asleep during menopause can be harder than other stages of life due to what’s causing you to wake. The key to getting the sleep your body needs rests with your day and night habits.

Why Women+ Are Prone To Restless Leg Syndrome (RLS) And How To Treat It
Do your legs move uncontrollably at night? Learn why Restless Leg Syndrome (RLS), is more common in women and how to treat it.

Why Can’t I Sleep During The Menopause Transition? Understanding It Can Help You Sleep
Understanding why you can’t sleep during perimenopause and menopause can help you get more sleep.

The Sleep Hygiene Hack That “Tunes” Your Brain For Better Quality Sleep
Ready to “tune” your brain for better sleep? Add binaural beats to your sleep hygiene routine to improve sleeplessness during menopause.
Upper Body
Anger and Rage | Anxiety | Brain Fog | Depression | Ears | Eyes | Hair | Headaches | Mood Swings | Oral | Thyroid |
Anger and rage
During menopause, women can experience mental and emotional concerns from rage to depression and everything in between.
In addition to the hormonal fluctuations of menopause, you may be upset with your spouse, disappointed in your weight, confused by symptoms like brain fog, or lamenting on the loss of fertility. The list of contributing reasons for your emotions can go on and on!
It's been awful, and the mood swings and rage are the worst!
pausitive health survey respondent
If you’re having these emotions, it’s essential to get to the bottom of “why” you’re feeling the way you are because long-term anger and rage are bad for your health.
Are you even able to tell the difference between rage and anger or when one fuels the other?
A good starting point is the pausitive health downloadable anger log. It can help you identify your emotions and feelings, triggers, and trends.
Get Relief From Your Emotions
Having mood swings? Track how you feel, identify your triggers, and find ways to calm the emotional firestorm with this mood log.
"*" indicates required fields

Menopause Rage Is Real! How To Tame The Beast Inside
Do you feel menopause rage? Learn how to tame the beast inside and control your emotional symptoms, including anger, during menopause.

Why Anger Problems Are Bad For Your Health
Anger is yet another menopause symptom, but anger problems are bad for your health, leading to depression and other health concerns.

What Causes Anger Issues During Menopause And How To Manage It
Do you feel anger during menopause? It can make other menopause symptoms worse. Learn what causes anger issues and how to manage them.
 Anxiety
Anxiety
Are you feeling anxious? Have you always felt this way, or is it a new experience?
How long do the symptoms last? Do you continue to feel anxious long after the stressful situation passes? That’s an indicator that you could have an anxiety disorder.
According to the American Psychological Association, anxiety “is considered a future-oriented, long-acting response broadly focused on a diffuse threat…” It is characterized by “a feeling of fear, dread, and uneasiness.”
Anxiety evolves to a disorder when it persists (i.e., occurs more days than not, for at least 6 months). It may impact your work and activities of daily living. Generalized anxiety disorder (GAO) is seen in close to 6% of the adult population in the U.S. at some point in their lives and is more common in women+ than men. In some studies, it was found to be twice as common.
Like depression, the risk of anxiety increases during the menopause journey. One reason is the fall in estrogen levels. And anxiety has been noted to be more common in women+ who experience vasomotor symptoms (VSMs) – hot flashes, night sweats, and palpitations.
There are other potential causes of or contributors to anxiety, like a thyroid condition or past trauma. Therefore, as always, contact your healthcare provider to get guidance and develop a treatment plan.
Symptoms of anxiety
Look out for these symptoms:
- Being angry and on edge
- Going back to the same thought over and over
- Being worried or stressed on a regular basis
- Avoiding public or social settings
- Having panic attacks (which may include symptoms like palpitations, nausea, feeling weak or lightheaded, sweating, and having chest pain)
- Being afraid (the feeling of fear) or fearful
- Hot flashes
- Having difficulty sleeping
- Shaking
- Having tense muscles/body
- Having fatigue and exhaustion
These feelings may come and go or last longer. As you can see, many of the symptoms of anxiety are also menopause symptoms, so it may be difficult to distinguish between the two.
Managing anxiety
There are basic steps you can take, like improving your sleep routine, that will be helpful for anxiety and other menopause symptoms like mood swings. Others include watching your intake of caffeine and physical activity. Learn about treatment options for anxiety.
Some women find relief with non-hormonal treatment options like yoga and meditation, which can help you to relax your mind and body, decrease stress, and get better sleep. Some may need medication, like antidepressants. And some women+ may find cognitive behavioral therapy (CBT) an effective modality for anxiety, as well as sleep issues and hot flashes.

17 Menopausal Anxiety Treatment Options To Ease Your Mind
Feeling anxious during the menopause journey? Try these 16 anxiety treatment options to ease your mind of worry and fear.

Feeling Anxious? How Anxiety Impacts Menopausal Symptoms and Vice Versa
Are you feeling more anxious during the menopause journey? You are not alone. Learn how it can impact other menopause symptoms too.

What Is Anxiety, and Why Does It Impact More Women+ Than Men?
Are you experiencing anxiety during the menopausal transition for the first time? Learn about the types of anxiety and why it impacts more women.
I worry brain fog will prevent me from performing tasks and assuming the responsibilities that my position requires.
pausitive health survey respondent
Brain fog
Do you feel like you’re losing your mind or are your thoughts all scrambled? Brain fog can make it hard to go about your day, and can impact your personal and professional life.
In a pausitive health survey, 18% of respondents listed brain fog as one of their emotional and mental health concerns.

Clear Your Mind: 5 Potential Herbal Remedies for Menopausal Brain Fog
Menopausal “brain fog” (or menofog) is a real thing, but it doesn’t have to be the end of the road. While treatment options are lacking, herbs hold promise.
Depression
How are you feeling? Truthfully! If you’re struggling with sadness or medically diagnosed depression, you are not alone. It’s common in women, and can be one of the first symptoms of menopause.
One of the reasons is that menopause changes your brain. That’s why you may feel a wide range of emotions, almost as if you’re on an emotional rollercoaster. Learn if you’re at risk for depression.
Women are 70% more likely to suffer from depression than men.

When Perimenopause Depression Steals Your Joy: How To Recognize It And Cope
Are you feeling down? Perimenopause depression is a common symptom. Learn about the symptoms and treatment options.

Are You At Risk For Depression During The Menopause Transition?
During menopause, especially perimenopause, there’s a risk for depression. Do you have any of the 10 risks for this mental health concern?
Ear symptoms
During the menopause journey, there are also possible changes related to your ears and hearing, including:
- ringing of the ears during perimenopause (tinnitus)
- blocked ear canals
- infection
- hearing loss, especially for postmenopausal women+
- hot ears
- itchy ears
The drop in estrogen levels during the menopause transition can cause the lining of the ear canal and inner ear to dry out, impact blood flow, and affect certain cells as well as bone metabolism. As a result, you may be more prone to ear infections, dizziness and issues with balance, and itchy ears. Some women experience hot ears related to hot flashes, particularly if the hot flashes prmarily occur from the chest up.
Tinnitus, a hearing disorder which results in noise in the ear(s) that can sound like ringing, buzzing, or other sounds, may also develop related to hormonal volatility.
 Hearing loss and HT
Hearing loss and HT
You may notice a change in your hearing during this stage of life. It may be something as simple as a wax build-up related to the dryness from lower estrogen levels. However, you should check to make sure it is not something more serious, especially since hearing impairment/loss can be a risk factor for dementia.
It may not be surprising that hearing loss increases with age, but there are surprising links to age of onset of menopause and hormone therapy.
In a prospective study of 80,972 women+ published in Menopause, there wasn’t an association between menopausal status and hearing loss. But, there was an association between the age at which women+ reached menopause and HT use. The link appeared to be related to the age at which HT was started and the amount of time it was used.
- Women who experienced menopause at an older age had a higher risk of hearing loss. Women who experienced natural menopause at age 50 or older had a 10% higher chance than women who experienced it before age 50.
2. Use of oral estrogen hormone therapy or an estrogen-progestogen combination increased the risk, and the risk was greater for women+ who used HT longer.
3. The risk was also greater for women+ who used HT for 5 years or more, compared to those who did not use it.
Always talk to your doctor about hormone therapy. The latest guidelines say HT should be individualized, and you should use the lowest dose possible that is effective. There are many risks and benefits to be taken into account. In addition to timing and dose, you should also consider the type of hormone therapy and duration when discussing treatment with your doctor.
 How your eyes can change
How your eyes can change
The menopause transition can also lead to eye issues like:
- dry eyes
- light sensitivity
- blurred vision
- increased tearing
- red or swollen eyelids
- scratchy eyes
These symptoms are believed to be related to the hormonal shifts and fall in estrogen and progesterone levels that occur during the journey.
Don’t take unnecessary risks with your vision or suffer when there are steps you can take to get relief. Make time to see an eye specialist to find out if the cause of your symptoms is related to the menopause transition or potentially a sign of conditions like thyroid disease or diabetes. Regular eye exams can also detect issues like glaucoma and AMD early so treatment can begin to help protect your vision.
Menopause and glaucoma
As you age, your vision may decrease due to conditions like cataracts, and glaucoma, and age-related macular degeneration (AMD), which are more common as one gets older.
A new (2023) study suggests menopause may also increase a woman’s chance of developing glaucoma. It’s the leading cause of blindness that can’t be cured. 59% of people who develop it are female.
Now, researchers believe the changing levels of estrogen during the menopause journey cause women+ to develop glaucoma and other vision issues.
Additionally, women+ who experience early (older than 40 but younger than 45 years of age) menopause are at increased risk of open-angle glaucoma.
Some studies found postmenopausal hormone therapy can decrease the risk of secondary open-angle glaucoma and elevated pressure in the eyes, which can lead to glaucoma. Researchers believe further studies are needed to examine the relationships between medications like HT and the risk of glaucoma.
This article includes affiliate links. We may earn a small commission if you access Happy Head telehealth services and solutions. The companies we work with are carefully vetted. However, we do not guarantee their products and services.
 Hair changes
Hair changes
Have you noticed a change in your hair texture or receding hairline? Is it more dry or frizzy even though you haven’t changed your care routine? Is your hair thinning or shedding more hair than usual?
These all can be a sign you’ve started on the menopause journey.
As you might have come to expect, hormonal changes may be to blame for these symptoms. Estrogen and progesterone can help hair stay in the anagen (growing) phase of the hair life cycle. When levels fall, hair thins out and grows more slowly. At the same time, the level of androgen hormone increases, which leads to hair loss on your head but can also cause hair growth on your face/chin. It’s a potential perfect storm of hair changes resulting in a distribution that’s less than optimal.
Hair thinning and loss (alopecia) can also be caused or exacerbated by other factors like stress, anemia, a problem with your thyroid, or insufficient intake of protein, biotin, iron, or zinc. Alopecia is the sixth most common dermatologic diagnosis for African American women.
Women+ are at increased risk of depression and hypertension. Certain medications for depression and high blood pressure can also cause hair loss. So, check in with your healthcare provider to determine if you need a work-up, a referral to a dermatologist, or a change in your medication regimen.
You may also experience a dry, itchy, or sensitive scalp.
The hair changes experienced in menopause may also vary depending on your race/ethnicity and degree to which you stressed your hair over the years.
Caucasian hair
Hair is typically at its thickest between ages 42 and 53 years old for Caucasian women+, and it can thin out as estrogen levels drop during the menopause journey.
Flat irons, blow drying, coloring, and other hair treatments can damage hair. Some of that damage can lead to further graying. Depending on the number of treatments and grooming habits, one woman’s hair may be more or less susceptible to stress.
African American hair changes
African hair is more fragile and breaks earlier and at lower stress levels than Caucasian and Asian women. It also breaks faster than it grows. Compared to Asian women, the growth difference can be as much as 5-cm less in one year.
The denisty is also less than Caucasian and Asian women, and it decreases with age.
Asian hair
Asian hair is more resistant to stress from coloring and straightening, but it does become weaker with age. That’s after 40 years of age for Japanese women+ and 50 years of age for Korean women+.
Hispanic/Latino hair
A Hispanic or Latino woman has hair similar to that of an Asian woman. But, Hispanic women tend to report more heat-styling habits to achieve smooth, shiny hair. That can damage the hair, and depending on the extent of treatments and habits, damage can show up earlier than it otherwise would with natural aging.
Helping hair grow
There are steps you can take to help support your hair and scalp health. For many women+, the thinning and hair loss may eventually abate, and regrowth may occur.
- Manage emotional stress and avoid physical stress to your hair and scalp from:
- harsh chemicals
- hairstyles that put a lot of traction on the hair
- heat tools like curlers and hair straighteners
- Speak with your healthcare provider about:
- topical treatments like minoxidil, which can help some people regrow hair when used consistently
- spironolactone, an oral medication used for hypertension and other conditions, and off-label for hair loss and thinning
- Look at your eating habits.
- Are you consuming foods that ensure sufficient intake of vitamins that play a role with regard to the condition of your hair like biotin, zinc and vitamins C, B, A, and D?
- Are you experiencing heavy periods during perimenopause that may lead to an iron deficiency?
- Are you eating omega-3 fatty acids, which can be found in foods like salmon, tuna, and walnuts
- Are you eating foods packed with these nutrients so you can help make your menopause symptoms better?
Additionally, some women+ who use HT for menopausal symptoms like hot flashes and may find their hair issues improve. However, depending on the type of hormone formulation, others may find HT worsens hair and scalp changes.

Grow Your Hair Back in 3 to 6 Months!
Connect with a Happy Head board-certified dermatologist with expertise in hair restoration to develop a treatment plan for hair thinning/loss.
You will also receive a 65% discount on your first order of medication if needed to address your hair issues. Enter code “pausitive” at checkout to receive the discount.
This is an affiliate link. We may earn a small commission if you access Happy Head telehealth services and solutions. The companies we work with are carefully vetted. However, we do not guarantee their products and services.

Menopause and Hair Loss: Understand the Connection and Find the Right Solution
Learn about solutions for menopausal women experiencing thinning hair, a receding hairline, or bald patches.

Menopause Hair Loss 101: What Causes It and 7 Ways To Support Hair Growth
Are you experiencing hair loss, changes in texture, or an itchy scalp? Find out why this is happening and how to manage this menopuase symptom.
 Headaches
Headaches
Is your head throbbing? You are not alone.
Headaches are common in the general population (approximately 17% of individuals) and up to twice as prevalent in women+ than those of the male sex.
There are several types of headaches, including:
- Migraine – characterized by a throbbing pain, often severe, typically on one side of the head and commonly accompanied by symptoms like nausea, vomiting, light sensitivity and sensitivity to sound; cause believed to be abnormal brain activity which can also cause a change in blood flow
- Tension – the most common type, characterized by mild – moderate pain, and often described as a tight band around the head; cause unclear
- Cluster – an uncommon type, more prevalent in men and may run in families, characterized by one-sided head pain that can be severe and often accompanied by symptoms such as a stuffy nose or tearing of the eyes; cause unclear
In women+, headaches are often related to hormonal shifts, particularly changes in estrogen levels. Therefore, they may be present throughout the course of a woman’s life cycle, starting with menses all the way through to the menopause journey. They can also be seen in response to hormonal changes related to other factors such as a surgical procedure like a hysterectomy.
Headache is common during the menopause transition, starting in the perimenopause stage of the journey.
Migraines
Migraine headaches are among the most common type of headache during the hormonal transition.
For those with a history of migraines, there can also be a reciprocal relationship with hot flashes – women+ with migraines are more likely to have severe hot flashes, and those with severe hot flashes are more likely to have migraine flares.
Researchers have also found women+ with a history of migraine headaches had varying patterns when the menopause journey was underway. 24% saw their headaches get worse, 36% got better, and 40% experienced no change during the menopause transition.
Some 25 – 30% of migraine sufferers experience an “aura,” which can be a signal a migraine is on its way. During an aura, which can last up to an hour, an individual may experience a tingling or numb sensation of various parts of the body, seeing zig zags, sparks, and bright dots, or being unable to speak clearly. Visual changes are the most common type of aura.
Women+ going through the menopause journey are already at an increased risk of coronary heart disease. Unfortunately, a recent study found an association (currently unexplained) between migraine with aura and an increased risk of cardiovascular disease.
Besides hormonal changes, there are many other potential triggers for a migraine:
- Certain foods and fluids – chocolate, those containing tyramine (e.g., wine, aged cheese, chicken livers smoked fish, figs, and certain beans), meats containing nitrates (e.g., bacon, hot dogs, cured meats), fermented, processed, pickled, and marinated foods, foods containing MSG, onions, peanuts, avocado, citrus fruit, bananas, alcohol
- Caffeine withdrawal
- Missing meals
- Not getting enough sleep
- Loud noises and bright lights
- Perfume
- Smoking or being exposed to smoke
- Stress/anxiety
Headaches and health disparities
Like so many other areas of medicine, health disparities exist when it comes to headaches. Both Black women and Latinas are less likely to get a migraine diagnosis than their white counterparts, which also means greater risk of delayed or even no migraine-specific treatment altogether.
Some studies have also found health disparities in the queer community compared to cisgender heterosexual individuals. For those who are transgender, there are the additional potential challenges of the applicable hormonal regimen, its impact on headaches, and finding a provider who is knowledgeable. And, related to a greater prevalence of anxiety and depression, LGBTQIA+ members are at additional greater risk for coronary heart disease beyond hormonal shift and migraines with aura.
Be mindful of the intensity of those headaches as they can become migraines. A severe headache is one symptom of a migraine. It may be accompanied by nausea, blurry vision, dizziness, light sensitivity, and fatigue.
The researchers said migraine and tension-type headaches are the most common types of headaches during menopause.
Migraine help
As you can tell from the trigger list, there are many lifestyle changes you can make to help manage migraines, several of which may also help with other menopausal symptoms like hot flashes, fatigue, and weight gain – healthy eating, reducing or eliminating alcohol use, and getting enough high-quality sleep.
There are many additional options you can try for migraines, both hormonal and non-hormonal, including:
- over-the-counter NSAID pain medication
- acupuncture
- mind-body therapies that relieve stress and tension, including mindfulness-based stress reduction (MBSR)
- black cohosh
- vitamin E
- exercise (to help relieve stress and anxiety; but avoid exercising during an attack, as it may make symptoms worse)
- yoga
- antidepressants like venlafaxine, paroxetine, and escitalopram
- anti-seizure medicine like gabapentin
- transdermal hormone therapy may also be an option, although talk to your doctor about the risks and benefits of using HT
- migraine-specific medications, both those used to prevent a migraine and those taken to abort an acute attack
Many of these treatment options can also help with other menopause symptoms.
As always, seek guidance from your healthcare provider to identify the best regimen for your particular situation, as well as to learn about the risks, benefits, and various formulations of HT.
Mood swings
In a pausitive health survey, mood swings were the top emotional and mental health concern, affecting 22% of respondents.
Some women compare the up-and-down range of emotions to being on a rollercoaster.
Know that you are not alone, and you don’t have to suffer in silence. There are treatment options available and steps you can take to adjust your mindset, to find the positives of this ride through life!
It is difficult to think of anything positive about this time of life.
pausitive health survey respondent

Missing Your Life Before Menopause? How to Manage The Grief and Loss
Do you ever think about life before menopausal symptoms? If you feel a sense of loss or grief, try these emotional coping strategies.
Oral health
Your oral health is important throughout your life and can impact many other parts of the body. For example, periodontal (gum) disease can cause inflammation in the body that can increase the risk of cardiovascular disease, make diabetes more difficult to manage, and result in premature delivery.
This stage of life is no different, as both the gums and teeth can be affected.
During the menopause journey, the hormonal changes can increase the risk of plaque, which in turn increases the risk for gingivitis (gum inflammation) and advanced periodontitis (gum infection).
Women+ can also experience:
- dry mouth (xerostomia)
- metallic taste
- mouth pain and burning tongue (Burning Mouth Syndrome aka BMS)
- receding gums
- tooth decay
- tooth sensitivity
- loose teeth/losing teeth
- TMJ

Periodontal issues are the most common sign of the impact of the menopause transition on oral health, present up to 60% of the time, followed by dry mouth (25%), and burning tongue (15%) of the time.
Dry mouth is more than an inconvenience. Saliva plays an important role in clearing bacteria from your teeth, so a reduction in saliva increases the risk of cavities, gum recession (which can lead to tooth loss), thrush (oral yeast), a bad taste in the mouth, and issues with the jaws.
Burning mouth syndrome (BMS)
Just like it sounds, BMS can affect all parts of the mouth, including the tongue, palate, lips, or areas that support dentures.
It affects mostly women+ in their 40s and 50s but is most common in postmenopausal women.
TMJ jaw pain
Some of your menopausal muscle aches and pains may be in a jaw joint, commonly referred to as TMJ or the temporomandibular joint.
You can feel these joints on either side of your face just below your ears. Open and close your mouth, and you’ll feel the joint at work.
TMJ can cause:
- pain in the jaw
- chewing pain
- pain opening and closing your mouth
- popping noises in your ears
- clicking or popping noise in your jaw
- headaches
- neck pain
Pain in this joint that lasts more than six months can lead to a degenerative disease known as chronic TMD. So, it’s important to tell your dentist if you’re experiencing pain.
One study has reported that women with severe menopausal symptoms also experienced more severe TMJ pain. And another study also found it’s more common in menopausal women than in non-menopausal women.
It’s less clear during which stage of menopause you’re most at risk for TMJ pain, as studies have shown conflicting findings.
Preventing oral health symptoms related to menopause
The risk of several oral health issues during the menopause journey may be reduced by good oral hygiene. Steps you can take include:
- Brushing your teeth at least twice a day for at least two minutes with fluoride toothpaste.
- Flossing at least once a day.
- Reducing the consumption of sugar and eliminating sugary food and drinks.
- Using a fluoride rinse once a day.
- Eliminating tobacco products.
- Using xylitol toothpaste, gum, or candy, which can help prevent cavities.
- Seeing a dentist for a check-up at a frequency based on your particular situation; for example, you might be prescribed a special rinse for dry mouth or toothpaste with a higher concentration of fluoride.
Additionally, according to the American Dental Association (ADA), “Systematic reviews found that mouth rinses containing an antimicrobial effective amount of a fixed combination of four essential oils (eucalyptol, menthol, methyl salicylate, and thymol) or cetylpyridinium chloride, and toothpastes containing triclosan or stannous fluoride, were associated with decreased risk of gingivitis and periodontal disease.”
Treatment
For oral health issues, studies present a mixed bag. Hormone therapy has proven effective in some, but others have not shown marked improvement.
HT can increase bone density, and some studies have found postmenopausal women on HT for osteoporosis prevention had a lower prevalence of severe periodontitis, and tooth loss.
When it comes to TMD, the American Academy of Orofacial Pain (AAOP) says treatment depends on the cause, of which there are many.
Stress management, physical therapy, medication, a night guard to prevent clenching or grinding which can worsen TMJ, or a stabilization splint can help.
In most cases, conservative treatments work. Surgery is only required in 5 out of 100 cases, according to AAOP.
Your dentist can help address your TMJ symptoms, or you might be referred to an orofacial pain specialist.
 Thyroid
Thyroid
One in eight women+ will develop an issue with the thyroid over a lifetime. And hypothyroidism (underactive thyroid) was found to be more common in Korean women in later perimenopause and during the post-menopause stage of the journey than in earlier stages of their lives.
As is often the case, many of the symptoms of the menopause journey overlap with those of various conditions. Thyroid disorders are no exception. Both overactive (hyperthyroidism) and underactive (hypothyroidism) thyroid function changes can lead to symptoms commonly experienced by menopausal women+ – palpitations, weight gain, hair changes, fatigue, GI symptoms, mood changes, sleep issues, and menstrual irregularities.
For example, your thyroid helps regulate your metabolism. As you age, your metabolism naturally slows. So, if you gain weight, is it your metabolism slowing or is it your thyroid? Both? It can be difficult to tell the root cause without further testing.
Thyroid conditions can also increase the risk of certain conditions for which women going through the hormone transition are already at increased risk – heart disease, high cholesterol, depression, and osteoporosis. And if you already have hypothyroidism and are taking levothyroxine, a dosage reduction may be needed. However, if you are on hormone therapy for menopause symptoms, the dosage may need to be increased.
Thyroid issues can also make menopause symptoms worse.
Your doctor can check your thyroid for changes in the size and feel for nodules during an exam. It’s also likely bloodwork would be ordered to check your thyroid hormone levels.
Torso
Heart palpitations
In addition to an overall increased cardiovascular risk, women+ may also experience palpitations. They’re most common in perimenopause but they can also occur in postmenopausal women+. Up to 42% of perimenopausal women and 54% of postmenopausal women have palpitations.Symptoms may vary among women+. You may describe it as:
- an irregular heartbeat
- fast heartrate
- fluttering
- pulsating
- racing
- pounding
Risk factors for palpitations
Like other menopause symptoms that vary by race and ethnicity, there are differences with palpitations too. Hispanic women are more likely than white women+ to have palpitations. Cardiovascular disease risk factors are also higher in Hispanic individuals. Palpitations are also seen more commonly in women+ who are inactive, have sleep disturbances, and hot flashes.By managing some of the other correlated symptoms, you may also be able to manage a racing heart.
When your heart is involved, always talk to your doctor, as it can be a sign of a more serious heart condition.Cardiovascular concerns for women+
Cardiovascular disease is the leading cause of death in women+ in the United States. While it can strike at any time, the risk increases as a woman+ transitions through the stages of menopause.
It’s critical that you seek the advice of a doctor and get help immediately at any sign of heart distress. Research shows that while it’s a leading cause of death, only 56% of women recognize it as the #1 killer.
Women may have different signs than men, including:
- nausea
- vomiting
- fatigue that won’t go away
They may also feel:
- dull or heavy chest
- pain in the neck, jaw, or throat
- pain in the back or upper abdomen
Risk factors for women+
Risk factors include overall lifestyle, the timing of menstruation and menopause, and your health during pregnancy. You’re at risk if you had/have:
- period before age 11
- early menopause (before age 40)
- polycystic ovary syndrome
- gestational diabetes during pregnancy
- preterm delivery
- delivery of a low birth or high birth-weight baby
- hypertensive disorders of pregnancy
Reducing the risk of heart disease
To reduce the risk of heart disease:- watch your weight
- exercise
- eat healthy foods
- find ways to decompress after a long day
- minimize stress
- limit alcohol
- monitor your cholesterol
- monitor your blood pressure
- check you triglycerides


18 Cardiovascular Risk Factors Menopausal Women Need To Know
Cardiovascular disease (CVD) is the #1 killer in women. Learn 18 cardiovascular risk factors menopausal women need to know.

How Menopause Impacts Heart Health: 7 Action Steps That Help
Heart health lifestyle habits can help you manage menopause symptoms and help reduce the risk of cardiovascular disease.
Gastrointestinal pain
During menopause, you may increase a wide range of gastrointestinal pain including:
- gas
- indigestion
- abdominal cramps
- bloated
- changing bowel habits
- heartburn and acid reflux
- constipation
- nausea
- vomiting
- diarrhea
You can also get gallstones and pancreatitis. For some women+, the symptoms can also indicate gastrointestinal diseases like irritable bowel syndrome.
It’s critical that you talk to your doctor about many of these symptoms as they can be a sign of other, more serious conditions like colon cancer or ovarian cancer.
Learn about the various stomach diseases that affect menopausal women and the ways to treat gastrointestinal concerns and stomach pain.

Menopause Bloating and Constipation? Don’t Suffer From GI Pain Any More
Does your stomach hurt or feel bloated? Menopause GI pain can cause several symptoms in your gastrointestinal tract. Learn how to manage them.
Non-alcoholic fatty liver disease (NAFLD)
Your liver is also part of the GI tract, but it’s unlikely you’ve given as much thought to it. New research suggests postmenopausal women are at risk for non-alcoholic fatty liver disease (NAFLD).
NAFLD refers to several liver diseases that affect people who drink little to no alcohol. With this disease, there’s too much fat in the liver cells.
In a review of 12 cross-sectional studies, researchers found the risk of getting non-alcoholic fatty liver disease (NAFLD) increases nearly 2.4 times in postmenopause. Plus, the mortality rate is higher for women.
Symptoms of NAFLD
You may not have many symptoms with NAFLD. If you do have signs of it, you may struggle with fatigue or pain in the upper abdomen.
More advanced cases of this disease have more pain and symptoms like yellowing of the skin and eyes.
Age and hormonal fluctuations increase the risk of liver disease in postmenopausal women enough that researchers say there should be a heightened sense of suspicion of this so you can get treatment early before the disease becomes advanced.
Shortness of breath
However, shortness of breath can also be a sign of a serious lung condition, so talk to your doctor if you’re having shortness of breath.
It's as if menopausal women+ smoked 20 cigarettes a day for 10 years.
That's how much lung function decreases, according to researchers in Norway.
Lower Body
Leg pain
Pain during the menopause journey can be generalized muscle aches and joint pain or specific to a part of the body like the leg.
When the pain is specific to the leg, women+ complain of:
- cramps
- restless legs
- achiness
- swelling
- tingliness
- pain near the hip
- hot and cold feet

Restless Leg Syndrome (RLS)
When the pain causes you to move your legs uncontrollably while you rest, you may have Willis-Ekbom disease, also known as Restless Leg Syndrome (RLS).
In addition to the leg movements, you may have a pins and needles feeling in your legs or pain between the ankle and knee.
There are specific criteria used to diagnose RLS, which is more common in women than men. Some of the changes women+ experience during the menopause journey can increase the chance of getting RLS.

Best Foods To Eat To Manage Restless Leg Syndrome (RLS)
Food as medicine. Get a list of the best foods to eat to manage restless leg syndrome (RLS) and avoid triggering it.

Why Women+ Are Prone To Restless Leg Syndrome (RLS) And How To Treat It
Do your legs move uncontrollably at night? Learn why Restless Leg Syndrome (RLS), is more common in women and how to treat it.

Having Leg Pain And Cramps? You May Be In Menopause
Do you have leg pain and cramps, during the day or at night? It’s a menopause symptom. Learn how to treat the leg pain.
 Loss of libido
Loss of libido
If you’re having vaginal pain, you may not be interested in sex because it’s painful or causes you to not orgasm. Unrelated to that pain, fluctuating hormones during the menopause journey can also result in a loss of libido or sex drive.
Women+ may also find it harder to be aroused by their partner, impacting their relationship and mood.
Other menopause symptoms like urinary incontinence can also cause you to lose your sex drive. If you’ve gained weight or experiencing mood swings, you may feel less sexy and find it hard to get in the mood.
The status of your relationship with your partner in midlife can be a factor. Talk to your partner about how you feel. Open communication will help you manage this symptom of menopause.
Loss of libido is a complex issue in midlife that’s likely hormonal, physical, and emotional. While your doctor can prescribe medication to increase sex drive, you also need to address this symptom’s emotional and physical components.
If you experience this, it may happen to be your only sexual symptom or there can be others. It can also happen in combination with other sexual, urinary, and genital symptoms and may be referred to as genitourinary syndrome of menopause.

Reignite Passion: How To Manage Genitourinary Syndrome Of Menopause (GSM)
Are you experiencing vaginal dryness, no orgasm, or painful sex? If you wait or don’t have sex, it can get worse. Try these menopause treatments.
 Pins and needles in hands and feet
Pins and needles in hands and feet
Do your hands and feet tingle so intensely that it feels like pins and needles? These sensations can happen throughout a woman’s body, but typically on the arms (hands, fingers), feet (toes), and skin.
It’s called paresthesia. It can make it difficult to walk or grab things, and can cause you to lose your balance.
Women+ describe this sensation as:
- pins and needles
- tingling
- prickly
- a sensation of something crawling on you
- burning
- numbness
- cold sensation
- increased sensitivity
- electric shock
It’s all related to how menopause changes your body – from head to toe – including the nervous system.
Pay attention to the pins and needles sensation in combination with other symptoms. Does it make your anxiety or mood swings worse? Does it bring about a cold or hot flash?
How to manage tingling sensations
Like so many other symptoms, lifestyle modifications are a great way to manage this menopause symptom.
You can:
- Eat foods rich in vitamins you need for menopause, especially B12. You can also take a supplement, but talk to your doctor about this to avoid contraindications with medications or other supplements.
- Exercise regularly to keep your blood moving and muscles and joints flexible.
- Watch your caffeine and alcohol intake, as they can dehydrate you.
- You can also try non-hormonal techniques that relieve stress like mind-body remedies, massage, and acupuncture.
Urinary incontinence
Does urine randomly leak from your bladder? This uncontrolled leakage is considered urinary incontinence. It may happen when you’re exercising, coughing, sneezing, or laughing.
If you’ve been pregnant, you may blame it on that. Just like during that time of your life when your doctor perhaps told you to do Kegel exercises, the same advice holds during the menopause journey.
Urinary incontinence can be due to an overactive bladder and/or weak pelvic floor muscles, which Kegels strengthen. There are also other treatment options to manage pelvic floor dysfunction.
Urinary GSM symptoms
Urinary incontinence is just one of the urinary symptoms of genitourinary syndrome of menopause (GSM). Others include:
- painful urination
- urgency (need to go to the bathroom quickly)
- blood in the urine
- more frequent UTIs
- stress/urgency incontinence
Any of these urinary symptoms can appear on their own or in combination with sexual and vaginal symptoms. That’s why it’s referred to as genitourinary syndrome of menopause (GSM).
Managing urinary symptoms
Urinary symptoms can impact daily life and your sex drive, if you have leakage during sex.
So talk to your doctor about it before it affects your relationship too.
If you have urinary incontinence, you can manage it by:
- Watching your weight, as this is a risk factor.
- Limiting caffeine, alcohol, or drinks with gas.
- Monitoring for activities that make symptoms worse.
- Trying bladder training which means going to the bathroom less and exercises to control your urine stream.
- Doing pelvic floor exercises like Kegel exercises.
- Using a professional pelvic floor therapist who can use other techniques.
- Having surgery as a last resort.
If you have urinary leakage or have to go to the bathroom too much, you can:
- Try Kegel exercises on your own or with a physical therapist.
- Schedule trips to the bathroom.
- Use panty liners or pads.
- Practice bladder training.
- Ask your doctor about percutaneous tibial nerve stimulation (PTNS).
- Talk to your doctor about nerve stimulation.

Is Your Pelvic Floor in Perimenopause Too?
Give your pelvic health some love in perimenopause. It’s more than Kegels. Get solutions to improve vaginal and sexual health, your bladder, and pelvic floor.

Pelvic Floor Rehab: 10 Treatment Options During the Menopause Journey
Pelvic floor symptoms can be embarrasing, but don’t have to be. Learn about pelvic floor rehab options. Get treatment that’s right for you.

Menopause Matters: Understanding Pelvic Floor (Bladder and Bowel) Symptoms
Your pelvic floor is the “forgotten core” but your body may remind you of this area during the menopause journey, with bladder and bowel symptoms.
 Urinary tract infection (UTI)
Urinary tract infection (UTI)
Urinary tract infections are common in postmenopausal women. It’s a bacterial infection and can also be associated with genitourinary syndrome (GSM) of menopause.
They’re recurrent when you have three UTIs in 12 months or two in six months.
The most likely symptom is a burning pain when you go to the bathroom and urinate. It may also feel like you have to use the restroom but only produce a few drops of urine. Your urine may also have an odor or look cloudy.
You may also feel pain in your lower abdomen, pelvic area, and even your lower back.
If you notice blood in your urine, seek the help of a doctor immediately. This can be a sign of a more serious condition.
Why menopausal women get UTIs
The microbiome of the urinary tract changes during the menopause journey, which can make women+ prone to UTIs. Also, vaginal tissues thin, and trouble emptying your bladder during the menopause journey can also contribute.
UTI treatment
While antibiotics can help, you don’t want to take those frequently to minimize drug resistance. Topical and intravaginal estrogen can help reduce the risk.
You can also try probiotics, cranberry juice, and d-mannose. Your doctor may also suggest an oral immunostimulant or filling your bladder with a solution and then draining it in a procedure known as a bladder instillation.
When you have to go to the bathroom, go! Take your time urinating.
Research also shows women+ have success with an oral combination of hyaluronic acid, chondroitin sulfate, curcumin and quercetin while using estrogen therapy.
Researchers are also working on a promising bladder vaccine that helps your bladder fight off the E-coli bacteria.
Vaginal pain
During menopause, your vagina tissues change. It can lead to:
- frequent urinary tract infections
- pain during sex
- vaginal dryness
- vaginal itching
- lack of an orgasm
The pain and symptoms can involve your vagina, vulva, and urinary tract.
Due to the number of body parts involved in this region, you may hear your doctor refer to it as genitourinary syndrome of menopause or GSM. Depending on the specific symptoms, there are other names, like vaginal atrophy.
Don’t be embarrassed to tell your doctor about sexual issues like pain or orgasm issues. The key is to get treatment quickly before the vaginal or sexual pain gets worse.

Reignite Passion: How To Manage Genitourinary Syndrome Of Menopause (GSM)
Are you experiencing vaginal dryness, no orgasm, or painful sex? If you wait or don’t have sex, it can get worse. Try these menopause treatments.
Treating GSM
Depending on where the pain is located, treatment may vary. You have options to help with the pain and lack of an orgasm including:
- HT
- non-hormonal medication
- pelvic floor and Kegel exercises
- vaginal stretching
- dilators
- moisturizer
What to look for in a vaginal lubricant or moisturizer
Lubricants and moisturizers will become your best friend if you’re experiencing this pain or itching in your vagina.
Do not use petroleum jelly or mineral oil as they can make the symptoms worse.
Look for a long-acting vaginal moisturizer that you can apply inside the vagina. The word “internal” is important on the label. You don’t want to apply an external product.
Weight gain
The average woman gains 4.5 pounds during the menopause transition and then another pound each year as the woman ages in her/their 50s and 60s.
In our pausitive health survey, women told us they want to lose weight, but they feel alone on their journey to do this.
Women said weight gain was the most difficult symptom to manage. With you in mind, we created the menopause shopping list to help you pick foods that will provide the right combination of vitamins and nutrients menopausal women need.
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
"*" indicates required fields
If you don’t feel good about your body weight, it can affect other physical, emotional, and sexual aspects of your daily life.
- Your mental health can suffer.
- Your relationship with your partner can be affected.
- Your sex drive can decrease.
- You may feel more aches and pains.
Losing weight can improve your mood and make menopause symptoms better, including hot flashes and night sweats.
Ready to get started?

Weight Gain in Menopause Have You Down? Try These 9 Lifestyle Changes
Have you noticed your clothes getting tighter as you age? Weight gain is common in menopause. Learn how to lose weight and feel better.

Menopause Exercise Videos To Improve How You Feel
Try these menopause exercise videos to improve how you feel. They can help with weight loss, body strength, and flexibility.

How Exercise Can Positively Change Your Menopause Journey
Exercise is a secret weapon for menopausal women. It can help symptoms, lower risks of some conditions, help with weight, muscle tone, and strength.
LePillouer-Prost, A., Kerob, D., Nielsen, M., Taieb, C. and Maitrot Mantelet, L. (2020), Skin and menopause: women’s point of view. J Eur Acad Dermatol Venereol, 34: e267-e269. https://doi.org/10.1111/jdv.16242
European Journal of Obstetrics & Gynecology and Reproductive Biology, Volume 207, 2016, Pages 125-128,
ISSN 0301-2115, https://doi.org/10.1016/j.ejogrb.2016.10.018.
