Feeling new joint pain even though you haven’t had an injury or changed your physical activity routine? Don’t have as much muscle strength as a few years ago?
If you’re on the menopause journey, you may have the musculoskeletal syndrome of menopause (MSM), a lesser-known but common set of symptoms that more than 70% of women+ experience during the hormonal transition. It’s caused by the natural decline in estrogen seen during this stage of life. MSM can show up as joint pain, muscle weakness, inflammation, and even loss of bone density. Let’s dive into what MSM is, who’s most at risk, and what you can do to manage it.
What Is Musculoskeletal Syndrome of Menopause (MSM)?
MSM is an umbrella term for the aches, pains, and other musculoskeletal changes that occur during the menopause journey.
Why does it happen? Like many other health conditions during the menopause journey, it’s due to falling estrogen levels. This hormone plays a critical role in maintaining healthy bones, muscles, and joints.
When estrogen decreases, it can lead to:
- Joint pain (Arthralgias): most commonly in the knees, hips, or shoulders
- Loss of Muscle Mass and Strength (Sarcopenia): On average, post-menopausal women have a 0.6% reduction in muscle mass per year. And a recent study by Johns Hopkins indicates sarcopenia increases the risk of dementia.
- Bone Thinning (Osteopenia) and Bone Loss (Osteoporosis): In perimenopause, women have an average reduction of bone density by 10%. Osteoporosis can increase the risk of falls and fractures.
- Tendon and Ligament Injury
- Frozen Shoulder (Adhesive Capsulitis): pain and stiffness in your shoulder usually due to inflammation. It limits your ability to move your arm.
About 70% of menopausal women experience musculoskeletal symptoms. So, it’s a fairly common symptom, yet it just received a name recently! The new terminology was established in 2024 due to the research conducted by Dr. Vonda Wright, an orthopedic sports surgeon and Associate Professor of Orthopedic Surgery at the University of Central Florida School of Medicine (UCF SOM).
Why you should manage those aches and pains
Here’s why it matters. It’s not simply about discomfort and feeling aches and pains.
25% of women+ may face significant disability without intervention.
Without proper management, MSM can have lasting impacts, including:
- Osteoarthritis/Progression of Osteoarthritis: a degenerative joint disease that occurs when the cartilage and bone in a joint break down over time; the incidence of osteoarthritis increases during the menopause journey
- Frailty: Muscle loss combined with bone fragility increases the risk of falls and fractures.
- Reduced Mobility: Persistent pain and weakness can diminish independence.
We get it – nobody wants to deal with these aches and pains! And we’ve been there where the pain changes our mindset about our ability to exercise. Don’t let MSM win because the long-term consequences can be debilitating. You can do something about the pain!

What can you do?
Here’s the good news: you don’t have to suffer through MSM! There are many steps you can take to prevent some of the symptoms and/or several ways to manage it.
You can focus on your lifestyle and get medical care.
Lifestyle
Don’t underestimate the power of lifestyle changes in how you feel, especially during the menopause journey.
Take small steps to make a positive difference in your well-being. If you need support, join pausitive health and become empowered with information, tools, and a community of women+ supporting each other on the menopause journey.
1. Get Moving
We understand the temptation is not to move as much when you’re feeling aches and pains. But it’s the best thing you can do!
Staying active reduces stiffness and inflammation.
Try exercises that improve muscle mass and bone density like:
- strength training
- yoga
- weight-bearing exercises
Some exercises should be avoided if you already have osteoporosis, but many others can reduce the risk of falls and fractures. Watch these exercise videos from a pausitive health fitness expert.
2. Eat Well
Ever heard of food as medicine? It really can play as important a role as medicine during the menopause journey.
Load up on bone-friendly foods rich in:
- calcium (like dairy and leafy greens)
- vitamin D
- protein
Adding magnesium and vitamin K2 to your diet can support both muscle and bone health.
Additionally, healthy eating helps with reaching and maintaining a healthy weight. Carrying extra weight can make joint pain worse.
Being just 10 pounds overweight puts an extra 15 to 50 pounds of pressure on your knees. This makes it more likely to you’ll develop osteoarthritis (OA) or increase its progression if you already have it.
Source: Arthritis Foundation

Boost Energy & Banish Cravings
Save 10% off MenoWell Menobars
Amp up your nutrition with these energy and protein bars! They provide many of the things important to eat during your menopause journey – protein, fiber, and gut-supporting prebiotics. The bars are vegan, gluten-free, dairy-free, low-carb, and low in added sugars.
Control your cravings and help manage your weight with these convenient bars that come in flavors like the best-selling Double Chocolate Brownie.
This is an affiliate link. We may earn a small commission if you access these services. The companies we work with are carefully vetted. However, we do not guarantee their products or services.
3. Consider Vitamin Supplementation
If you have vitamin D deficiency, supplementation may be necessary. Also, magnesium (500 mg daily) may help increase vitamin D levels.
A recent study found 1000 IU of vitamin D3 for 9 months was associated with reduced bone turnover markers and bone loss in post-menopausal women.
4. Quit smoking and limit alcohol consumption.
It’s never too late to stop unhealthy habits. Recent studies show there’s no safe level of alcohol especially for women.
There are many new alcohol-free beers and wines. You still want to drink these in moderation, but you may try one to help limit your consumption of alcohol.

Clinical Options
Talk with your doctor about your options to manage and treat the pain. That being said, medical gaslighting is a real concern. When you add the menopause journey and a complaint of chronic pain, the likelihood is even greater.
Musculoskeletal syndrome of menopause only became a named medical condition in 2024. So, your provider may not make the connection to the menopausal journey.
If your provider dismisses your concerns, it may be time to get a second opinion or a new healthcare provider. Many doctors do not receive sufficient training about the management of the menopause journey, so you must advocate for yourself so you can make a change for the better!
1. Consider Menopausal Hormone Therapy (MHT)
MHT can replenish estrogen, alleviate joint pain and slow bone loss. Talk to your doctor to see if it’s right for you. (It’s also important to note that if you are on hormone therapy and it is suddenly stopped, inflammation and joint pain may increase.)
2. Physical Therapy
Physical therapy can work wonders for chronic pain, stiffness, or post-fracture recovery. Tailored programs focus on improving strength, flexibility, and balance to prevent falls.
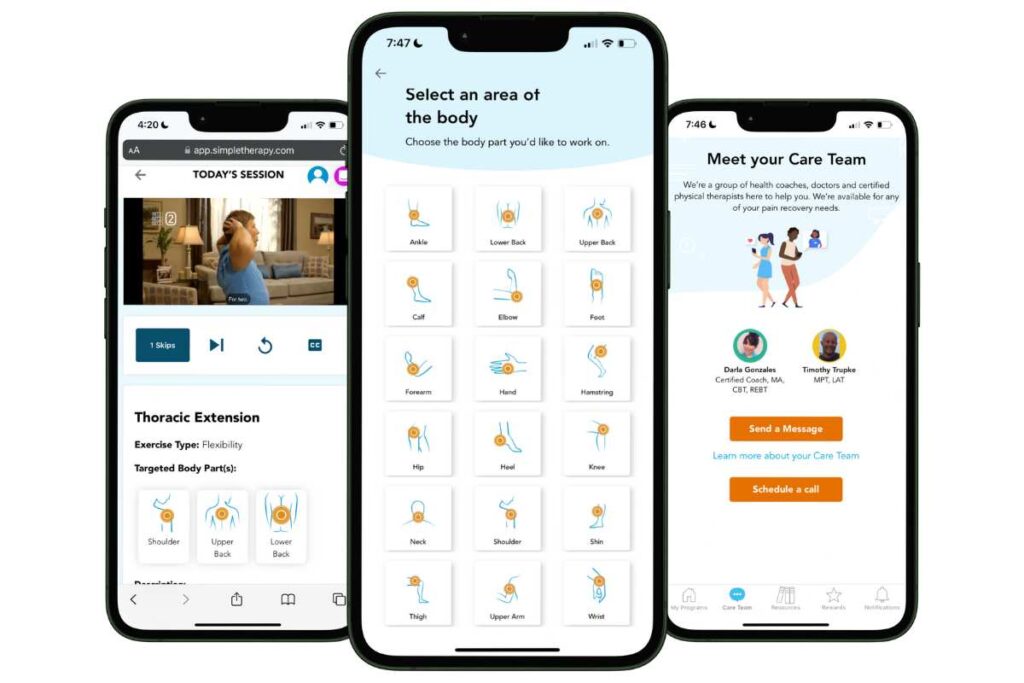
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!
3. Medications
NSAIDs (e.g., ibuprofen, naproxen) can help with pain relief and inflammation. However, it’s important to check with your healthcare practitioner about appropriate dosing, risks of bleeding (which can increase if you drink alcohol), and any conditions you might have for which NSAIDs would not be safe to take.
If you have osteoporosis, you might be prescribed medications like (a) biphosphonates, which help prevent bone breakdown, or (b) selective estrogen receptor modulators (SERMs), which mimic the protective effects of estrogen on bones.
Who’s Most at Risk for MSM?
The musculoskeletal syndrome of menopause (MSM) can affect anyone on the menopause journey, but certain factors make it more likely. These include:
- Age: Symptoms typically begin during perimenopause and extend into the post-menopause stage of the journey.
- Genetics: A family history of osteoporosis or arthritis increases your risk.
- Lifestyle: Sedentary habits, smoking, alcohol use, and poor diet can worsen symptoms.
- Race/Ethnicity: White and Asian women are more prone to osteoporosis due to lower baseline bone density.
Additionally, disparities in care are seen that can increase the risk of the consequences of MSM healthcare providers may overlook MSM symptoms in women of color or fail to provide adequate education.
Black and Hispanic women/Latinas tend to develop symptoms later but often face delays in diagnosis and treatment. They are often also diagnosed with osteoporosis at later stages, making treatment more challenging.
And women+ in underserved areas are less likely to receive/have access to bone density scans, physical therapy, and treatment like menopausal hormone therapy (MHT).
Don’t suffer in silence
While MSM can be uncomfortable, you don’t have to suffer in silence! Treatment options are available, including through the pausitive health program.
Be an advocate for yourself. While there is now a name for these aches and pains felt during the menopause journey, there are well-documented issues with women frequently being subjected to medical gaslighting.
Know that there are options, and you can take action to improve how you feel!
Losing muscle may increase risk of developing dementia | Healthline Media
Wright, V. J., Schwartzman, J. D., Itinoche, R., & Wittstein, J. (2024). The musculoskeletal syndrome of menopause. Climacteric, 27(5), 466–472. https://doi.org/10.1080/13697137.2024.2380363
Noel SE, Santos MP, Wright NC. Racial and Ethnic Disparities in Bone Health and Outcomes in the United States. J Bone Miner Res. 2021 Oct;36(10):1881-1905. doi: 10.1002/jbmr.4417. Epub 2021 Oct 7. PMID: 34338355; PMCID: PMC8607440.
How Fat Affects Osteoarthritis | Arthritis Foundation
Vázquez-Lorente H, Herrera-Quintana L, Molina-López J, Gamarra-Morales Y, López-González B, Miralles-Adell C, Planells E. Response of Vitamin D after Magnesium Intervention in a Postmenopausal Population from the Province of Granada, Spain. Nutrients. 2020 Jul 30;12(8):2283. doi: 10.3390/nu12082283. PMID: 32751522; PMCID: PMC7468838.
Nahas-Neto J, Cangussu LM, Orsatti CL, Bueloni-Dias FN, Poloni PF, Schmitt EB, Nahas EAP. Effect of isolated vitamin D supplementation on bone turnover markers in younger postmenopausal women: a randomized, double-blind, placebo-controlled trial. Osteoporos Int. 2018 May;29(5):1125-1133. doi: 10.1007/s00198-018-4395-y. Epub 2018 Feb 15. PMID: 29450585.
Martin-Key, N.A., Funnell, E.L., Spadaro, B. et al. Perceptions of healthcare provision throughout the menopause in the UK: a mixed-methods study. npj Womens Health 1, 2 (2023). https://doi.org/10.1038/s44294-023-00002-y
Gender Disparities in Pain and Pain Care | Southern Pain Society
You may also like…

28 At-Home Osteoporosis Exercise Videos To Help Prevent or Manage It
Try these at-home osteoporosis exercise videos from our collaborative partner. They can help prevent or manage osteoporosis and osteopenia.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

Weight Gain in Menopause Have You Down? Try These 9 Lifestyle Changes
Have you noticed your clothes getting tighter as you age? Weight gain is common in menopause. Learn how to lose weight and feel better.

