95% of women... would try hormone alternatives before HT.
Source: Women’s Health Concern
Non-Hormonal Options 101
How are you managing your menopause symptoms? You have choices, both hormonal and non-hormonal.
It’s your body, and you have the power to select (in consultation with your healthcare provider) the option(s) that’s best for your situation. Some women can’t use HT or don’t want to. Others want to know about the options they can add.
There are many possibilities, both hormonal and non-hormonal. For example, there are different forms of hormone therapy. And non-hormonal options include “food as medicine”, mind-body therapies, hormone-free prescription medication, herbal remedies, and lifestyle modifications.
Let’s explore 36 non-hormonal treatment options that can help women+ manage menopause symptoms.

Finding hormone alternatives
While women+ say these non-hormonal treatments help, studies show most women don’t tell their doctor they’re thinking about alternatives to hormones. They seek individual providers like a naturopath, herbalist, acupuncturist, massage therapist, or chiropractor/osteopath on their own and “self-prescribe” therapies.
Being open and transparent about what you are doing to improve your health and well-being with your medical practitioners is important.
For example, vitamin supplements like biotin can impact thyroid blood test results which are used to make decisions about your treatment. And not revealing the side effects of medications you are taking, or that you’re not taking them at all can delay finding something that works for you and managing your condition effectively.
Consult an expert to maximize the efficacy and safety of your approach. You have options, but not every option is appropriate for everyone, e.g., taking St. John’s Wort to treat depression while on an antidepressant to treat hot flashes.
You have choices
pausitive health believes women+ should have choices as they “make a change for the better” and that includes an understanding of all treatment options of which we are aware and show potential positive impact.
In 2023, The Menopause Society (formerly the North American Menopause Society or NAMS) released the Non-Hormonal Therapy Position Statement.
pausitive health respects and appreciates the academic review they performed and the position statement, which provides guidance for women+ and their practitioners. We know the nature of research is such that there may be treatments that prove effective for which studies may never be conducted and others that have been studied but not to the standards used by The Menopause Society.
We believe there are modalities for which there are studies which indicate positive impacts on menopausal symptoms and/or one’s physical and mental health and well-being, which in turn have a positive impact on the menopause journey. Therefore, you will find information about a broad range of non-hormonal options in pausitive health content, some of which may not align with the position statement.
As always, it is essential to discuss with your health practitioner options which are a fit for your unique needs and that take into account your current clinical status, past and family history, medications you may be taking, etc., to determine the best options for your specific circumstance and to make an informed decision.
Select a hormone alternative, and we’ll show you the data so you can make a change for the better that’s a good fit for you!
Before you try these options, talk with your healthcare practitioner. There is a risk of potential injury, side effects, or an adverse event when you start a new routine, if you have an underlying chronic condition, or are on certain medications. Always ask your doctor for guidance about the best option, as some might not be a good option depending on your personal health status.
Non-Hormonal Prescription Medication
VEOZAH™
The medication, VEOZAH™ (fezolinetant) is a first-of-its-kind treatment for moderate to severe hot flashes. It’s the first non-hormonal nuerokinin 3 (NK3) receptor antagonist to receive approval from the Food and Drug Administration.
It’s a new non-hormonal treatment that targets the cause of hot flashes, by targeting the area of the brain responsible for thermoregulation.
In clinical studies, VEOZAH™ reduced hot flashes by about 60% after 12 weeks of use and also led to less severe hot flashes and improved quality of sleep.
This medication can cause liver issues, and your doctor will require baseline bloodwork before taking the medication and at specific follow-up intervals.
Antidepressants
Paroxetine (Brisdelle®) was the first non-hormonal Food and Drug Administration-approved treatment for moderate to severe vasomotor symptoms (hot flashes, night sweats, and palpitations). It is an antidepressant known as an SSRI.
Women+ also use other antidepressants (SSRIs and SNRIs/SSRIs) off-label for hot flashes, including citalopram (Celexa), Sertraline (Zoloft), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil), duloxetine (Cymbalta), venlafaxine HCI (EFFEXOR XR®), and desvenlafaxine (Pristiq).
The manufacturer of Brisdelle® reports a reduction in hot flashes by up to 64%, and improvement in sleep.
In a small study of 80 postmenopausal women, extended-release venlafaxine also led to a reduction in hot flashes and an improvement in quality of life. Side effects in that study included dry mouth, sleeplessness, and decreased appetite.
Additional Effexor XR® (venlafaxine) side effects can occur, including nausea, dizziness, constipation, sexual dysfunction, and increased blood pressure, among other symptoms.
Overall, antidepressants such as SSRIs and SNRIs can reduce hot flash intensity and frequency by between 20 and 65%. In general, the off-label use of SSRIs and SNRIs can decrease symptoms in as few as two weeks.
Talk to your doctor before using antidepressants for menopause symptoms
Paroxetine is the only FDA-approved drug at this time, so always talk to your doctor.
Also, some of these antidepressants are first-line, and others are second-line options for hot flashes. And depending on any underlying conditions you may have, one medication may be preferable over others.
Antidepressants can also increase the risk of suicidal thoughts, so you should exercise caution and work with a healthcare practitioner.
Remember, if your OB/GYN or internist is not on board with using antidepressants to help your hot flashes, you may want to get a second opinion from a menopause-certified doctor.
 Gabapentin
Gabapentin
Gabapentin (Neurontin), an anti-seizure medication, has been found to be moderately effective for hot flashes.
In a review of seven randomized controlled trials, Gabapentin was studied as a postmenopausal alternative for women who wanted another option or had a contraindication to hormone therapy.
Side effects include drowsiness, dizziness, and unsteadiness which can occur in up to 50% of postmenopausal women. You can also suffer from withdrawal, and some people may even have suicidal thoughts or behaviors.
Lyrica
Pregabalin (Lyrica) is another anti-seizure medication that has also been found to be helpful in addressing hot flashes. Potential side effects include dizziness, drowsiness, difficulty concentrating, and weight gain.
Clonidine
Clonidine is a high blood pressure medication that may help with hot flashes and night sweats.
It can cause side effects like dry mouth, drowsiness, depression, and constipation.
INTRAROSA®
Is sex painful for you? It’s a common post-menopause symptom in up to half of all women. It’s typically caused by a condition called vulvar and vaginal atrophy (VVA), which results in dryness that can lead to pain during intercourse.
INTRAROSA® vaginal inserts treat moderate to severe sexual pain.
In clinical trials, women experienced a reduction in moderate to severe pain during sex when used for twelve weeks at bedtime.
It’s non-hormonal, made from a plant-derived form of DHEA, which your body naturally produces from the adrenal glands. Like DHEA, your body converts the substance into other hormones, including testosterone and estrogens.
Side effects include vaginal discharge and PAP smear changes.
Risks of vaginal inserts
If you have vaginal bleeding that has not been checked by your healthcare provider, it is critical to share this information to determine if the bleeding necessitates a work-up and if the inserts should not be used.
Since the inserted ingredients become estrogen in your body, it’s also important to tell your doctor if you’ve had, have, or think you may have breast cancer.

Reignite Passion: How To Manage Genitourinary Syndrome Of Menopause (GSM)
Are you experiencing vaginal dryness, no orgasm, or painful sex? If you wait or don’t have sex, it can get worse. Try these menopause treatments.
Oxybutynin
Oxybutynin (Ditropan XL) is most commonly used to treat urinary conditions like overactive bladder, but in some women it can also help with hot flashes. It comes both as a pill and a patch.
Side effects can include dry mouth and/or dry eyes, nausea, constipation, and dizziness.
So, there are prescription drugs other than hormones that can help menopause symptoms. Always consult with your doctor about the benefits and risks of each medication.

This article includes affiliate links. We may earn a small commission if you access Happy Head telehealth services and solutions. The companies we work with are carefully vetted. However, we do not guarantee their products and services.
Hair loss medication
There are several prescription medications for hair loss, a common menopausal symptom.
While some of the medications available to address hair loss/thinning may impact hormonal pathways, they are not hormone therapy themselves.
Medications include:
- Dutasteride
- Minoxidil
- Spironolactone
- SuperCapsule®
- Finasteride
Some women+ who are on hormone therapy for other menopausal symptoms like hot flashes and night sweats may experience benefits to hair changes as well. However, hormone therapy would not be prescribed as a standalone hair loss/thinning treatment. It would simply be a lucky side effect.
Explore your non-hormonal hair loss/hair thinning solutions.

Grow Your Hair Back in 3 to 6 Months!
Connect with a Happy Head board-certified dermatologist with expertise in hair restoration to develop a treatment plan for hair thinning/loss.
You will also receive a 65% discount on your first order of medication if needed to address your hair issues. Enter code “pausitive” at checkout to receive the discount.
This is an affiliate link. We may earn a small commission if you access Happy Head telehealth services and solutions. The companies we work with are carefully vetted. However, we do not guarantee their products and services.
Alternative Approaches
Herbal medicine
Herbal medicine is the study and practice of the medicinal and therapeutic use of plants.
Some of the popular herbs used for symptoms of menopause like hot flashes, sleeplessness, and anxiety include:
- Black cohosh
- John’s wort
- Evening primrose oil
- Vitex agnus-castus
- Hops
- Valerian
- Sage
- Red clover
- Dong Quai
- Ginseng
- Kava
Herbs can also help with brain fog.
Learn about each herb’s benefits, side effects, and risks in the pausitive health herbal guide, which details the latest research.
Herb side effects
Just like medications produced by drug companies, there may be risks and side effects. Herbs may not be safe depending on your clinical status or the medication you may be taking.
They can interact with other medications, and some have serious side effects. For example, there’s the potential for liver damage with black cohosh, which led to the requirement for a warning label on black cohosh products in Australia. And European regulatory agencies suggest a timeframe of less than six months.
Finding an herbalist
According to the American Herbalists Guild, there is currently no licensing or certification for herbalists in any state that precludes the rights of anyone to use, dispense, or recommend herbs, except in states where it is linked with acupuncture.
Always consult with your healthcare practitioner or a trained herbal medicine professional before trying this option.
During a pausitive health webinar, clinical herbalist, Kay Sidahmed, PhD, MS, talked about how herbal support strategies can help with your menopausal journey.

Clear Your Mind: 5 Potential Herbal Remedies for Menopausal Brain Fog
Menopausal “brain fog” (or menofog) is a real thing, but it doesn’t have to be the end of the road. While treatment options are lacking, herbs hold promise.

Which Herbal Remedies Offer Relief From Hot Flashes And Other Menopause Symptoms?
Can herbal remedies help menopause symptoms like hot flashes? Get the latest science, risks, and reported health benefits.
 Pollen Extracts
Pollen Extracts
More than 30% of women use plant products to manage symptoms. One of them is pollens from bees or flowers.
A study in Poland found promising results with a product similar to Femelis Meno, which is flower pollen and pistil (PI 82-GC FEM) extracts along with vitamin E for perimenopausal and postmenopausal women+ who had hot flashes and other vasomotor symptoms.
These were the results:
- Hot flashes improved by more than 60% on average.
- 93% of the women were satisfied or very satisfied with the treatment option.
- Nearly all the women+ (97.5%) said they were willing to continue the therapy after the follow-up period in this study.
In another study, researchers tested a product called Femal. It’s an herbal remedy made with pollen extracts. In the small trial, the women+ also experienced a drop in hot flashes and other quality-of-life factors that can be impacted during the menopause journey.
How flower pollen works
The use of flower pollens dates back to ancient Egypt and China.
The flower pollen is thought to work like SSRIs, which can also be used to manage menopause symptoms. The pollen regulates brain functions that control mood, sleep, and the body’s heat regulation.
Since the pollen extract is non-hormonal and is thought to have no effect on hormones, researchers are looking at whether it’s an effective treatment for women with hormone-sensitive cancers.
Femelis Meno® was first introduced in Sweden in 1995 and has other names in countries around the world.
If you’re looking for a similar product, the main extract is PI 82 which comes from the pollen of:
- Grass – Secale cereal
- Grass – Dactylis glomerata
- Tree – Pinus silvestris
The other active compound is GC FEM. That’s an extract from the pollen of:
- Grass – Secale cereal
- Cereal grain – Zea mays
- Tree – Pinus silvestris
In the United States, Relizen® is a pollen supplement made from four Swedish plants. It may take several months to work.
Allergens are typically removed in flower pollen products, so women+ with allergies can try the product. But always contact your doctor or allergist first, especially if you have an allergy to pollen.
Bee pollen
Like flower pollen, bee pollen can also effectively treat menopause symptoms. It also has other health benefits aside from menopause since it’s full of amino acids, healthy fats, vitamins, and minerals.
In Germany, the Federal Ministry of Health classifies bee pollen as a medicine because it can positively impact an individual’s health.
In a study of Egyptian women+, women+ received conventional clover honey or clover honey enriched with bee pollen, royal jelly, and bee gum.
In the study, women+ who took the enriched honey saw hot flashes and night sweats disappear along with body pain, sleep disruption, and psychological symptoms like irritability, anxiety, and depression.
Cancer patients on antihormonal treatments
Bee pollen is also being studied for use in breast cancer patients. A study examined whether bee pollen can help menopause symptoms in women+ receiving tamoxifen and antihormonal treatment.
Patients were given a pollen-honey mixture in the small study or a placebo of just honey. Interestingly, there was not a significant distinction between the two groups. 70.9% of the women+ taking pollen saw improvements in menopause symptoms and 68.3% of the honey patients also saw improvements.
So, researchers believe honey and bee pollen can both improve menopausal symptoms for breast cancer patients on antihormonal treatments.
Unlike flower pollen and pistil extracts, bee pollen may not be suitable for individuals with allergies.
Bee safety concerns
There is some concern that harvesting pollen for humans can affect the bee colony over time and cause it to die. Researchers are looking at more sustainable ways to gather bee pollen.
CBD
Perhaps you’ve seen regulated medical cannabis stores in your community or cannabidiol (CBD) products in retail stores offering to help you with daily life struggles from anxiety to menopause.
CBD is a chemical found in marijuana that doesn’t produce a high like the chemical component that does, tetrahydrocannabinol or THC.
The body has receptors for cannabidiol that are involved in pain, mood regulation, sleep, the immune system, fertility and reproduction, temperature regulation, and memory.

CBD oil and CBD-infused products are gaining in popularity. Some women+ report using it to aid in treating menopause symptoms – such as joint pain, sleeplessness, and anxiety.
However, consistency and potency may vary from product to product.
CBD health benefits
The study of CBD’s benefits for medical ailments is an active area of investigation and still under review, despite the marketing you may see.
While some research shows positive effects with the use of CBD, it’s not related to menopause. And the FDA has not approved it for use to address menopause symptoms.
For example, a 2020 article in Frontiers in Pharmacology evaluated the effects of CBD on chronic pain and identified these risks and benefits:
Risks
- Lack of long-term studies
- The presence of an analgesic (pain-relieving), or lack thereof, may depend on the cause of the chronic pain
- Lack of regulation
- Evidence of contamination in commercial preparations
- Preclinical evidence of teratogenicity (ability to cause defects in a developing fetus)
Benefits
- Improved sleep
- Well-tolerated
- Improved quality of life
- Effective for pain that wasn’t being controlled with standard medical care
- Non-psychoactive
- Increases bioavailability (the extent and rate at which the active component of the drug enters the circulation and can be absorbed and used by the body) of analgesics (medications that relieve pain)
There is also evidence that CBD may be helpful for those with mental health conditions.
Talk to your doctor before you try CBD, especially if you’re taking other medications.
CBD products may vary
Much of the CBD industry is unregulated, and the range of quality, purity, dosing levels, and efficacy of the products you may find is vast. And in some cases, the only treatment you will receive is the extraction of cash from your wallet!
Marijuana
Lastly, the use of marijuana in its various forms currently is still not legal at the Federal level, except under the 2018 Farm Bill for hemp and hemp-derived products with a THC content of less than 0.3%.
And the legal status of CBD and other cannabinoids varies by state.
Probiotics
Like so many other parts of your body, your gut also changes during menopause. Focusing on your gut health may improve how you feel during menopause.
You often hear people talking about their gut instinct or what their gut is telling them. It turns out science says there is indeed a connection!
It’s called the “gut-brain axis.” Some people even call your gut the “second brain.” Gut microbiota significantly affects metabolism and immunity, which means it can help protect against pathogens. In fact, the gut is home to the majority of immune cells in the body!
Although there is still much to be learned, there’s a well-established connection between the health of your gut and your health and well-being.
So, what makes up the health of your gut? Well, it’s the number and variety of organisms (bacteria, viruses, and fungi), the impact of medications like aspirin or NSAIDs on the lining of the gut, the impact of antibiotics on the balance and type of organisms, and the connection between the gut and hormone production.
If you’re feeling down during menopause, it may be related to your gut. The loss of estrogen during menopause is thought to be one reason women experience depression during the menopause transition.
It can also influence your weight, mood, and the amount of inflammation in your body, which in turn impacts other parts of your body, like your cardiovascular system.
Certain bacteria in the gut microbiome appear to increase or contribute to the risk of certain cancers (like colon cancer in African Americans and ovarian cancer).
Early research shows the potential positive benefits of a healthy gut, including on bone health (reduced risk of osteoporosis), weight (less difficult to lose it), and menopause symptoms (including hot flashes).
 Menopause changes your microbiome
Menopause changes your microbiome
Like most everything else with menopause, scientists at Arizona State University discovered the hormonal shifts that occur during the menopause transition changes the bacteria living in the gut, also known as the microbiome.
While estrogen treatment can improve the microbiome, it won’t reverse all the changes, according to researchers.
They are also looking at bacteria in vitamins, prebiotics, and probiotics as an alternative to hormone therapy.
There are many probiotics marketed for women+ in the menopause transition. So, which ones offer benefits? It can be hard to decipher as you’re navigating a complicated arena which you may never have heard of before. So, let’s break down some of the research.
Which probiotics might help with menopause?
Women between 40 and 60 took Lactobacillus acidophilus YT1 (MENOLACTO®) in a randomized, double-blinded, placebo-controlled clinical trial. The bacterium alleviated menopause symptoms and improved quality of life with no notable side effects.
Researchers believe MENOLACTO® could help women with hot flashes, nervousness, fatigue, headache, vaginal dryness, and heart palpitations.
Other Lactobacillus strains have also improved bone health and protected against osteoporosis. One study used a combination of three strains and found protection against lumbar spine loss in postmenopausal women.
Another study looked at probiotics with red clover isoflavones, an herb some women take to manage menopause symptoms. It was a small trial of 62 perimenopausal women who experienced five or more hot flashes daily. The women received isoflavones and probiotics or a placebo. In this trial, their physiological and self-reported vasomotor symptoms were reduced.
Probiotic studies on weight loss and mood
There are also several non-menopausal probiotic studies, including male and female participants. Many focused on common life issues like weight loss or mood changes. While not solely focused on those changes during menopause, the achieved benefits may offer menopausal women+ benefits.
In research on probiotic use for weight loss involving men and women, women lost weight while taking Lactobacillus rhamnosus. Interestingly, men did not see any improvement.
In another small study of men and women, trial participants saw improved mood, decreased anger and fatigue, and improved sleep.
Probiotic research is ongoing, and much is not yet known. So, talk to your doctor and also be on the lookout for scams, “miracle cures,” and false claims of the unproven benefits of a variety of products, as they are commonly seen in the unregulated world of supplements and probiotics.

Menopause Bloating and Constipation? Don’t Suffer From GI Pain Any More
Does your stomach hurt or feel bloated? Menopause GI pain can cause several symptoms in your gastrointestinal tract. Learn how to manage them.
Healing Your Body
 Acupuncture
Acupuncture
Acupuncture can help women bring their bodies into better balance. It’s low risk and (relatively) low cost. Plus, women+ see results quickly, so you know if it will be effective in a relatively short time. The results can also last for months after treatment.
Studies have found acupuncture to be effective in the treatment of several menopausal vasomotor symptoms (VSMs), including hot flashes and night sweats. Researchers at the medical schools at Duke University and Wake Forest reported a 36.7% reduction in the frequency of VMS at 6 months, with relief beginning at week 3 and maximum impact by week 8. At 12 months, the degree of relief had continued at a 29.4% reduction in frequency.
Other studies have found acupuncture can be effective in some women for additional issues which can arise during the menopause journey:
- anxiety
- bone density
- cognitive decline
- sleep disturbance
The Menopause Society recognizes acupuncture as a complementary and alternative treatment despite inconsistent study benefits.
Some experts believe sham acupuncture may be as effective as traditional acupuncture. While sham indicates fake, sham acupuncture is not fake. The acupuncturist follows a protocol; the difference is that the needles do not penetrate the skin.
It’s important to find a well-trained, licensed practitioner with pristine hygiene practices. The National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM) has a Find a Practitioner Directory
And you can also find out about practitioners through your state medical board, as licensure occurs at the state level.

Naturopathic, Integrative, and Functional Medicine: Holistic Health for Menopausal Women Explained
What’s the difference between naturopathic, integrative, functional, and Traditional Chinese Medicine?

What You Need to Know About Acupuncture Benefits for Menopause Symptoms
For many women, acupuncture is a viable alternative that can provide relief from menopause symptoms like hot flashes, night sweats, and sleeping problems. Learn about the benefits.
 Massage
Massage
Massage is excellent for pain relief and stress management, no matter your stage of life.
Therapists can use heat, pressure, touch, reflexology (the application of pressure to areas on the feet or hands and sometimes the ears), and vibration to stimulate healing.
Aromatherapy can also assist in relaxation, though one must be careful about the quality of the aromatherapy oils which are used. There have sometimes been recalls related to bacterial contamination.
During menopause, massage may improve symptoms. Research is limited and inconsistent.
In one randomized controlled study of 120 women, reflexology improved vasomotor and sexual dysfunction symptoms. Hot flashes decreased by 56% after 12 twice-weekly reflexology sessions. In another study, reflexology showed no improvement.
An Iranian study showed reflexology also helped women with sleep issues.
Another study found that craniofacial massage improved quality of life, mental health distress, and a negative body image.
Reflexology (foot massage)
In addition to a whole body massage, a massage focused on your feet can help improve symptoms during the menopause transition.
Massage helps individuals relax, reduce stress, and restore balance. And it stimulates the nerve cells in the leg.
A randomized controlled study in Turkey, published in Menopause, the journal of The Menopause Society, found a foot massage can help with sleep in postmenopausal women. In the small study, the women gained an average of one more hour of sleep each day!
With sleeplessness a common menopause complaint, foot massage is a relatively simple and easy way to improve sleep. (There are other ways to improve sleep, including listening to brain wave music or improving your sleep hygiene.)
It can also lower fatigue and anxiety. Fatigue is one of the top three menopause complaints according to The Menopause Society, and it’s often a result of hot flashes and poor sleep quality.
The Menopause Society said previous studies found foot reflexology was effective in helping with stress and fatigue in premenopausal women, but no previous studies looked at the effects of anxiety, fatigue, and sleep at the same time in postmenopausal women.
The findings, released in 2022, helped The Menopause Society conclude there is little downside to recommending foot massage as a non-hormonal way to improve menopause symptoms.
Find a massage therapist
There is no national certification process, and not every state requires a license (though most do via the state medical board). The American Massage Therapy Association offers a search tool to find a therapist.
Movement
 Pilates
Pilates
Pilates is perhaps one of the most active mind-body therapies, with body weight exercises that build strength and muscle tone. The focus is on the core, which can mean a reduced likelihood of back pain because of strengthening of the abdominal muscles.
The exercise also helps with flexibility.
While many movements in Pilates are active and can engage all your muscles simultaneously, there are also slower, more deliberate movements.
In a small study of 74 postmenopausal women, individuals experienced a significant decrease in menopausal symptoms (except for urogenital symptoms) after eight weeks of Pilates. The women participated in three Pilates sessions a week.
In addition to a decrease in symptoms, women also experienced an increase in lumbar strength and flexibility.
Pilates can be done without equipment, although there are also exercises that involve specific machines.
Like any new exercise, check with your medical practitioner before starting, especially if you have a known pelvic floor disorder or are at high risk of developing one.
Gyrotonic® Method
Gyrotonic® classes focus on movements that help with increased range of motion, strength, and agility. And there are variations of the Gyrotonic® Method, which make it more likely you’ll be able to find an approach that might work for you.
The low-impact workouts, which are performed seated, include movement sequences that flow from one to the next and can be adapted as needed.
Alexander Technique
FM Alexander created a technique focusing on your body’s posture and movement to improve health.
The American Society for the Alexander TechniqueTM (AmSAT) promotes the benefits of improved coordination of your musculoskeletal system, including improved posture, pain relief, and better stress management skills.
Athletes use it to improve strength, endurance, flexibility, speed, and accuracy.
You can apply the technique to your movements throughout your day.
Find an AmSAT-certified instructor who will provide verbal instructions and manual guidance in a private setting.
Feldenkrais Method®
How often do you think about how you move through life? Many of us walk, run, and sit through life with little thought about how we do it.
With the Feldenkrais Method®, you focus on body awareness.
Dr. Moshe Feldenkrais created this technique which uses gentle, mindful movements to improve thinking, emotional regulation, and problem-solving. This method can also offer pain relief and improve posture and balance.
For example, you may walk slowly and pay attention to your posture. Is your spine straight, shoulders relaxed, and hips pointed forward? While paying attention to your posture can help you medically, the broader focus and goal is to improve body awareness.
Menopause impacts a woman’s body in new ways, and awareness of what’s happening and how you can manage these symptoms can improve your journey throughout the transition.
It can also help you redefine your journey in a positive light, viewing it as a time of self-reflection and hyper-focus on how your lifestyle impacts how you feel.
You can learn the Feldenkrais Method® in a group setting or private session. Find a practitioner.
Improving Physical Balance
Tai Chi
Tai chi is an ancient martial art that originated in China. It’s a low-impact exercise focusing on gentle body movements and deep breathing.
You proceed through each movement slowly while concentrating on taking deep breaths.
Tai chi can help with strength, flexibility, and balance. It’s perfect for all fitness levels, and you can do it standing up or sitting down.
A small study found that tai chi slowed bone loss in early postmenopausal women.
A systematic review of five studies found perimenopausal women in China experienced improved body pain, general health, vitality, and mental health with tai chi.
Tai chi is also popular for reducing stress, improving health and fitness, and overall well-being. Studies have also found it can be helpful in reducing the risk of cardiovascular disease for individuals age 50 or older who are obese.
Study results are inconsistent, and researchers note they need more data to evaluate whether it effectively prevents osteoporosis.
The risks are typically minimal, though, with this low-impact exercise.
 Qigong
Qigong
Qigong, pronounced “chee gong,” is a physical mind and breath exercise developed thousands of years ago and used in Traditional Chinese Medicine (TCM). It optimizes mind, body, and spirit, energy, and well-being. And you have options:
- There’s Active Qigong, which focuses on body movements.
- Meditative Qigong emphasizes breathwork and mind exercises, with almost no body movement.
Qigong can work well for adults and those with limited mobility because the movements focus on relaxation, visualization, and long, slow, deep breaths and can be adapted to a range of levels of fitness or mobility, e.g., seated, in a wheelchair.
Qigong benefits for women+
Qigong can help prevent falls and improve balance, bone health, anxiety, and depression.
In a study of postmenopausal Spanish women, 12 weeks of qigong improved general health, physical function, body pain, vitality, and mental health.
There may also be cardiovascular health improvements, a concern of menopausal women. Controlled trials in China and Korea suggest that qigong can reduce blood pressure, fasting cholesterol, and triglyceride levels in adults with hypertension or cardiovascular disease.
A small study of perimenopausal women showed qigong improved sleep quality and climacteric symptoms such as hot flashes, vaginal dryness, sexual problems, and mood swings.
Types of qigong
Tai chi is a form of qigong. Other forms include:
- Baduanjin – a traditional Chinese mind-body aerobic exercise of moderate intensity which requires practitioners to achieve coordination between mind and body.
- Liuzijue – a traditional Chinese method of fitness that focuses on controlling breathing. It involves performing the actions of inhaling and exhaling through different mouth patterns to regulate and control the rise and fall of the breath in the body.
- Hu Ye Xian – originally choreographed by an ancient Chinese physician in the Donghan Dynasty and figuratively known as the “five animals” exercise. It includes movements imitating tigers, deer, bears, apes, and birds. Hu Ye Xian also involves symmetrically slow movements, integrated with breathing techniques, physical and mental relaxation, body awareness, and meditation.
- Yijin Jing – the aim is to strengthen the muscles and tendons and build stamina. The movement combinations stretch muscles, tendons, and ligaments for improved range of motion, mobility, resiliency, balance, and coordination.
- Medical Qigong – a form of healing energy therapy that incorporates the diagnostic and energetic balancing principles of Traditional Chinese Medicine (TCM); the first of the 4 branches of TCM, predating acupressure, acupuncture, and herbal medicine. When used with tai chi, the health benefits are even more substantial.
 Yoga
Yoga
There are many different types of yoga, and the intensity varies by practice. It’s a spiritual and physical exercise focusing on mindfulness, stretching, and strength.
Through different positions (poses), you enter a state of mindfulness that can improve your overall well-being no matter your stage of life.
There are inconsistent data on the impact of yoga on symptoms women+ experience during the menopause journey.
A review of studies about yoga and menopause indicates a general consensus regarding a positive impact on psychological symptoms.
Some studies also show yoga improves fatigue.
In a study of 216 perimenopausal women who did Patanjala and Hatha yoga for 12 weeks, the women saw improvement in hot flashes, night sweats, and sweating compared to the benefits of regular exercise. Sexual symptoms and anxiety also significantly improved.
Yoga can help with perceived stress, reduce symptoms of depression and anxiety, decrease anger, and improve sleep.
There’s also growing evidence that yoga may reduce risk factors for cardiovascular disease. Since menopause increases a woman’s risk for cardiovascular disease like hypertension and heart issues, yoga can be a beneficial intervention.
Yoga is an accessible and easy practice to learn and may offer women+ a non-invasive and approachable physical activity to manage their symptoms.
Relaxation
 Yoga Nidra
Yoga Nidra
While yoga is in the name, yoga nidra differs from traditional yoga forms. You perform this mind-body exercise lying down, and there are no postures.
The name means “yogic sleep.” With sleeplessness a common menopausal symptom, this may be just what you need.
It’s a guided meditation that helps you unwind and enter a state of complete relaxation while lying down.
During the exercise, you become aware of your body, feelings, emotions, and senses. You let go of anything holding you back – worries, stress, and emotions of the day.
You can do yoga nidra any time of day, but it’s a great practice to add to your sleep routine if you’re struggling with sleeplessness.
Yoga Nidra video
Try this guided yoga nidra for sleep.
 Paced breathing
Paced breathing
Slow-paced breathing is often used with cognitive behavioral therapy (CBT) because it can help you reframe your thoughts to positive or neutral ones. There is evidence that paced breathing can reduce hot flash frequency and severity.
It’s a safe and accessible treatment method that The Menopause Society recommends for women experiencing hot flashes. In a study of paced breathing versus progressive muscle relaxation, only paced breathing helped women significantly reduce hot flashes after eight weeks.
So, it can have an impact on its own or in conjunction with other mind-body relaxation techniques.
How to practice paced breathing
Some smartphone apps can guide you through the process, or you can do it yourself. There are also free videos available online.
All you need is a chair, your mind, and your body.
Sit in a straight-back chair with both feet on the floor, and rest your hands on your abdomen.
Feel your abdomen rise as you inhale slowly, counting to four. Hold your breath for a second, then exhale slowly for four seconds.
Find a rhythm that works for you, but the target rate is 6 to 8 breaths per minute.
When you feel a hot flash come on, use this exercise. Work through the breathing exercise for 15 minutes.
Women are advised to practice paced breathing twice a day, but the more often you experience hot flashes, the more often you should practice.
The Women’s Health Concern, part of the British Menopause Society, also notes that focusing on your breath helps you accept the hot flash as something that will pass with time. This acceptance reduces feelings of embarrassment or frustration, which will only cause more stress.
 Mindfulness Meditation
Mindfulness Meditation
Jon Kabat-Zinn, who is often called the “godfather of mindfulness,” defines mindfulness as “awareness that arises through paying attention, on purpose, in the present moment, non-judgmentally in the service of self-understanding and wisdom.”
Meditation is one technique, among many, that you can use to practice mindfulness. It has a relaxing effect on your body, and it brings about calm and psychological balance. It’s become a popular stress reduction technique and exercise cool down.
How mindfulness helps menopause symptoms
During menopause, meditation can help reduce hot flashes, sleep and mood disturbances, stress, and muscle and joint pain.
Mindfulness for menopause focuses on distancing yourself from the thoughts, feelings, and sensations of a menopause symptom like a hot flash. Simply observe the situation and how you feel, and don’t judge. Do not react!
Researchers at the Mayo Clinic found women between the ages of 40 and 65 who had higher mindfulness scores also had fewer mental health symptoms. These included reduced irritability, depression, and anxiety.
Research is ongoing into the effectiveness of meditation for many conditions. A form of mindfulness known as Mindfulness-Based Stress Reduction (MBSR) is effective in the management of several chronic conditions, such as diabetes, chronic pain, and high blood pressure (which is seen at increased rates during the menopause transition and after). And there are free resources available to learn more about it.
It is relatively safe in healthy people. In rare cases, meditation can worsen psychiatric problems like anxiety and depression. Talk with your doctor before beginning a meditation practice.
How to meditate
There are many ways to meditate, but they all usually have four things in common:
- A quiet place with few distractions.
- A comfortable posture.
- Focused attention. Only think about the present moment.
- A non-judgmental attitude.
Mindfulness impacts the autonomic nervous system, which regulates involuntary bodily functions like breathing, heart rate, and blood pressure.
It is composed of two components:
- The sympathetic nervous system – “fight or flight response”
- The parasympathetic nervous system – “rest and digest” response
Mindfulness helps dial up the parasympathetic response and dial down the sympathetic reaction.
You can do it at home using a guided meditation app or online video. We also have a mindfulness script using the RAIN technique.
Watch mindfulness webinars
During pausitive health webinars on mindfulness, our expert guides a mindful moment. Learn about how this can help you and give it a try. Watch this mindfulness playlist.
The accessibility of meditation, ease of use, and low risks associated with it make it another tool to help manage symptoms in a non-hormonal way. And it’s free!

Power Through Menopausal Changes with this RAIN Mindfulness Technique
The RAIN mindfulness technique can help you power through menopausal changes with a positive mindset. Read or listen to this script.

Missing Your Life Before Menopause? How to Manage The Grief and Loss
Do you ever think about life before menopausal symptoms? If you feel a sense of loss or grief, try these emotional coping strategies.

19 Menopause Self-Care Ideas To De-Stress and Improve Symptoms
Menopause self-care can de-stress you and improve symptoms. Take time for you! Learn 19 self-care ideas.
Listen to Your Body
How to perform guided imagery
You may hear about guided imagery as part of a meditation, mindfulness, self-hypnosis, or relaxation practice.
In effect, you visualize yourself someplace else and use that imagery to calm your mind, body, and soul.
That scenery can be the calming sound of waves crashing on the shore or the sight of palm trees swaying in the wind. It may be a brook, meadow, or forest.
Choose a place that brings about calm and happiness for you.
All you need is your imagination, a quiet and comfortable place to rest and close your eyes, and an app, video, or audio recording that guides you to this serene place. And there are also practitioners who offer “live” sessions, which can be more individualized to your needs.
As you visualize this location, focus on your breath. Take slow, deep breaths as you transport yourself to this place. While focusing on visualization, you want to experience more than just the scenes.
Transport your entire body to that location. Think about the sounds, smells, and objects you can feel there.
It’s more than just the waves crashing ashore. It’s the sensation or feeling as the water envelops your feet.
Watch these pausitive health guided imagery webinars and learn how it can help you change your mindset, clear out energy draining emotions, ease physical symptoms, and help with overall well-being.
 Hypnotherapy
Hypnotherapy
People use hypnosis to relieve various conditions, including irritable bowel syndrome (IBS), anxiety, headaches, post-traumatic stress disorder, and pain control, as well as for smoking cessation.
While the evidence is inconsistent for some of these conditions, the The Menopause Society considers hypnosis a “promising strategy for managing hot flashes.” There’s little risk and potential benefits.
How hypnosis helps with menopause
Hypnosis is a mind-body therapy that puts you into deep relaxation and increases focus. The focus is on controlling symptoms, so they don’t control you.
You’re hyper-focused so that you can respond to suggestions. But hypnotherapy is not mind control by another person! You will not be induced to do anything you would not otherwise be open to doing.
In the case of menopausal hot flashes, if the hypnotist tells you to imagine yourself in a cool place, your heightened response will help take you to that place.
Impact on hot flashes
While large-scale controlled and randomized studies are not available, smaller-scale studies show promising results with hypnosis to treat menopause symptoms.
In a study of postmenopausal women published in Menopause, hot flashes decreased significantly for women who had at least seven a day or 50 per week.
After 12 weeks of clinical hypnosis, the frequency dropped by 74%.
These women also experienced better sleep.
During the 45-minute in-person sessions, the women received suggestions for mental imagery for coolness, safe place imagery, and relaxation. Women also received an audio recording so they could practice self-hypnosis at home.
In another study of women with a history of breast cancer, hypnosis was better at reducing hot flashes, mood swings, and sleep than no treatment.
Hypnosis is generally safe when you consult a trained, licensed healthcare provider. In some cases, though, it can worsen some psychological problems.
Find a hypnosis practitioner
The American Society of Clinical Hypnosis has a search tool to help you find a certified hypnotherapist.
Emotional Freedom Technique (EFT)
The Emotional Freedom Technique, also known as tapping, focuses on sequential tapping on specific body parts. It allows you to tap into your internal healing powers so energy can flow freely without disruption or negative thoughts.
It’s a stress relief technique that can help with menopause symptoms like anger, rage, mood swings, and hot flashes.
How tapping works
During tapping, you locate meridian points on your body and recognize and accept emotional or physical pain without judgment.
While EFT follows specific steps to balance your energy, you can do it yourself at home.
The risks of the technique are minimal.


Can the Emotional Freedom Technique (EFT) Or Tapping Help Menopause Symptoms?
Emotional Freedom Techniques (EFT) or tapping are effective stress relief techniques. Tap into this self-help technique (no pun intended) when you’re in a fit of rage, stressed, or experiencing a mood swing or hot flash.
Cognitive Behavioral Therapy (CBT)
Cognitive behavioral therapy (CBT) is a form of psychotherapy that helps you change how you think and respond. It also asks if the stories you tell yourself are actually true and can help you reframe your perceptions. It focuses on understanding the connection between your thoughts, emotions, reactions, and behavior.
With menopause, CBT can make what is often a challenging situation, like hot flashes or difficulties with sleep, a less impactful experience. Changing your mindset can help you cope and reduce stress, which in turn is helpful in and of itself.
How to use CBT during menopause
Instead of thinking that everyone is staring at you as your face turns red or you break out in a sweat from a hot flash, CBT teaches women coping skills like acceptance. It can help you embrace this stage of life or have a more neutral response rather than a negative one, like embarrassment or dread.
Thinking of the hot flash negatively can aggravate the symptoms by increasing your stress and anxiety levels. Think about how strong you are for dealing with another hot flash and taking action to manage your journey.
Hot flashes can be less of a problem and nuisance with this more neutral emotional response.
If night sweats interrupt a night of sleep, don’t think worst-case scenario about how it will negatively impact your day. Recognize how many other times you’ve experienced them and still gotten through the day.
 CBT and hot flashes
CBT and hot flashes
Studies in the UK and Netherlands show women experience significantly fewer hot flashes and night sweats with CBT.
Unlike hormone treatment, CBT has little, if any, risks. Plus, the coping strategies have long-lasting effects in life and help you achieve balance to manage negative thoughts, stressors, and anxiety more effectively.
The Menopause Society supports cognitive behavioral therapy for menopause symptoms because of the positive benefits for women+ suffering from hot flashes and other menopause-related issues like depression, sleeplessness, and sexual concerns.
Find a CBT provider
pausitive health members can access digital CBT (d-CBT) as part of our program. Become a member today.
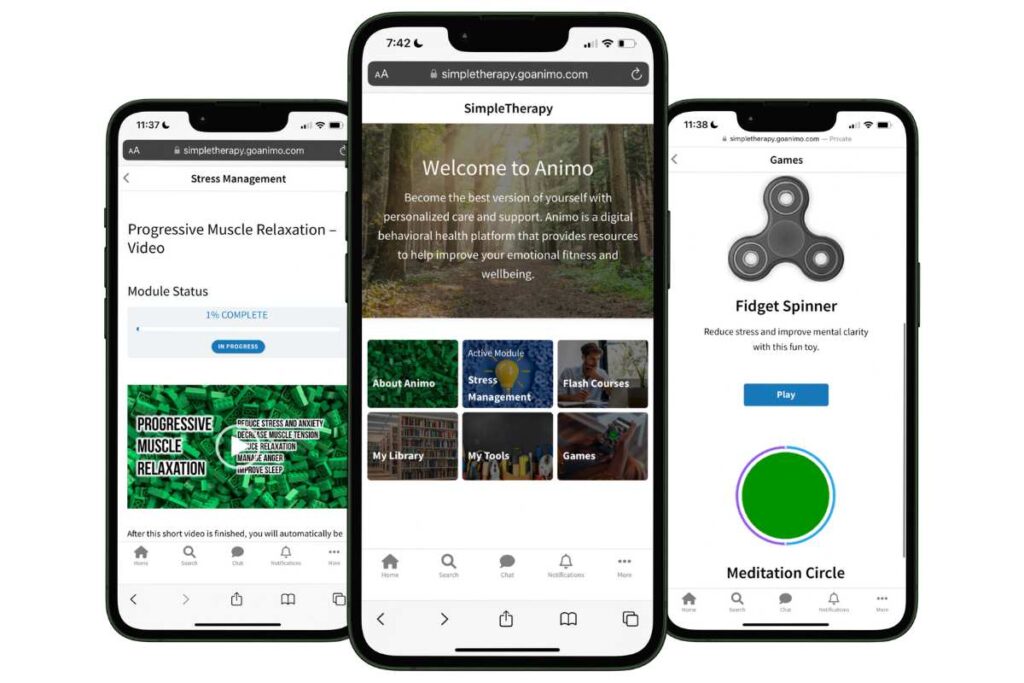
Free Digital CBT (d-CBT)
Only available for a limited time!
Become a member of the pausitive health pilot program and get access to complimentary digital cognitive behavioral therapy (d-CBT) from our collaboration partner, SimpleTherapy. These sessions can relieve anxiety, stress, and depressive symptoms.
As a member, you’ll also get access to personalized text messages that focus on topics you select, virtual care, a supportive community, and more!
The Association for Behavioral and Cognitive Therapies (ABCT) provides a way to Find a Practitioner.
Psychology Today also provides a Find a Practitioner directory for those trained in CBT.
The Academy of Cognitive Behavioral Health Therapists has a directory as well.

17 Menopausal Anxiety Treatment Options To Ease Your Mind
Feeling anxious during the menopause journey? Try these 16 anxiety treatment options to ease your mind of worry and fear.
Conquer Menopausal Hot Flashes And Sleeplessness With CBT
Learn about cognitive behavioral therapy or CBT to help manage hot flashes, night sweats, and sleeplessness.
Arts
Music Therapy
Music is a universal language, and it has the power to change emotions and thoughts quickly. It can energize, relax, or make you sad in a few seconds.
Music stimulates the release of neurotransmitters like dopamine and serotonin, the hormone oxytocin, and endorphins. At the same time, stress hormones decrease.
It also makes it easier to forget past and future worries and focus on the present, so you are really being present in the moment.

Music and menopause
There is promising research into the use of music therapy for several conditions, including Parkinson’s disease, stroke, and chronic pain.
It also effectively treats mood disorders and depression – something many menopausal women+ experience.
A new Turkish study, which was small, showed music could significantly decrease depression and reduce menopause symptoms in postmenopausal women.
The study, published in Menopause, found music improves depression, hot flashes, sexual dysfunction, and sleep issues during menopause.
Dr. Stephanie Faubion, medical director of The Menopause Society, highlighted the study and pointed out an “easy-to-implement, low-cost, low-tech, and low-risk intervention.”
She said, “Although additional research is needed to confirm these findings in larger study populations, there is little downside to adding music therapy to our armamentarium for menopause symptom management.”
Music also allows an easy, free way to experiment and pull what we need to feel better at any given time. For some, when they are down, listening to sad or melancholy music makes them feel better because of a sense of capturing the emotions the person is experiencing. Upbeat music does the trick for others because it helps lift their spirits and gets them out of a funk. And the same individual may respond differently at different points in time.
In addition to traditional music, you can listen to brain-wave sleep music. It’s often called music, but it’s a combination of sounds that target specific brain waves that can help you sleep by putting you into a more relaxed state.
Ready to take the edge off menopause? Listen to music.

The Sleep Hygiene Hack That “Tunes” Your Brain For Better Quality Sleep
Ready to “tune” your brain for better sleep? Add binaural beats to your sleep hygiene routine to improve sleeplessness during menopause.
Dance Therapy
Dance therapy relies on the power of music in tandem with movements to help you feel better. Music is powerful on its own as a non-hormonal approach to managing menopause. Combined with dance, you engage the mind and body.
Try dancing away the blues of menopause if you’re struggling with weight, your mood and emotions, brain fog, or stress.
A recent study published in Menopause demonstrated dancing lowered cholesterol levels, improved fitness and body composition and boosted self-esteem in postmenopausal women.
It also improves health and happiness, boosting the “happiness neurochemicals” of dopamine and oxytocin.

Art Therapy
How do you express what you’re feeling during menopause with words? Now, consider how you’d describe your menopause journey with art. Would the expression be different in each exercise?
Now, think beyond the original artwork you created in your head. Create that art using various mediums, textures, and tools. Does menopause look different again?
Art therapy helps you express yourself during menopause.
Art therapy is a form of psychotherapy that can help you tap into your inner thoughts and feelings. It can help you heal and change the way you view things.
The American Art Therapy Association says art therapy has the power to help with:
- Cognitive and sensory-motor functions
- Self-esteem
- Self-awareness
- Emotional resiliency
- Social skills
- Insight
- Conflicts and distress
- Societal and ecological change
Hospitals, communities, memory care, and correctional institutions commonly use it for individuals struggling with anxiety, grief, or another traumatic event. Art therapy also helps children, seniors, veterans, and military members.
While focusing on the art, you distract yourself from other thoughts and worries. That way, you create a pathway to express yourself without worry or judgment.
Art therapy benefits observed in studies
In the UK, art therapy helps menopausal women deal with debilitating symptoms. These include confusion, depression, anxiety, and exhaustion.
In an Iranian study of 104 menopausal women, mindfulness-based art therapy (MBAT) helped women with their menopausal symptoms. The authors called it “encouraging data” that decreased signs of distress and improved lifestyles.
During menopause, women have positive and negative experiences. Art therapy can help you process your emotions.
Find an art therapist
Art therapists are trained in this field and considered healthcare professionals. Find an art therapist from the American Art Therapy Association.
Lifestyle Choices
Nutrition
Healthy eating plays a critical role in your health and well-being.
During menopause, these differences matter. Healthy food choices can reduce symptoms like hot flashes and help manage weight gain. At the same time, other foods can make your symptoms worse.
It’s never too late to improve your nutrition, but the earlier you start, the better control you’ll have over your menopause journey. So, what should you eat?

Soy isoflavones
Plant-based estrogens and soy get a lot of attention because soy is often a staple in the Asian diet, and Asian women tend to have fewer hot flashes.
Only 10-20% of Asian women in Asian countries have hot flashes; in the U.S., that number is closer to 70-80%.
Despite that anecdotal evidence, a review of hundreds of studies found mixed results on the effects of isoflavones (of which soy is the most commonly used) in midlife.
And for a time, there was concern about eating soy and the possible risk of breast cancer.
According to the Dana-Farber Farber Cancer Institute, “Those undergoing treatment for ER+ breast cancer may want to avoid soy protein isolate in powdered form as well as soy protein enriched nutrition bars or vegetarian meat replacements.”
For everyone else, the current general opinion appears to be that soy intake is safe in the forms and quantities most people would eat such products (tofu, edamame, soy protein powder).
While further research is needed, The Menopause Society found it’s reasonable for postmenopausal women to try soy for distressing vasomotor symptoms. The study showed a modest impact on hot flashes in early post-menopause stage of the journey.
Healthy eating for menopause
If you’re looking to improve your nutrition, you can also try these food categories:
- Naturally low-fat foods
- Vegetables
- Plant-based based foods
- Fruit
- Whole grains
- Nuts and seeds
- Fiber-rich foods
- Water
Lower or eliminate foods high in:
- Saturated fat
- Trans fat
- Sugar
- Red meat
Focusing on these healthy diet staples can help prevent osteoporosis, control weight, and manage menopause symptoms like hot flashes.
Ongoing research shows that healthy foods can boost your brain health and prevent Alzheimer’s disease.
The Mediterranean Diet has been found to be healthy, with benefits regarding a reduced risk for overweight/obesity and the development of chronic conditions like diabetes and cardiovascular disease.
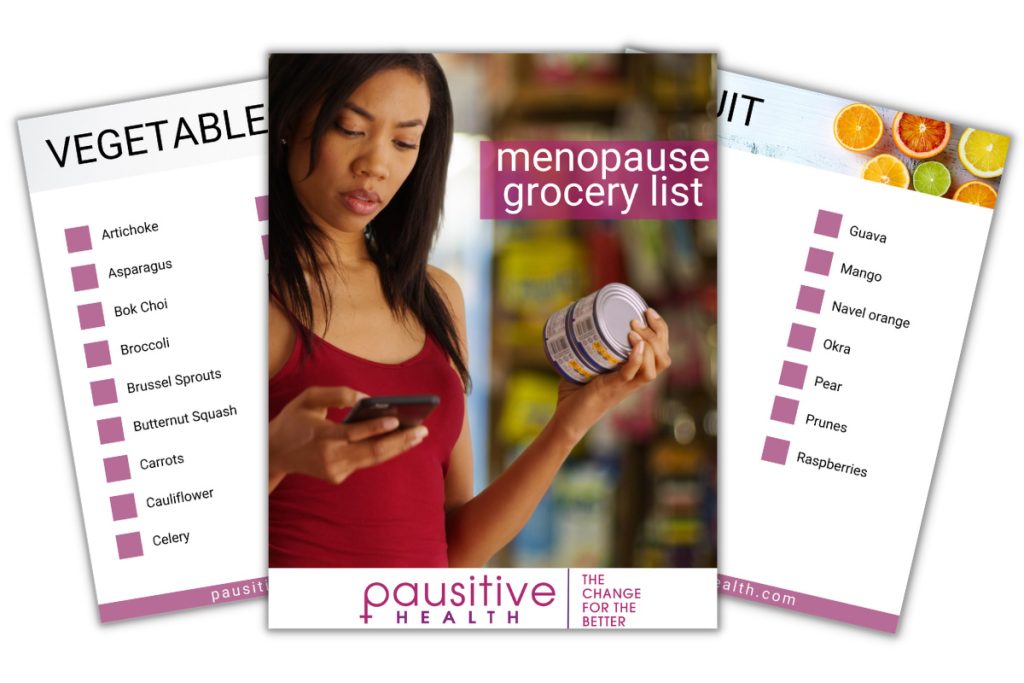
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
"*" indicates required fields

Best Foods To Eat To Manage Restless Leg Syndrome (RLS)
Food as medicine. Get a list of the best foods to eat to manage restless leg syndrome (RLS) and avoid triggering it.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

Healthy Eating Tips From Around The World That Can Make Menopause Easier
Food as medicine. It can be as powerful as medicine for menopause symptoms. Get healthy eating tips from around the world to manage symptoms.
 Mindful eating
Mindful eating
Ever heard “you are what you eat”? During menopause, your body may throw multiple curveballs like cravings and stress eating. If you aren’t paying attention and consume food mindlessly, you are more likely to eat more, as well as scarf down food that may taste good in the moment but leaves you sluggish and regretful later.
Focusing on healthy foods rich in the necessary nutrients to keep your body humming can help you manage menopause symptoms.
While healthy food fuels your body, how much you eat also matters.
Mindful eating can help you with portion control and binge eating.
With mindful eating, you focus on what you’re eating. You’re not on your phone, and you’re not distracted.
You indulge in the process of feeling, seeing, and savoring every piece of food.
Power of water
Do not overlook the power of water! Aim for 8-12 glasses a day.
It offers benefits for managing common menopause symptoms like skin and vaginal dryness, weight gain, and hot flashes.
Water can replenish the lost moisture, cool you down during a hot flash, make you feel full so you don’t eat as much, reduce the risk of UTIs, and help prevent constipation.
 Watch your weight
Watch your weight
Weight gain is a common problem for menopausal women.
And it’s common for more of the weight to accumulate in the abdominal area compared to the hips and thighs. That distribution is particularly concerning because internal fat around the organs triggers inflammation, which puts you at increased risk for inflammation and chronic conditions, like heart disease and diabetes.
The drop in estrogen levels may be one link to weight gain during the menopause journey. Additional factors that can also contribute include a reduction in muscle mass as one gets older and a lifestyle that includes unhealthy eating (e.g., processed foods, white starches, trans fats, lots of red meat), insufficient sleep, and not enough physical activity.
The University of Washington indicates most people gain 5 – 8% of their baseline body weight during the first two years of menopause. And according to a report in the Mayo Clinic Proceedings, almost three-quarters of women aged 60 and older are overweight.
It was also one of the top concerns for women+ in a pausitive health survey. One woman who described her experience as mild said weight gain was the biggest obstacle.
“The biggest issue has been weight gain in my stomach area and slower digestion,” she explained.
This metabolic slowdown is sometimes called the “midlife metabolic crisis.” Whether it’s a crisis or a cause of concern for you, a woman’s metabolism tends to slow as she ages.
After 40, it is common to gain 1- 2 pounds a year, which you might not notice. However, these slow weight changes mean over 10 years you may have gained 20 pounds without realizing it until more and more of your clothes don’t fit and you struggle to get the extra weight off.
Most people will need to take a fresh look at their lifestyle habits, and the earlier the better.
First, are you getting enough sleep? If not, you’re more likely to eat more, as well as less healthy foods. So, focus on getting 7-8 hours of high-quality sleep.
Second, take a look at your portions and calorie intake. Most people grossly underestimate both. Track what you eat throughout the day to improve accountability and to manage your portions.
Third, don’t eat for at least 3-4 hours before bed. If you give your body 10-12 hours of rest between dinner and breakfast, your body can process what you’ve already consumed. And there is growing evidence that intermittent fasting (compressing all your eating to occur during an 8-hour period) can aid in weight loss.
Know that you’re not alone. And in this case, you can talk about your misery and connect with others in the same boat to help support each other and lose weight together.
Weight gain can also make menopause symptoms worse, especially hot flashes and night sweats, along with increasing the chance of other health conditions.
If you’re struggling with weight gain, try these nine techniques known to be effective ways to take care of menopause weight gain.
 Get enough high-quality sleep
Get enough high-quality sleep
Sleep is fundamental to good health, and a lack of it can raise your risk for heart disease, hypertension, obesity, and depression. Yet, it can be hard to get enough sleep, and even more so during menopause.
Middle-of-the-night awakenings and night sweats are common. Once you’re up, it can be challenging to fall back asleep.
Your sleep routine should be the first place you start.
Sleep routines that work
Sleep hygiene can help address the underlying reasons for not getting enough sleep. It’s a 24/7 process and not just something you practice a few minutes before bed.
Watch your alcohol and caffeine intake, eat healthy meals during the day, exercise, and manage stress.
Then, focus on your bedroom. Is it a good sleep environment with few to no distractions? Ideally, your bedroom should be used only for sleep and sex.
Avoid intense exercise before bed, and eliminate exposure to blue light-emitting electronics like your cell phone at least an hour before bed.
Next, create a bedtime routine that will send a signal to your body that it’s time for sleep, e.g., dimmed lights, gentle yoga designed to induce relaxation and help sleep, deep breathing, and meditation.
Finally, do you have ways to fall asleep if you’re awakened in the middle of the night? Arm yourself with a sleep routine to fall back asleep quickly.
Many women use melatonin, an over-the-counter dietary supplement, to improve sleep. However, melatonin can sometimes have the opposite effect, and the wrong dose may cause new problems. Additionally, it can interact with several types of medication.
Several of the mind-body therapies discussed earlier are also helpful in improving sleep, including cognitive behavioral therapy (CBT) and paced breathing.

Why Women+ Are Prone To Restless Leg Syndrome (RLS) And How To Treat It
Do your legs move uncontrollably at night? Learn why Restless Leg Syndrome (RLS), is more common in women and how to treat it.

Having Leg Pain And Cramps? You May Be In Menopause
Do you have leg pain and cramps, during the day or at night? It’s a menopause symptom. Learn how to treat the leg pain.

Why Can’t I Sleep During The Menopause Transition? Understanding It Can Help You Sleep
Understanding why you can’t sleep during perimenopause and menopause can help you get more sleep.

The Sleep Hygiene Hack That “Tunes” Your Brain For Better Quality Sleep
Ready to “tune” your brain for better sleep? Add binaural beats to your sleep hygiene routine to improve sleeplessness during menopause.

Having Trouble Sleeping? How To Kickstart A Menopause Journey Sleep Routine That Works
Waking up in the middle of the night? Beat sleeplessness with this sleep routine.
Relax! Sleep Better With These Day And Night Mind-Body Remedies
Can’t sleep? Try these day and night mind-body remedies for better sleep.
Quit smoking
Want to improve your menopause symptoms? Stop smoking!
Research shows smoking increases menopause symptoms like hot flashes.
Be aware, however, that even if you quit, you’re at an increased risk for hot flashes compared to lifelong non-smokers. But if you haven’t stopped yet, then menopause is one more reason on a long list of reasons to do so – lung cancer, wrinkles and premature aging of the skin, COPD, and heart disease, just to name a few.
Smoking and hot flashes
Quitting can reduce the severity and frequency of hot flashes. The earlier you stop, the better!
Studies have shown that smokers who quit for five years or longer were 45% less likely to have severe or frequent hot flashes compared to those who never quit.
 Stress can make menopause symptoms worse
Stress can make menopause symptoms worse
Stress may seem unavoidable, especially during midlife, but can be a destructive force you should not underestimate.
Stress and menopause symptoms can turn into a vicious cycle.
During menopause, symptoms can make stress worse. Think about sleepless nights. If you’re worried, it will likely be harder to fall back asleep after being awakened by night sweats.
And, being stressed can make symptoms worse. The Study of Women’s Health Across the Nation shows women upset by a stressful event experienced 21% more vasomotor symptoms than women with no life stressors.
Chronic stress can also increase the risk or contribute to health problems, including overweight/obesity, depression, and heart disease.
A Yale study found that premenopausal women who were not overweight but were vulnerable to stress had excess abdominal fat. (Excess fat around the internal organs increases inflammation in the body, which, in turn, increases the risk of conditions like heart disease.) They also had higher levels of the stress hormone cortisol.
Manage stress and develop coping skills
So, how do you manage stress? First, figure out your triggers. Next, change your response to a stressful event with coping mechanisms.
Many non-hormonal mind-body therapies discussed here are effective at relieving stress and other menopause symptoms. These include cognitive brain therapy, tai chi, Pilates, qigong, paced breathing, gratitude, music therapy, and art therapy.
Be Less Stressed
Feeling stressed or overwhelmed? Learn life hacks to reduce stress with the Be Less Stressed toolkit.
"*" indicates required fields
Mindfulness-based stress reduction (MBSR)
You can also try mindfulness-based stress reduction (MBSR). That takes mindfulness to a new level and is effective in managing many chronic conditions.
One study showed that Mindfulness-Based Stress Reduction (MBSR) reduced anxiety, stress, sleep issues, and hot flashes.
Mind-body techniques help you to focus on the present moment without judgment.
Over time, they can also help you change your mindset so you have a more positive perspective on menopause, making it easier to manage symptoms so they don’t add stress to your life.

How Stress Affects Your Body and Makes Menopause Symptoms Worse
Did you know stress symptoms and menopausal symptoms are similiar?Learn how stress affects your body and how it can mkae menopause symptoms worse.

19 Menopause Self-Care Ideas To De-Stress and Improve Symptoms
Menopause self-care can de-stress you and improve symptoms. Take time for you! Learn 19 self-care ideas.
 Exercise | Physical Activity
Exercise | Physical Activity
Exercise is a powerful tool during menopause to improve mental, physical, and emotional well-being.
It is especially effective if (1) you mix things up to make sure you include aerobic exercise, strength training, weight-bearing exercise, and physical activity that helps flexibility and balance and (2) you find something you actually enjoy and in which you will consistently engage as time goes on.
Be creative and try a variety of activities to keep your heart healthy and help manage your weight. Aerobic exercises don’t always have to include running, a bike, or a machine. You can dance, try a HIIT (high-intensity interval training) workout, or even walk, which has a multitude of health and well-being benefits.
Benefits of walking
Don’t underestimate the power of a walk. If that’s all you have energy for, do it!
Menopausal women who walked at a fast pace for 40 minutes several times a week reduced their risk of heart disease by 25%, according to research presented by the American College of Cardiology.
Walking outside can also help you clear your mind from stress. Walk in peaceful locations like trails and the woods to practice forest bathing.
Use strength training to keep your bones strong and protect against osteoporosis. Try Pilates, weights, body weight, balance, core workouts, and stretching exercises.
Finally, try mind-body exercises like yoga, tai chi, yoga nidra, and qigong to manage stress and improve sleep.
Want new ideas to jazz up your exercise routine? Get ten menopause exercises to improve how you feel.

Yoga For Lifelong Strength: 5 Yoga Types To Power Through Daily Life
Yoga can provide lifelong strength. Learn about 5 yoga types and the benefits so you can power through daily life.

Discover Inner Balance: 8 Yoga Poses To Help Manage Menopause Symptoms
Yoga can improve your emotional and physical well-being during menopause, easing symptoms like hot flashes and sleeplessness. Try these yoga poses. for menopause.

28 At-Home Osteoporosis Exercise Videos To Help Prevent or Manage It
Try these at-home osteoporosis exercise videos from our collaborative partner. They can help prevent or manage osteoporosis and osteopenia.

Menopause Exercise Videos To Improve How You Feel
Try these menopause exercise videos to improve how you feel. They can help with weight loss, body strength, and flexibility.

How Exercise Can Positively Change Your Menopause Journey
Exercise is a secret weapon for menopausal women. It can help symptoms, lower risks of some conditions, help with weight, muscle tone, and strength.
Individualizing Treatment
“More research is needed. Results are inconsistent.”
How many times did you read those words in this ultimate guide to non-hormonal remedies? A lot!
It’s the reality, but it doesn’t mean integrative modalities don’t work. They can be a viable alternative to hormone therapy for certain symptoms, and many women+ see success.
More than 60% of the women who’ve tried CAM believe the treatments help menopause symptoms.
So, which non-hormonal technique should you try? It depends on your situation and menopause symptoms.
Treatment should be personalized based on your personal and family history and risk factors for various conditions.
Knowledge is power! Get the latest information from menopause societies or find a practitioner who specializes in the treatment you’re interested in trying:
- Women’s Health Concern
- EMAS
- Australian Menopause Society
- The Menopause Society
- National Center for Complementary and Integrative Health
Find a practitioner

Change How You Feel During Menopause With These Blue Zone Tips For Aging
Do you want to live a long healthy life disease free? It happens around the world. Change how you feel during menopause with these Blue Zone tips.

Naturopathic, Integrative, and Functional Medicine: Holistic Health for Menopausal Women Explained
What’s the difference between naturopathic, integrative, functional, and Traditional Chinese Medicine?
Ways to manage menopause
There are lots of options to help manage menopause symptoms. Knowledge is power! If you don’t want to take hormones, tell your doctor no and discuss other things you’d like to try. If that person has nothing more to offer, take what you’ve learned and find a practitioner who listens to your concerns and goals and can help you map out an approach that fits your specific needs. Every menopause journey is unique!
Complementary & alternative therapies | Women’s Health Concern
Biglia N, Bounous VE, De Seta F, Lello S, Nappi RE, Paoletti AM. Non-hormonal strategies for managing menopausal symptoms in cancer survivors: an update. Ecancermedicalscience. 2019 Mar 11;13:909. doi: 10.3332/ecancer.2019.909. PMID: 31123492; PMCID: PMC6445536.
Koch, L. Citalopram for hot flashes. Nat Rev Endocrinol 6, 475 (2010). https://doi.org/10.1038/nrendo.2010.116
Evans ML, Pritts E, Vittinghoff E, McClish K, Morgan KS, Jaffe RB. Management of postmenopausal hot flushes with venlafaxine hydrochloride: a randomized, controlled trial. Obstet Gynecol. 2005 Jan;105(1):161-6. doi: 10.1097/01.AOG.0000147840.06947.46. PMID: 15625158.
Find a Menopause Practitioner | The Menopause Society
Yoon, Sang-Hee MD, PhD; Lee, Ji Young MD, PhD; Lee, Chulmin MD, PhD; Lee, Hyojin MD; Kim, Soo-Nyung MD, PhD. Gabapentin for the treatment of hot flushes in menopause: a meta-analysis. Menopause 27(4):p 485-493, April 2020. | DOI: 10.1097/GME.0000000000001491
Alternatives: Hormone replacement therapy | NHS UK
Home | Intrarosa
Home | American Herbalists Guild
Paszkowski T, Skrzypulec-Plinta V. Assessment of quality of life in women using Femelis Meno. Prz Menopauzalny. 2018 Jun;17(2):77-85. doi: 10.5114/pm.2018.77306. Epub 2018 Jun 30. PMID: 30150915; PMCID: PMC6107096.
Winther K, Rein E, Hedman C. Femal, a herbal remedy made from pollen extracts, reduces hot flushes and improves quality of life in menopausal women: a randomized, placebo-controlled, parallel study. Climacteric. 2005 Jun;8(2):162-70. doi: 10.1080/13697130500117987. PMID: 16096172.
Pollen extract | Memorial Sloan Kettering Cancer Center
Czuczwar P, Paszkowski T, Lisiecki M, Woźniak S, Stępniak A. The safety and tolerance of phytotherapies in menopausal medicine – a review of the literature. Prz Menopauzalny. 2017 Mar;16(1):8-11. doi: 10.5114/pm.2017.67365. Epub 2017 Apr 26. PMID: 28546801; PMCID: PMC5437054.
Relizen | Bonafide
Fouad S, El Gendy A, Monir R, Abdel-Wahhab KG, Shafei HF, Hegazi AG. Bee Products for Relieving Menopausal Symptoms. Open Access Maced J Med Sci [Internet]. 2022 Feb. 15 [cited 2023 May 17];10(B):632-8. Available from: https://oamjms.eu/index.php/mjms/article/view/8191
Münstedt K, Voss B, Kullmer U, Schneider U, Hübner J. Bee pollen and honey for the alleviation of hot flushes and other menopausal symptoms in breast cancer patients. Mol Clin Oncol. 2015 Jul;3(4):869-874. doi: 10.3892/mco.2015.559. Epub 2015 May 4. PMID: 26171198; PMCID: PMC4486804.
Argueta DA, Ventura CM, Kiven S, Sagi V, Gupta K. A Balanced Approach for Cannabidiol Use in Chronic Pain. Front Pharmacol. 2020 Apr 30;11:561. doi: 10.3389/fphar.2020.00561. PMID: 32425793; PMCID: PMC7204604.
Not a Freudian Slip: CBD and Mental Health – Therapeutic Magic or Myth? Part 2 | Wharton Healtcare Quarterly
Hemp Production and the 2018 Farm Bill | U.S. Food and Drug Administration
The Farm Bill, hemp legalization and the status of CBD: An explainer | Brookings
State Medical Cannabis Laws | National Conference of State Legislatures
Lim EY, Lee SY, Shin HS, Lee J, Nam YD, Lee DO, Lee JY, Yeon SH, Son RH, Park CL, Heo YH, Kim YT. The Effect of Lactobacillus acidophilus YT1 (MENOLACTO) on Improving Menopausal Symptoms: A Randomized, Double-Blinded, Placebo-Controlled Clinical Trial. J Clin Med. 2020 Jul 9;9(7):2173. doi: 10.3390/jcm9072173. PMID: 32660010; PMCID: PMC7408745.
If Serotonin Doesn’t Cause Depression, Then What Does? | Psychology Today
African Americans, The Microbiome, and Colon Cancer | BetterBiome
Hormone and gut bacteria link may guide better treatment for menopause symptoms | Arizona State University
Jansson P, Curiac D, Lazou Ahrén I, Hansson F, Martinsson Niskanen T, Sjögren K, et al. Probiotic treatment using a mix of three Lactobacillus strains for lumbar spine bone loss in postmenopausal women: a randomised, double-blind, placebo-controlled, multicentre trial. The Lancet Rheumatology. 2019, Volume 1, Issue 3, E154-E162.
Lambert MNT, Thorup AC, Hansen ESS, Jeppesen PB. Combined Red Clover isoflavones and probiotics potently reduce menopausal vasomotor symptoms. PLoS One. 2017 Jun 7;12(6):e0176590. doi: 10.1371/journal.pone.0176590. PMID: 28591133; PMCID: PMC5462345.
Sanchez M, Darimont C, Drapeau V, Emady-Azar S, Lepage M, Rezzonico E, Ngom-Bru C, Berger B, Philippe L, Ammon-Zuffrey C, Leone P, Chevrier G, St-Amand E, Marette A, Doré J, Tremblay A. Effect of Lactobacillus rhamnosus CGMCC1.3724 supplementation on weight loss and maintenance in obese men and women. Br J Nutr. 2014 Apr 28;111(8):1507-19. doi: 10.1017/S0007114513003875. Epub 2013 Dec 3. PMID: 24299712.
Marotta A, Sarno E, Del Casale A, Pane M, Mogna L, Amoruso A, Felis GE, Fiorio M. Effects of Probiotics on Cognitive Reactivity, Mood, and Sleep Quality. Front Psychiatry. 2019 Mar 27;10:164. doi: 10.3389/fpsyt.2019.00164. PMID: 30971965; PMCID: PMC6445894.
Avis NE, Coeytaux RR, Isom S, Prevette K, Morgan T. Acupuncture in Menopause (AIM) study: a pragmatic, randomized controlled trial. Menopause. 2016 Jun;23(6):626-37. doi: 10.1097/GME.0000000000000597. PMID: 27023860; PMCID: PMC4874921.
Acupuncture for Menopausal Symptoms | Evidence Based Acupuncture
NCCAOM® Find a Practitioner Directory | National Certification Commission for Acupuncture and Oriental Medicine (NCCAOM)
CDC Expands Recall fo Aromatherapy Sprays Tied to Rare Illness | HealthDay
Johnson A, Roberts L, Elkins G. Complementary and Alternative Medicine for Menopause. J Evid Based Integr Med. 2019 Jan-Dec;24:2515690X19829380. doi: 10.1177/2515690X19829380. PMID: 30868921; PMCID: PMC6419242.
Asltoghiri M, Ghodsi Z. The effects of Reflexology on sleep disorder in menopausal women. Procedia – Social and Behavioral Sciences, Volume 31, 2012, Pages 242-246, ISSN 1877-0428. https://doi.org/10.1016/j.sbspro.2011.12.049.
Espí-López G, Monzani L, Gabaldón-García E, Zurriaga R. The beneficial effects of therapeutic craniofacial massage on quality of life, mental health and menopausal symptoms and body image: A randomized controlled clinical trial. Complementary Therapies in Medicine, Volume 51, 2020, 102415, ISSN 0965-2299.
https://doi.org/10.1016/j.ctim.2020.102415.
Foot Massage Effective in Improving Sleep Quality and Anxiety in Postmenopausal Women | The Menopause Society
Find a Massage Therapist | American Massage Therapy Association
Lee H, Caguicla JM, Park S, Kwak DJ, Won DY, Park Y, Kim J, Kim M. Effects of 8-week Pilates exercise program on menopausal symptoms and lumbar strength and flexibility in postmenopausal women. J Exerc Rehabil. 2016 Jun 30;12(3):247-51. doi: 10.12965/jer.1632630.315. PMID: 27419122; PMCID: PMC4934971.
Gyrotonic® Method | Gyrtonic®
Find a Studio | Gyrotonic®
The Alexander Technique | American Society for the Alexander Technique™
Find an AmSAT-Certified Teacher Near You | American Society for the Alexander Technique™
Home | Feldenkrais Method
Find a Practitioner | Feldenkrais Method
The health benefits of tai chi | The President and Fellows of Harvard College
Chan K, Qin L, Lau M, Woo J, Au S, Choy W, Lee K, Lee S. A randomized, prospective study of the effects of Tai Chi Chun exercise on bone mineral density in postmenopausal women. Arch Phys Med Rehabil. 2004 May;85(5):717-22. doi: 10.1016/j.apmr.2003.08.091. PMID: 15129394.
Wang Y, Shan W, Li Q, Yang N, Shan W. Tai Chi Exercise for the Quality of Life in a Perimenopausal Women Organization: A Systematic Review. Worldviews Evid Based Nurs. 2017 Aug;14(4):294-305. doi: 10.1111/wvn.12234. Erratum in: Worldviews Evid Based Nurs. 2017 Oct;14 (5):424. PMID: 28742289.
Sun, Lei MD; Zhuang, Lv-Ping MD; Li, Xiu-Zhu MD; Zheng, Jian MD; Wu, Wei-Fen MD. Tai Chi can prevent cardiovascular disease and improve cardiopulmonary function of adults with obesity aged 50 years and older: A long-term follow-up study. Medicine 98(42):p e17509, October 2019. | DOI: 10.1097/MD.0000000000017509
Qigong: What You Need To Know | National Center for Complementary and Integrative Health
Jahnke R, Larkey L, Rogers C, Etnier J, Lin F. A comprehensive review of health benefits of qigong and tai chi. Am J Health Promot. 2010 Jul-Aug;24(6):e1-e25. doi: 10.4278/ajhp.081013-LIT-248. PMID: 20594090; PMCID: PMC3085832.
Carcelén-Fraile M, Hita-Contreras F, Martínez-Amat A, Loureiro V, Loureiro N, Jiménez-García J, Fábrega-Cuadros R, Aibar-Almazán A. Impact of Qigong exercises on the severity of the menopausal symptoms and health-related quality of life: A randomised controlled trial. Sport & Exercise Medicine & Health. 2022. Pages 656-664. https://doi.org/10.1080/17461391.2022.2044915
Innes KE, Selfe TK, Taylor AG. Menopause, the metabolic syndrome, and mind-body therapies. Menopause. 2008 Sep-Oct;15(5):1005-13. doi: 10.1097/01.gme.0b013e318166904e. PMID: 18779682; PMCID: PMC2810543.
Yeh SC, Chang MY. The effect of Qigong on menopausal symptoms and quality of sleep for perimenopausal women: a preliminary observational study. J Altern Complement Med. 2012 Jun;18(6):567-75. doi: 10.1089/acm.2011.0133. Epub 2012 Apr 26. PMID: 22537466.
Xia R, Qiu P, Lin H, Ye B, Wan M, Li M, Tao J, Chen L and Zheng G (2019) The Effect of Traditional Chinese Mind-Body Exercise (Baduanjin) and Brisk Walking on the Dorsal Attention Network in Older Adults With Mild Cognitive Impairment. Front. Psychol. 10:2075. doi: 10.3389/fpsyg.2019.02075
Nayak, Gayathry; Kamath, Asha1; Kumar, Pratap N.2; Rao, Anjali3,. Effect of yoga therapy on physical and psychological quality of life of perimenopausal women in selected coastal areas of Karnataka, India. Journal of Mid-life Health 5(4):p 180-185, Oct–Dec 2014. | DOI: 10.4103/0976-7800.145161
Menopause Yoga Nidra for disturbed sleep and low mood | Health & Her [YouTube]
What You Should Know About Relaxation Techniques for Hot Flashes | The Menopause Society
Paced Respiration for Hot Flashes? | The Menopause Society
Cognitive Behaviour Therapy (CBT) for Menoapusal Symptoms | Women’s Health Concern
An In-depth Look at the Definition of Mindfulness from Jon Kabat-Zinn | Mindfulness Based Happiness
Meditation and Mindfulness: What You Need To Know | National Center for Complementary and Integrative Health
Mindfulness may ease menopausal symptoms | Mayo Clinic
About Guided Imagery | Images of Wellness
Hypnosis | National Center for Complementary and Integrative Health
Nonhormonal management of menopause-associated vasomotor symptoms: 2015 position statement of The Menopause Society. Menopause: The Journal of The Menopause Society
Vol. 22, No. 11, pp. 000-000 DOI: 10.1097/GME.0000000000000546
Elkins GR, Fisher WI, Johnson AK, Carpenter JS, Keith TZ. Clinical hypnosis in the treatment of postmenopausal hot flashes: a randomized controlled trial. Menopause. 2013 Mar;20(3):291-8. doi: 10.1097/gme.0b013e31826ce3ed. PMID: 23435026; PMCID: PMC3556367.
Elkins G, Marcus J, Stearns V, Perfect M, Rajab MH, Ruud C, Palamara L, Keith T. Randomized trial of a hypnosis intervention for treatment of hot flashes among breast cancer survivors. J Clin Oncol. 2008 Nov 1;26(31):5022-6. doi: 10.1200/JCO.2008.16.6389. Epub 2008 Sep 22. PMID: 18809612; PMCID: PMC2652097.
Find a Certified Professional | American Society of Clinical Hypnosis
CBT for menopause | Health & Her
Cognitive behavior therapy shown to improve multiple menopause symptoms | The Menopause Society
Find a CBT Therapist Directory | Association for Behavioral and Cognitive Therapies
Find a Cognitive Behavioral Therapist (CBT) | Psychology Today
Find a Certified CBT Therapist | Academy of Cognitive and Behavioral Therapies
Koçak, Derya Yüksel PhD; Varişoğlu, Yeliz PhD. The effect of music therapy on menopausal symptoms and depression: a randomized-controlled study. Menopause 29(5):p 545-552, May 2022. | DOI: 10.1097/GME.0000000000001941
How Listening to Music Can Take the Edge Off the Menopause Transition | The Menopause Society
Jalambadani Z. The Effectiveness of Mindfulness-Based Art Therapy (MBAT) on Healthy Lifestyle in Iranian Menopausal Women. J Lifestyle Med. 2020 Jan 31;10(1):44-48. doi: 10.15280/jlm.2020.10.1.44. PMID: 32328447; PMCID: PMC7171058.
Art Therapist Locator | American Art Therapy Association
The role of soy isoflavones in menopausal health: report of The Menopause Society/Wulf H. Utian Translational Science Symposium in Chicago, IL (October 2010) Menopause: The Journal of The Menopause Society. Vol. 18, No. 7, pp. 732/753, DOI: 10.1097/gme.0b013e31821fc8e0
Is soy safe for cancer patients? | Dana-Farber Cancer Institute
Mediterranean Diet 101: A Meal Plan and Beginner’s Guide | Healthline
Menopause Weight Gain Is Common. Here’s How To Avoid It | Right as Rain by UW Medicine
Kapoor E, Collazo-Clavell M, Faubion S. Weight Gain in Women at Midlife: A Concise Review of the Pathophysiology and Strategies for Management. Mayo Clinic Proceedings Concise Review for Clinicians. 2017. Volume 92, Issue 10, P1552-1558. https://doi.org/10.1016/j.mayocp.2017.08.004
Adult Health | Mayo Clinic
Smith RL, Flaws JA, Gallicchio L. Does quitting smoking decrease the risk of midlife hot flashes? A longitudinal analysis. Maturitas. 2015 Sep;82(1):123-7. doi: 10.1016/j.maturitas.2015.06.029. Epub 2015 Jun 22. PMID: 26149340; PMCID: PMC4546860.
14 Reasons Why Walking Is One of the Best Forms of Exercise | GoodRx Health
Regular Walking May Protect Against Heart Failure Post Menopause | American College of Cardiology
The secret to mindful travel? A walk in the woods | National Geographic
Arnot M, Emmott EH, Mace R (2021) The relationship between social support, stressful events, and menopause symptoms. PLoS ONE 16(1): e0245444. https://doi.org/10.1371/journal.pone.0245444
Yale University. Stress May Cause Excess Abdominal Fat In Otherwise Slender Women, Study Conducted At Yale Shows. ScienceDaily. ScienceDaily, 23 November 2000.
History of MBSR | MBSR Teachers Collaborative of Greater New York
Carmody JF, Crawford S, Salmoirago-Blotcher E, Leung K, Churchill L, Olendzki N. Mindfulness training for coping with hot flashes: results of a randomized trial. Menopause. 2011 Jun;18(6):611-20. doi: 10.1097/gme.0b013e318204a05c. PMID: 21372745; PMCID: PMC3123409.
Mintziori G, Lambrinoudaki I, Goulis D, Ceausu I, Depypere H, Erel C, Pérez-López F, Schenck-Gustafsson K, Simoncini T, Tremollieres F, Rees M. EMAS position statement: Non-hormonal management of menopausal vasomotor symptoms. Maturitas 81 (2015) 410-413.
Complementary medicine options for menoapusal symptoms | Australian Menopause Society
What does NCCIH do? | National Center for Complementary and Integrative Health
Find a Practitioner | The Institute for Functional Medicine®
Find an ND | American Association of Naturopathic Physicians







