Dry, itchy skin is one of those symptoms that may leave you scratching your head – is it menopause, an allergy, the weather, or something else? It’s easy to attribute this menopause symptom to something else. But, it’s a common symptom, and it’s time women find relief. Try these 8 options to relieve your dry, itchy skin.
Types of menopause itching
In a 2018 survey study, 72% of women experienced skin changes during perimenopause and menopause. Changes included dryness, wrinkles, and itchy skin. Some women+ also experience acne.
Your doctor may refer to the itching by the medical term, pruritus, which can range from generally mildly itchy skin to prickly, itchy skin that feels like it’s burning.
The itch can occur from head to toe, including your scalp.
Many women say the itch can wander and affect different parts of the body. Sometimes it might just be your arms and/or your legs. But menopause-related itchy skin can also show up as itchy armpits, an itchy vagina and genital area, or an itchy face and scalp.

Vulvar and menopause vaginal itching
During the menopause journey, many women develop a condition called genitourinary syndrome, or GSM. GSM symptoms generally fall into three main areas – general, sexual, and urinary. Among general symptoms, women can experience dryness, intense vaginal itching, and discomfort. Some say it can feel like burning or sandpaper. These sensations are related to thinning, dryness, and inflammation of the vaginal (internal) and vulvar (external) areas of the genital area of the body.
Besides GSM, there are several other potential causes of vaginal or vulvar itching, including vulvar cancer (rare) and ones related to an infection like yeast, bacterial vaginosis (BV), and some sexually-transmitted diseases. It’s important to check with your healthcare provider to make sure you get the appropriate treatment.
For example, if your itching is related to menopause, a hormonal cream may be prescribed, but for BV an antibiotic would be the treatment.
Itching at night
Menopause-related itching and burning can happen during the day, or it might wake you up in the middle of the night (if you’re not already awake due to other menopause-related symptoms, like sleeplessness, leg pain, restless leg syndrome, or night sweats.)
Additionally, at night if your environment becomes quieter and your body becomes more relaxed, you may become hyper-aware of things you might not notice as much, if at all, during the day when you are on the go.
Eczema
You may get eczema for the first time during menopause or it may return from years prior. These flare-ups are typically milder, according to the American Academy of Dermatology Association.
It may also look different as an adult. The skin is typically extremely dry and scaly and may appear in different areas. You may find it on the backs of your knees, crooks of your elbows, back of the neck, face, or eyes.
A dermatologist can help diagnose eczema, and the type, of which there are many.
The peak time for developing adult-onset atopic dermatitis coincides with menopause in your 50s.
Causes of itchy skin
As with most of the symptoms of menopause, there are several causes of dry and/or itchy skin. They are wide-ranging and include:
- pH skin changes
- hormones
- environmental factors (e.g., dry air, windy, and cold climates)
- skin conditions like eczema and psoriasis
- medications (e.g., acne medications, statins, and diuretics)
- certain chemotherapy and radiation therapy regimens,
- harsh skin products
- medical condition, including liver disease, bile duct issues, kidney disease, diabetes, skin cancer, leukemia, and lymphoma, and vulvar cancer (rare)
- genital infections like yeast, bacterial vaginosis (BV), and some sexually-transmitted diseases.
Hormonal changes
The thickest layer of your skin, called the dermis, is sensitive to shifts in hormones. Estrogen helps your skin produce oil and hold on to the water, both of which help your skin remain plump. As estrogen levels fall and the skin becomes drier, itching follows.
So, it’s no surprise itchy skin happens during the menopause journey. Blame it on the declining levels of estrogen experienced during the transition.
Estrogen helps your skin produce oil and hold on to water, both of which help your skin remain plump. As estrogen levels fall and the skin becomes drier, itching follows.
pH changes
Also, your skin’s pH level changes around age 50 which is also around the time of menopause. That change makes your skin more sensitive and irritated.
Reduced collagen production
When a woman’s estrogen levels start to drop during perimenopause, and even further at menopause and post-menopause, there is also an impact on the body’s ability to produce collagen. It’s a protein that helps hold together cells in the body and provides structure to connective tissue. It is found in muscles, bones, and tendons and is responsible for the elasticity of the skin.
Your body can lose nearly 30% of its collagen in the first five years after menopause. As a result, skin can become quite dry. And dry skin often becomes itchy skin.
Treatment may vary depending on the cause
Check with your healthcare provider to determine if your skin changes are related to hormonal changes of the menopause journey or something else. The cause can change the treatment.
For example, if your itching is related to menopause, a hormonal cream may be prescribed, but for BV an antibiotic would be the treatment.

8 ways to care for dry, itchy skin during menopause
During perimenopause and menopause, as well as post-menopause, a good home and lifestyle routine can help provide relief and help you manage skin dryness and itchiness.
1. Shift from hot to warm showers or baths.
Hot showers strip your skin of natural oils, so keep your showers or baths short and use warm instead of hot water. Then, moisturize!
Moisturize, moisturize, moisturize. Moisturize immediately after you towel off, as your skin can better absorb our moisturizer of choice at that time due to greater skin permeability (the state or quality of a membrane that causes it to allow liquids pass through it) related to the warm temperature of the water. In general, ointments and creams tend to work better for dry or cracked skin because they have a higher content of oil compared to a lotion or a gel, which have a much higher concentration of water.
Moisturize daily and throughout the day. Try to find a moisturizer with hyaluronic acid or squalene, which can help hold in water and keep skin supple.
Some women also find that serums and creams with antioxidants like vitamin C help with dryness on their face and chest.
Moisturizers with ceramides can keep moisture from escaping. There are 12 different types of ceramides, so you may want to see a dermatologist to help figure out the best ones to use in your situation. For example, some types may work well on your face but not on your body.
If your scalp feels dry, use a gentle, co-wash or moisturizing shampoo, try to wash your hair less often, and tend towards warm rather than hot water.

Soothe Dry Itchy Skin
Shop a safe, gentle, clinically-proven line of skincare designed specifically for the unique needs of people with the most compromised skin. While originally designed to help cancer patients, Lindi Skin products can also help with aging and menopausal skin that’s dry, itchy, and sensitive. A portion of each sale helps those fighting cancer. Use code “pausitive“ for at least 10% off.
This is an affiliate link. We may earn a small commission if you access these services. The companies we work with are carefully vetted. However, we do not guarantee their products and services.

2. Clean your skin gently.
Even dry skin needs to be cleaned daily to remove the dirt that settles on your skin during the day. Also, remove makeup if you wear it.
The cleanser you use in your skincare routine can make a big difference in your skin’s “itchiness.” Unless your skin is oily, consider using a non-foaming, gentle cleanser specifically formulated for sensitive skin.
3. Start reading ingredient lists.
Avoid making dry skin worse with fragrances, colors, retinoids, alpha-hydoxy acid (AHA), and alcohol that can be drying. Sadly, if it smells good, it’s often the case it might not be great for your skin.
4. Make tweaks to your lifestyle and environment.
In addition to carefully selecting shampoos, cleansers, and skin care products and adjusting how you care for your skin, there are some steps you can take to help decrease dryness and your level of itchiness and give you some relief, including:
- Stay sufficiently hydrated, including increasing your intake of water and foods that have a higher water content, like cucumbers, watermelon, grapes, oranges, grapefruit, pineapple, strawberries, blueberries, cantaloupe, lettuce, zucchini, tomatoes, celery, bell peppers, and cabbage.
- Stop smoking (or don’t start in the first place!).
- Get enough (7 – 9 hours) high-quality sleep. Try these day-and-night mind-body remedies. If you regularly skimp, besides being tired, the lack of sufficient sleep decreases the barrier function of the skin leading to more water loss, which in turn leads to drier skin.
- Use a humidifier, especially during seasons like the winter when skin (and nails) tend to be drier.
- Discuss potentially using supplements that are important to skin health and help with dry skin – vitamin C, vitamin D, fish oil – with your healthcare provider.
- Consider using oils, creams, or lotions which contain vitamin E.
- Find effective ways to help with stress, e.g., physical activity, guided imagery, mindfulness, yoga, and music. Elevated stress levels trigger higher levels of cortisol which then can decrease collagen production.
5. Use a humidifier.
A humidifier puts moisture into the air, which can help reduce dry, itchy skin.
If a humidifier is not already included in your HVAC system, and you don’t have an interest in, the budget for, or live in a building where that is not an option, then a room humidifier may be a good option.
There are two types.
| Type of Humidifier | Pros | Cons | Miscellaneous |
|---|---|---|---|
| warm mist |
• quieter • less expensive • can help reduce bacteria • can help warm the air during cold weather |
• higher energy consumption • hot steam a potential safety hazard (burn risk) |
• better suited to smaller rooms • use distilled water • do not add oils or VapoRub • avoid room humidity > 50% |
| cool mist |
• can be used year-round • safe for around children and pets |
• lower energy consumption<br > • louder • more likely to have growth of bacteria |
• can accommodate larger spaces • use distilled water • avoid room humidity > 50% |
6. Don’t scratch!
Try putting a cold compress on the area that itches, or wear gloves to bed to avoid scratching and to reduce the damage severe scratching can cause.
7. Use sunscreen and be judicious regarding sun exposure.
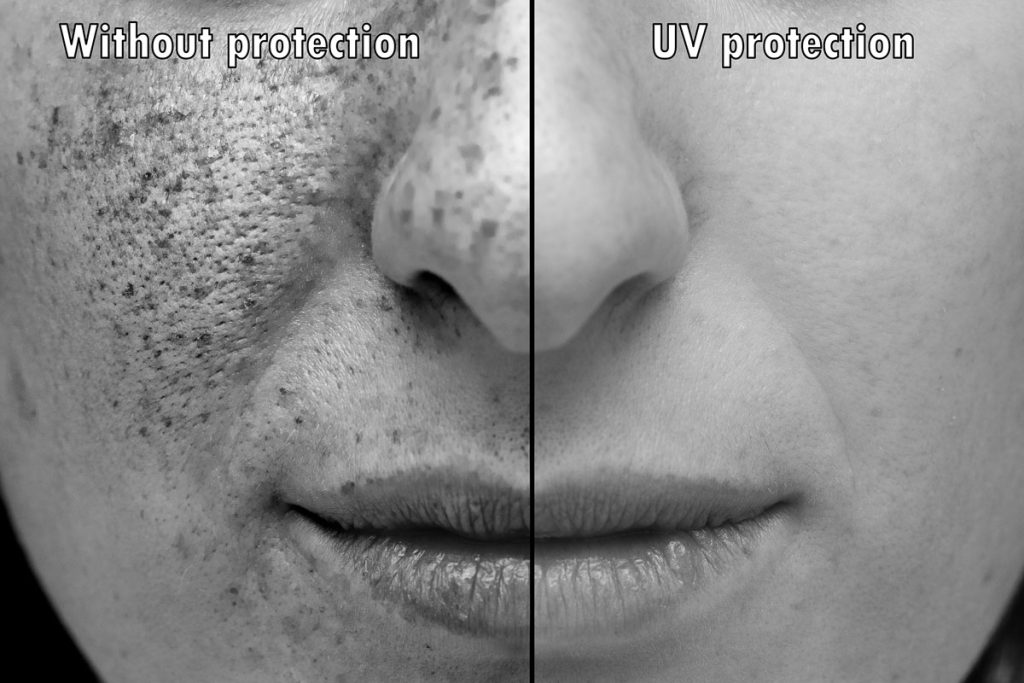
Sun exposure is one of the best sources of vitamin D and tends to boost our mood. However, unprotected sun exposure (to UV A and B radiation) of long duration – a long session at one time, e.g., tanning beds, and cumulative over the years – can dry out skin, make it flake, and lead to itchiness. (It also contributes to the development of wrinkles and leathery skin and increases the risk of skin cancer.)
Although those with lighter skin tones are at greater risk of sun damage (and those with red hair and light eyes are at greater risk of skin cancer), contrary to what you may have heard or read, the negative impacts of excessive, unprotected sun exposure can be experienced across all skin tones. And for women of color, a diagnosis of skin cancer is often delayed compared to white women, which means a greater likelihood of identification at a late stage of the disease, fewer treatment options, and a higher mortality rate. Women of color in this situation include Black, Asian, Latina, Mediterranean, Middle Eastern, and Indigenous women.
American Academy of Dermatology Association recommendations include:
- using sunscreen with an SPF of 30 or higher that protects against both UV A and IV B rays, is water-resistant, and isn’t past the expiration date
- avoiding tanning beds and sunlamps
- avoiding the sun between 10 am and 2 pm when the rays are the strongest
- being aware of environments that increase the reflection of the sun and, therefore the intensity of skin exposure – snow, sand, and water
- wearing sun-protective clothing
- making sure to cover all parts of the body with sunscreen, including the lips, your ears and neck, and the tops of your feet and head
- applying sunscreen at least 15 minutes before sun exposure and every two hours thereafter
- avoiding combination sunscreen + bug repellant products

8. Medication
There are several medications that can help relieve the dry, itchy skin of the menopause journey. They include:
- Hydrocortisone cream 1% – This is an OTC steroid that can come in handy for inflamed skin. If you need to use it on regular basis for more than two weeks, the general recommendation would be to see your healthcare provider. Long-term use can thin the skin, and you also want to make sure the case is not something else for which this treatment will not help or could actually be made worse.
- Prescription steroids – These products are stronger than steroids that can be purchased OTC. They must be prescribed and are available in several forms – aerosol, gel, cream, or lotion – based on the location and severity of the itching.
- Hormone therapy – Like prescription steroids, hormone therapy must be prescribed, and the formulation and mode of delivery will depend on the location and severity of the itching as well as other menopausal symptoms you may have.
Scratch less and pamper more
Leverage the knowledge you now have to set yourself up for a lifestyle and skin-care routine that will help reduce skin dryness and itching as well as the risk of sun damage and skin cancer.
Contacting your PCP when you have concerns and questions is a great first step. And if you have preexisting skin conditions like eczema, rosacea, or psoriasis, develop new skin changes, or have persistent or intense itching, you may need to see a dermatologist to help ensure an accurate diagnosis and the best treatment for your symptoms.
You have options that are under your control.
Take action now!
Skin and menopause: women’s point of view | Journal of the European Academy of Dermatology & Venereology
Itchy skin (pruritus) | Mayo Clinic
Collagen | Harvard T.H. Chan School of Public Health
About Bacterial Vaginosis | Centers for Disease Control and Prevention
Can You Get Eczema As An Adult? | American Academy of Dermatology Association
Eczema: Types and Treatment | American Academy of Dermatology Association
Caring For Your Skin in Menopause | American Academy of Dermatology Association
BC10: The impact of menopause on the skin and ageing process | British Journal of Dermatology
Dermatologists’ Top Tips for Relieving Dry Skin | American Academy of Dermatology Association
Oyetakin-White P, Suggs A, Koo B, Matsui MS, Yarosh D, Cooper KD, Baron ED. Does poor sleep quality affect skin ageing? Clin Exp Dermatol. 2015 Jan;40(1):17-22. doi: 10.1111/ced.12455. Epub 2014 Sep 30. PMID: 25266053.
Benefits of Using a Humidifier | MedicalNewsToday
Red Alert! | Skin Cancer Foundation
Sunscreen FAQs | American Academy of Dermatology Association
You may also like…

Menopause Hair Loss 101: What Causes It and 7 Ways To Support Hair Growth
Are you experiencing hair loss, changes in texture, or an itchy scalp? Find out why this is happening and how to manage this menopuase symptom.

Menopause Acne?! Why It Happens and How To Treat Your Skin
Do you have pimples on your face or torso in your 40s and 50s? Learn why menopause acne happens and how to treat it.

Menopause Is Just Like Being A Teenager Again, Except You’re Wiser For It
Menopuase is like a second adolescence, bringing back memories of acne, moodiness, and other teenage concerns. Learn how to navigate it!

