Since your menopause journey started, have you noticed seemingly unrelated symptoms, like urine or stool leakage, constipation, pelvic discomfort, or back pain? You may be one of the many women+ suffering from a weak or tight pelvic floor. While some of the symptoms can be embarrassing, you don’t have to suffer in silence. Get started with pelvic floor rehab options. Try these 9 treatment options to get relief from pelvic floor dysfunction!

Treatment for pelvic floor dysfunction
Pelvic floor dysfunction doesn’t go away by itself. In fact, if left untreated, it usually gets worse over time.
Luckily, there are many different options to manage your symptoms:
1. Consult with a urogynecologist.
A urogynecologist is a specialist who focuses on pelvic floor conditions. You may want to speak with your PCP about a referral to determine the type of work-up you might need and the best course of action to address your symptoms.
Learn more about pelvic floor issues from guest contributor K. Lauren de Winter, MD, FACOG, URPS of Praxis Urogynecology. She discusses bladder and vagina symptoms during the menopause journey and possible treatment options during a pausitive health webinar.
2. Pelvic floor rehab
As strange as it sounds, there is physical therapy (PT) specifically for your pelvic floor. But exactly what is pelvic floor PT?
Like all PT, your sessions are highly individualized based on your needs and specific symptoms. Depending on the type of problem you have, it can involve exercises, stretches, and other forms of therapy to help strengthen and/or relax your pelvic floor muscles.
Pelvic floor PT can also help you gain better coordination of your pelvic floor muscles so you can more easily control them. In turn, you will be better able to manage symptoms like leakage or constipation.
At-home Kegels
Many of the exercises are simple, do not involve equipment, and can be performed at home.
A common example of an easy, equipment-free exercise is Kegels, which are exercises used to strengthen pelvic floor muscles. Once you get the hang of it, they are simple and can be done anywhere.
- Step 1: Squeeze the muscles in your rectum that you would use to stop gas from passing. You also want to squeeze your vaginal muscles as if you’re gripping an inserted tampon.
- Step 2: Hold this position for 3 seconds.
- Step 3: Repeat 10 to 15 times. This can be done several times a day.
You can also work your way up to being able to hold one Kegel for 10 seconds, or stopping your urine mid-stream.
Other exercises to strengthen your pelvic floor
There are many exercises beyond Kegels that could help. Some involve using equipment like bands and balls. Adding this type of resistance could help improve your urinary symptoms even more.
It’s important to be patient. Strengthening your pelvic floor takes time. So, you may not notice improvement right away. Speak to your physical therapist about your goals and how long it may take.
It’s important to get guidance about the type of pelvic floor PT you need. For example, if you have issues with pelvic floor spasms, Kegel exercises could actually make things worse. Pelvic floor massage would be a more appropriate approach.
When you become a pausitive health member, you’ll get access to a pelvic floor program with online modules to lead you through exercises.
Plus, the first 100 enrollees in this pelvic floor program will have access to a virtual consultation with a physical therapist trained in pelvic floor issues. Everyone has access to online modules to lead you through exercises. Get access today!
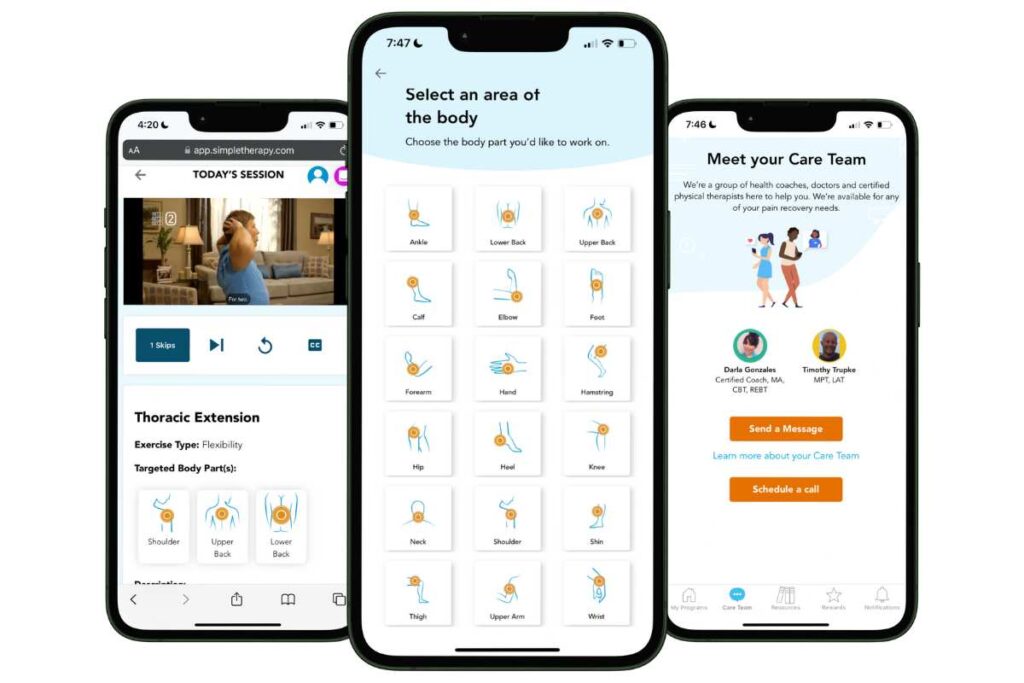
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!
3. Pelvic floor massage
Pelvic floor massage is another technique your physical therapist may try.
There are many muscles that make up your pelvic floor. And any of them could be tight. So, it’s important to be open about all your symptoms to help your physical therapist target the right muscles for you.
They may use internal and external techniques to help loosen and relax your pelvic floor muscles.
The massage can help with:
- pain
- bladder control
- sexual satisfaction
- pelvic floor spasm
If you find the pelvic floor massages beneficial, many of the techniques can be done at home. Some may involve equipment like a ball or pelvic floor wand.
4. Biofeedback
Biofeedback is a therapy usually done as an add-on to pelvic floor physical therapy. It involves using equipment that gives visual and audible feedback during certain exercises.
It’s usually used for people with bowel dysfunction symptoms, like stool incontinence, constipation, or rectal pain. But it can also be used for people with stress urinary incontinence.
It not only helps you gain strength, but it helps improve your muscle coordination and sensitivity. So, you can more easily detect when urine or stool is present. And you can better control your muscles to prevent urgency.
While PT alone can help your symptoms, doing a combination of PT and biofeedback has been shown to be even more effective in improving your muscle strength and endurance.

5. Vaginal Dilators
For those who experience pain during penetrative sex related to pelvic floor dysfunction, a dilator regimen may help.
Dilators are tubes of gradually increasing sizes that are used to improve the flexibility of your vaginal walls and the strength of your pelvic muscles.
Although they can be purchased without a prescription and used at home, you may want guidance from a healthcare practitioner like a physical therapist who specializes in pelvic floor dysfunction. They can help:
- Ensure you are using the correct insertion technique and dilator sizes.
- Advise how quickly to graduate to a larger size and determine if additional therapies are indicated.
- Reduce the risk of injury.
6. Vaginal hormone therapy
Vaginal estrogen is the most common hormone therapy (HRT) studied for pelvic floor dysfunction.
While it can improve urinary incontinence symptoms, it does not help with pelvic organ prolapse (POP).
But your doctor may prescribe it before or after certain procedures. It can help improve your thin, dry vaginal tissue before surgery. And it can reduce urinary symptoms after certain urinary tract surgeries.
Other forms, e.g., oral medication, of hormone therapy are generally not recommended for pelvic floor dysfunction. They tend to have more overall side effects and are less studied.
7. Local injections
When other options have not worked to improve pelvic pain, your doctor may consider local injections, called trigger point injections.
Usually, a combination of numbing medication and a steroid is injected into a specific muscle in your pelvic floor. This helps that muscle relax and numb the pain.
About 3 out of 4 women experience a reduction in pain. And about 1 in 3 become pain-free with this technique.
Unfortunately, this procedure is not a cure and needs to be repeated about every 3 months.
8. Medications
Speak with your healthcare practitioner. Depending on your symptoms, your doctor may recommend medication that could help with your symptoms.
These include:
Anticholinergics
Anticholinergics block a chemical in your body called acetylcholine. Acetylcholine tells the muscles in your bladder to contract. So, blocking acetylcholine can help reduce urinary urgency.
This group of medications includes oxybutynin (Ditropan) and tolterodine (Detrol).
Myrbetriq or Gemtesa
These two medications help relax the bladder so it can hold more urine.
Certain types of antidepressants
Certain types of antidepressants, e.g., imipramine (Tofranil), make the bladder muscle relax, while causing the smooth muscles at the bladder neck to contract. This dual effect can help prevent leaks.
Botox
If other options have failed, your doctor may recommend trying Botox. The medication is injected it into different parts of the bladder or urethra. This helps relax the muscles and lessen urinary urgency.
Unfortunately, this procedure needs to be repeated every 3 months.
Keep in mind, medications usually only treat the symptoms of pelvic floor dysfunction. They do not cure your pelvic floor disorder.
9. Lifestyle Actions
You can try several lifestyle actions to relieve pelvic floor pressure, strengthen your pelvic floor, and improve your symptoms.
These include:
- Exercise in general, using the physical activity guidelines from the Office of Disease Prevention and Health Promotion
- Loss of excess body weight
- Deciding to quit smoking
- Scheduling bathroom breaks regularly throughout your day. Start at every 2 hours while awake
- Avoiding constipation by eating high-fiber foods and drinking enough water

10. Breathing exercises
Strengthening your pelvic floor can be as simple as breathing. Your pelvic floor and diaphragm are aligned and work together.
As you inhale, your diaphragm lowers to expand your lungs. Your pelvic floor relaxes and drops.
As you exhale, your diaphragm relaxes and moves up to push the air out of your lungs. Your pelvic floor then contracts and moves up.
What is kapalabhati?
Kapalabhati is a fast-paced breathing technique that has quick and intentional exhales. Since your breathing and pelvic floor are aligned, you’re rapidly contracting your pelvic floor muscles with each exhale.
Kapalabhati is often performed during different types of yoga. But it can also be done alone whenever it’s convenient for you.
Here is more information and guidance in how to do it from Yoga International.
Breathing exercises, like kapalabhati, can improve your urinary symptoms by strengthening your pelvic floor muscles.
Take control now
Don’t be embarrassed about your urinary, bowel, and sexual health. Many women+ just like you are experiencing the same struggles.
During a podcast with Peli Health, Dr. Z. Colette Edwards, Founder and Chief Medical Officer of pausitive health, spoke about pelvic health during the menopause journey and the emotional and energetic levels of pelvic wellness.
Remember you have options that could improve your symptoms and your quality of life. You can make a change for the better!
Home | Praxis Urogynecology
Kegel Exercises | National Institute of Diabetes and Digestive and Kidney Diseases
Step-by-step guide to performing Kegel exercises | Harvard Health Publishing
Kegel exercises: A how-to guide for women | Mayo Clinic
Vyas R, Hande D, Nishad P, Barot H. Effects of pelvic floor muscle training vs an assisted pelvic floor muscle training among rural perimenopausal women with urinary incontinence: A comparative study. International Journal of Yoga, Physiotherapy and Physical Education. 2018. Impact Factor: RJIF 5.24. Volume 3, Issue 1, Pages 121-124.
Hite M, Curran T. Biofeedback for Pelvic Floor Disorders. Clin Colon Rectal Surg. 2021 Jan;34(1):56-61. doi: 10.1055/s-0040-1714287. Epub 2020 Sep 4. PMID: 33536850; PMCID: PMC7843943.
Bertotto A, Schvartzman R, Uchôa S, Celeste Osório Wender M. Effect of electromyographic biofeedback as an add-on to pelvic floor muscle exercises on neuromuscular outcomes and quality of life in postmenopausal women with stress urinary incontinence: A randomized controlled trial. Neurourology Urodynamics. 2017. Volume 36, Issue 8, Pages 2142-2147. https://doi.org/10.1002/nau.23258
Bodner-Adler B, ALarab M, Ruiz-Zapata A, Latthe P. Effectiveness of hormones in postmenopausal pelvic floor dysfunction – International Urogynecological Association research and development – committee opinion. International Urogynecology Journal. 2020 31:1577-1582.
Rahn DD, Good MM, Roshanravan SM, Shi H, Schaffer JI, Singh RJ, Word RA. Effects of preoperative local estrogen in postmenopausal women with prolapse: a randomized trial. J Clin Endocrinol Metab. 2014 Oct;99(10):3728-36. doi: 10.1210/jc.2014-1216. Epub 2014 Jun 20. PMID: 24947034; PMCID: PMC4184065.
Rahn, D.D., Ward, R.M., Sanses, T.V. et al. Vaginal estrogen use in postmenopausal women with pelvic floor disorders: systematic review and practice guidelines. Int Urogynecol J 26, 3–13 (2015). https://doi.org/10.1007/s00192-014-2554-z
Langford CF, Udvari Nagy S, Ghoniem GM. Levator ani trigger point injections: An underutilized treatment for chronic pelvic pain. Neurourol Urodyn. 2007;26(1):59-62. doi: 10.1002/nau.20393. PMID: 17195176.
Bladder control: Medications for urinary problems | Mayo Clinic
What’s the Best Medication for Overactive Bladder? | GoodRx Health
National Guideline Alliance (UK). Risk factors for pelvic floor dysfunction: Pelvic floor dysfunction: prevention and non-surgical management: Evidence review B. London: National Institute for Health and Care Excellence (NICE); 2021 Dec. (NICE Guideline, No. 210.)
Executive Summary: Physical Activity Guidelines for Americans 2nd Edition | U.S. Department of Health and Human Services
Water: How much should you drink every day? | Mayo Clinic
Malhotra V, Javed D, Wakode S, Bharshankar R, Soni N, Porter PK. Study of immediate neurological and autonomic changes during kapalbhati pranayama in yoga practitioners. J Family Med Prim Care. 2022 Feb;11(2):720-727. doi: 10.4103/jfmpc.jfmpc_1662_21. Epub 2022 Feb 16. PMID: 35360798; PMCID: PMC8963645.
Chandrasing Patil D, Honkalas P. The impact of kapalabhati on menopausal women’s pelvic floor muscle strength. 2022. The Journal of Community Health Management. 2022;9(4):178-182.
You may also like…

Is Your Pelvic Floor in Perimenopause Too?
Give your pelvic health some love in perimenopause. It’s more than Kegels. Get solutions to improve vaginal and sexual health, your bladder, and pelvic floor.

Pelvic Floor Rehab: 10 Treatment Options During the Menopause Journey
Pelvic floor symptoms can be embarrasing, but don’t have to be. Learn about pelvic floor rehab options. Get treatment that’s right for you.

Menopause Matters: Understanding Pelvic Floor (Bladder and Bowel) Symptoms
Your pelvic floor is the “forgotten core” but your body may remind you of this area during the menopause journey, with bladder and bowel symptoms.

