Were you looking forward to saying goodbye to the bodily fluids and discomfort associated with your periods? Only to have menopause hit and now you’re hit with a new set of issues like a vagina that feels dry, itchy, and inflamed? Then, there’s sex. For some women+, it’s painful and no longer enjoyable. If this sounds like you, you may have a common condition known as genitourinary syndrome of menopause (GSM). The good news is there are answers and treatments to address the problem, so don’t suffer in silence!
What is genitourinary syndrome of menopause (GSM)?
As much as this new, uncomfortable phase of menopause can come from out of left field, the medical terminology used to describe what you’re feeling “down there” won’t exactly roll off your tongue.
Your doctor may tell you that you have genitourinary syndrome of menopause (GSM) if you have pain in your vagina, vulva, pelvis, or urinary tract. Or if you have lower libido or pain during sex. There are a wide range of symptoms – genital, sexual, and urinary – that fall under the GSM umbrella.
GSM is a recently introduced term, as it more completely reflects the range of issues and symptoms related to the condition during the menopause journey.
Your vagina or vulva may feel itchy or irritated. While that may be the initial symptom, your genital tissue environment changes and can cause frequent UTIs or pain during sex.
The range and relationship between the symptoms is why GSM is a better characterization of this condition.
Symptoms of GSM
Studies suggest up to 50% of post-menopausal women+ experience GSM. That number is approximately 15% in women+ who are perimenopausal.
Symptoms of GSM can range from mild to intense. It can be challenging to diagnose because many women have mild symptoms, or their symptoms may be attributed to some other condition.
While many women+ will contact their provider if they have frequent urinary tract infections (UTIs), they may be reluctant or embarrassed to bring up issues related to their genital area or sexual well-being. But, GSM is a chronic and progressive condition so it’s important that you don’t delay treatment.
The National Institutes of Health (NIH) splits the most common GSM symptoms into three categories: genital, sexual, and urinary.
Genital symptoms can include:
- Vaginal dryness
- Burning or itching
- White, green, or yellow discharge
- Vaginal or pelvic pain and pressure
- Thinning or greying pubic hair
- Irritation from tight clothes or from sitting on a bike seat
- Paleness and thinning of the labia
Previously undiagnosed vaginal prolapse may also become apparent or more prominent due to a combination of tissue thinning in the vagina and less pelvic support.
Sexual symptoms can present as:
- Painful intercourse (dyspareunia)
- Bleeding or spotting after sex
- Reduced lubrication
- Less arousal during sex and/or loss of libido (sexual desire)
- Difficulty having an orgasm
- Pain during or after an orgasm (usually in the abdomen)
- Narrower, less elastic vagina
Urinary symptoms often present as:
- Painful urination
- Urgency (need to get to the bathroom quickly)
- Blood in the urine
- More frequent urinary tract infections (UTI)
- Stress/urgency incontinence
Your urethra and bladder have estrogen receptors. When estrogen declines as a result of the menopause transition, so do muscle mass and strength. And the dryness of GSM can make it easier for bacteria or yeast to enter your urinary tract.
These changes can result in urinary incontinence (leaking) and more frequent UTI’s than you experienced in prior years.
In the MsFLASH Vaginal Health Trial, of the 302 post-menopausal female participants, most women experienced multiple vulvovaginal symptoms, including:
- itching
- pain or soreness
- irritation
- dryness
- vaginal burning
These vaginal symptoms can be exacerbated during sex, with 80% of participants reporting at least one vaginal symptom during or after sex.
During a pausitive health webinar, Dr. K. Lauren de Winter talks about GSM and how hormonal changes impact the bladder, vagina, and pelvic floor muscles.
What causes it?
There are several potential causes for GSM, including:
- Menopause
- Infrequent/no sexual activity (with or without a partner)
- Medications (e.g., Tamoxifen, Provera, some birth control pills, anti-estrogen medication used to treat fibroids and endometriosis like Elagolix).
- Pelvic radiation for cancer
- Chemotherapy
- Smoking
- Breastfeeding
If the cause is related to a transient and short-term change in hormonal levels, GSM will correct itself after estrogen levels stabilize. If the issue is a longer term or permanent change in the hormonal profile, or related to another cause, then treatment will usually be needed to address symptoms and get relief.
It’s a complex condition, and symptoms can vary from person to person.
Why GSM is common in menopause
When your body goes through the menopause journey, your hormone levels shift, which results in physical changes to both your vagina (internal) and vulva (external).
One of the big hormonal shifts that happens is a drop in estrogen levels. Estrogen is a vital hormone produced in the ovaries. It stimulates the vagina to produce secretions and helps to protect the skin of your vulva.
During perimenopause, estrogen levels fluctuate and can be volatile, but overall, they head downward. Levels continue to fall into the post-menopause stage and ultimately trail off.
If you undergo surgical removal of your ovaries or are undergoing radiation therapy or chemotherapy, estrogen levels can plummet quickly instead of over several years. That can lead to an earlier onset of menopause.
If you have premature menopause (onset younger than age 40) or early menopause (onset older than age 40 but younger than 45), you may experience the symptoms of GSM earlier than the typical age when they would otherwise appear.
Vaginal atrophy – a symptom of GSM
While the condition is now called GSM, you may still hear the term vaginal atrophy if your vagina or vulva is the source of pain or discomfort.
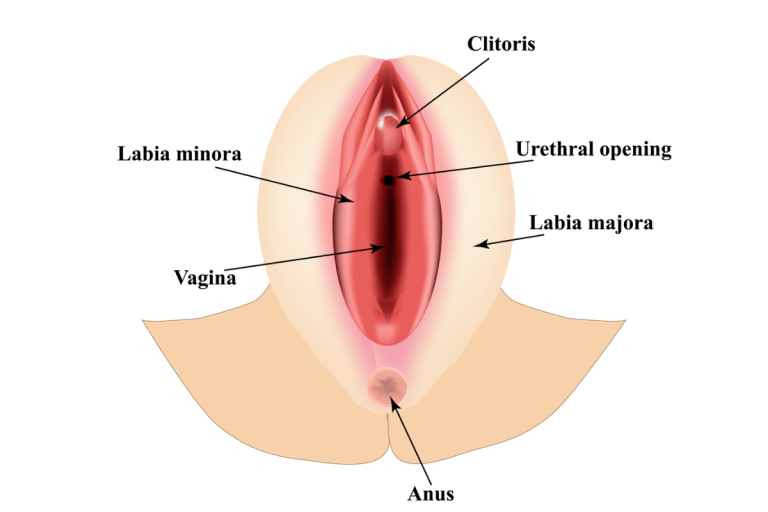
Your vagina refers to the internal area, and your vulva refers to the external area.
Vaginal atrophy is just one of the names you may hear. Your doctor may also describe your condition as:
- Atrophic vaginitis
- Vulvovaginal atrophy
- Urogenital atrophy
With names like these, you may be wondering what your doctor just said as much as you’re wondering what’s happening to your vagina.
Vaginal symptoms
According to an observational study the most common and bothersome symptom of vaginal atrophy is vaginal dryness, which affects 93% of women with the condition.
When your vagina is not well-lubricated, it can become irritated and even raw. This can manifest with varying degrees of severity, from mild discomfort to even pain when walking.
Causes of vaginal pain
As a result of the hormonal shift, the lining of your vulva (the labia majora, labia minora, and clitoris) and vagina becomes thinner, drier, and less flexible or supple.
Being sexually inactive can increase the likelihood of developing vaginal atrophy and also make it more severe because of decreased blood flow to the vagina.
It can be a chronic and progressive condition, meaning it can persist for a long time and often continues to worsen until you seek treatment.
GSM and orgasm
With wide-ranging symptoms, one of the signs of GSM may be painful sex. It can be upsetting for several reasons, not least of which may be more difficulty reaching orgasm, and who doesn’t love a good orgasm? We all love a good orgasm!
Even if sex isn’t painful, you may be asking yourself, “Why can’t I orgasm anymore?”
Vaginal atrophy usually won’t prevent you from having an orgasm from penetrative sex, but it can create hurdles to doing so if left untreated.
Remember, vaginal atrophy can cause a loss of vaginal elasticity. So, penetration can be tricky and painful. And vaginal dryness can irritate delicate tissues.
The friction of intercourse, use of a vibrator, or other form of penetration can make for a situation that is agonizing instead of pleasurable because of the lack of lubrication.
Additionally, during the menopause transition, especially in the post-menopausal stage, there is also reduced blood flow to your clitoris and lower vagina. This can reduce sensitivity and make it harder to orgasm in both situations involving a partner as well as other forms of sexual stimulation.
So, what’s the answer? Some women+ have less sex, which can make matters worse. And if they are in a relationship with a partner, a change in sexual intimacy may add stress and strain that can impact libido.
To add insult to injury, the less penetrative sex you have, the more difficult it can become to orgasm from sexual intercourse. When you don’t have regular penetrative sex, your vagina can become narrow and shorter.
And even with a lubricant, sex may still be painful. Which in turn means you avoid penetration, and it becomes a vicious cycle. As the saying goes, “Use it or lose it!”
It may sound counterproductive, but regular sexual activity during the menopause journey can help to keep your vagina longer and wider, help maintain blood flow, and increase natural lubrication.
So, to protect your orgasms for those who are able, engaging in safe sexual activity regularly is one more way to improve the symptoms of GSM.
Please remember GSM symptoms are not something you have to endure. Treatment options (hormonal and non-hormonal) are available so sex can be pleasurable again.
Treatment options
YES! There are many treatment options.
The most important takeaway? Do not suffer in silence!
Like many of the symptoms women experience during the menopause journey, your doctor may not ask if you are having this problem, and some women+ find it awkward and uncomfortable to discuss GSM.
However, vaginal atrophy is a progressive condition, so the longer you wait, the worse things can get and the longer you suffer unnecessarily.
So, what can be done?
Many women+ ask if vaginal atrophy can be reversed, but the thing to remember is that the primary goal of treatment is to relieve your symptoms, whether those are in your vagina, vulva, pelvis, urinary tract or you experience them during sex.
OTC lubricants and moisturizers for a dry vagina
If your symptoms are mild to moderate, there are a wide range of non-hormonal over-the-counter vaginal lubricants (reduce friction; used in the moment when engaging in sexual activity), which are a good place to start.
Just like you apply moisturizer to your body, if you have dry, itchy skin during the hormonal transition, you’ll also want to apply a vaginal moisturizer to your vagina. Your healthcare provider may recommend a long-acting vaginal moisturizer to hydrate cells and tissue. It is meant to be used consistently (like your face) up to 7 days a week.
When applied regularly, over-the-counter (OTC) products can help to alleviate the issues created by vaginal dryness, both as you go through your day and at the time of sexual activity.
As always, pay attention to labels and follow all instructions. Although you can use these products externally, these options are meant to be used inside the vagina to achieve their results. So, make sure you don’t find yourself picking up something labeled as a moisturizer but intended for external use only.
When it comes to lubricants, water-based are usually a better option, although silicone-based also works. However, silicone may cause sex toys made of silicone to break down.
Products such as petroleum jelly and mineral oil are NOT suitable and may worsen your symptoms or increase the risk of infection.
And if you are in the perimenopause stage of the journey, remember you can still get pregnant. Petroleum jelly and oils can also cause latex condoms to break. That means the effectiveness of condoms in preventing pregnancy and sexually transmitted infections (STIs) would be reduced.
Prescription medication for GSM
In addition to over-the-counter moisturizers and lubricants, there are several medications to treat GSM. Like treating other symptoms during the hormonal transition, some products have hormones and others are non-hormonal.
Some women+ have concerns and even fears regarding hormone therapy. There are indeed risks in its use that some women+ may not want to take. Others should not use HT, or certain HT formulations, due to prior or underlying medical conditions like breast and uterine cancer or blood clots.
It’s your body and you can choose a hormone-free product or one with hormones, depending on your personal situation. Connect with your healthcare practitioner to get guidance based on your particular health status.
Researchers are also testing other medications like vaginal tamoxifen capsules. The capsule DARE-VVA1 does not have hormones and helped post-menopausal women+ with thinning and dryness in a clinical study. Adverse side effects were mild to moderate.
Ospemifene (OSPHENA®)
Ospemifene is an oral, non-hormonal treatment approved by the FDA for moderate-to-severe vaginal dryness and/or moderate-to-severe painful intercourse. It also addresses symptoms due to changes in and around your vagina related to the menopause journey. It reduces the pH of the vagina and also changes the number of certain types of vaginal cells.
Ospemifene should not be used by everyone, e.g., those with unusual vaginal bleeding, a history of stroke, heart attack, blood clots, severe liver disease, and certain cancers. It can also increase the risk of uterine cancer. Potential side effects include stroke, blood clots, vasomotor symptoms like hot flashes and night sweats, headache, and heavy vaginal bleeding.
Prasterone DHEA vaginal inserts (INTRAROSA®)
INTRAROSA® is FDA-approved vaginal insert for use in post-menopausal women. It can treat painful sexual intercourse due to vaginal changes caused by menopause.
The insert is made of prasterone, a man-made form of DHEA.
Dehydroepiandrosterone (DHEA) is a hormone made in the adrenal glands. Those are located on top of each kidney and make hormones that help control functions like heart rate and blood pressure.
While it is advertised as a non-estrogen, it is converted to sex hormones such as estrogen, progestin, and testosterone in the body. DHEA is used by the body to produce those other hormones and, as such, is considered what is known as a precursor.
The inserts should not be used if you have abnormal vaginal bleeding, which needs to be investigated, and certain types of cancer. Potential side effects include abnormal Pap smear results and vaginal discharge.
Hormone therapy: pills, estrogen cream, and vaginal rings
There are a variety of formulations and ways to take hormones (e.g., creams, rings, tablets), and understanding the array of hormone therapy medication options can be challenging.
For example, some women may take hormones orally because they have several menopausal symptoms, for which systemic HT is a good option, like hot flashes and night sweats.
However, if your main menopause symptom is vaginal dryness, then estrogen cream used locally may be all you need, rather than a pill which results in the distribution in the bloodstream throughout the body.
Estrogen cream can help to relieve vaginal dryness as well as itching, inflammation, or soreness of the vulva. For some women+, it may be the best solution, especially if GSM symptoms are severe.
Low-dose estradiol or estriol vaginal rings have also been found to be effective for persistent GSM symptoms.
A new (2023) phase 2 study also found 15 mg of estetrol (E4) helps with hot flashes and GSM. It decreased signs of vaginal atrophy. The women+ reported a 41% reduction in vaginal dryness and 50% reduction in pain.
Vaginal stretching exercises and dilators
In addition to medication and over-the-counter moisturizers, anecdotally, some women have reported benefiting from gentle and regular vaginal stretching exercises, although there are no clinical trials to support this.
The muscles around your vagina, like any muscle in your body, can get tight or stiff. Gentle stretching may help alleviate muscle tension and discomfort.
A good option for women+ with severe GSM may be a vaginal dilator for those who engage in penetrative sex. It can be especially helpful if intercourse is not possible because your vagina has become too short or narrow.
Vaginal dilators can stretch and enlarge your vagina slowly as part of sexual activity alone or with a partner.
If you are considering vaginal exercises or dilators, please consult with your GYN, who may refer you to a pelvic floor physical therapist to offer specific guidance tailored to your needs.
Kegel exercises to strengthen your pelvis
These are not just for a postpartum body! They’re important during the menopause journey too.
Kegel exercises were developed in the 1940s by the gynecologist, Dr. Arnold H. Kegel.
They are a nonsurgical technique you perform that strengthens pelvic floor muscles and reduces the likelihood of leakage of urine.
On the other hand, “reverse Kegel” exercises can help release pelvic pain and tightness. It is important to learn how to tighten and release your pelvic floor.
A hypertonic pelvic floor (overactive) can cause as many disorders as a relaxed one but is often harder to diagnose.
Your healthcare provider can help you find a pelvic floor physical therapist to help you strengthen your pelvis as well as teach you additional pelvic floor exercises.
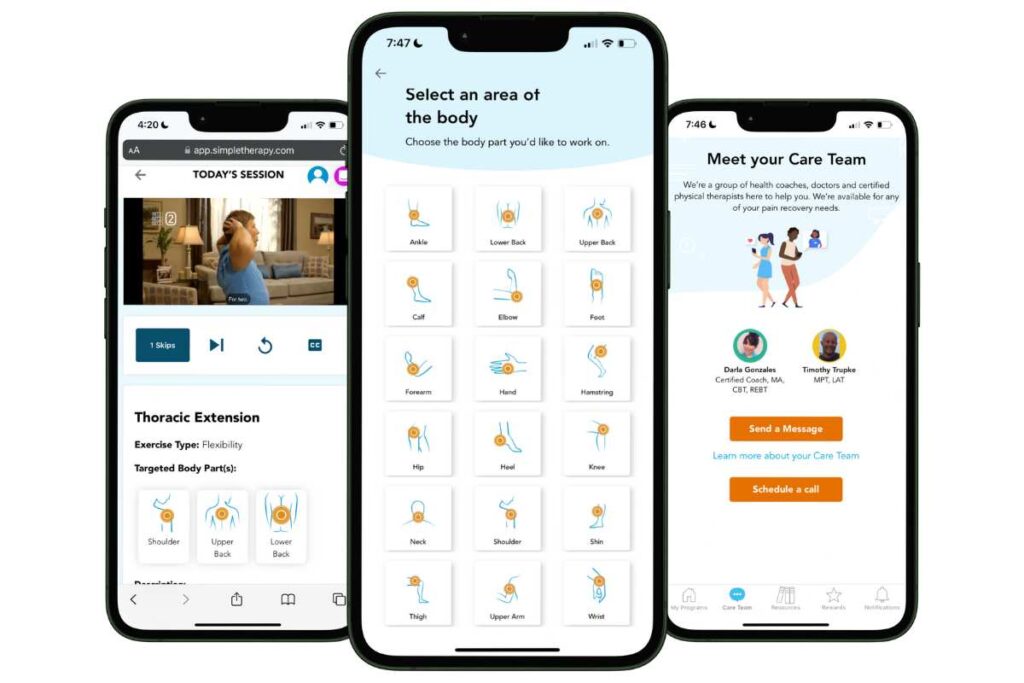
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!

Speak up
Don’t be embarrassed by vaginal, urinary, or sexual symptoms. Or any of the other symptoms you may experience. GSM is just one of them.
Dr. Z. Colette Edwards, Founder and Chief Medical Officer of pausitive health, spoke with Peli Health about pelvic wellness during the menopause journey and the emotional layers of it. This is a journey, and you can make this a stage of life that’s empowering.
While you have options to address symptoms like GSM, they may not work for everyone. The MsFLASH Vaginal Heath Trial, which sought to seek “lasting answers for symptoms,” found that contrary to treatment guidelines, estradiol tablets and OTC vaginal moisturizers did not provide additional benefits over placebo treatments.
In a post-hoc analysis of that trial, researchers concluded that instead of focusing on a single symptom, it might be more important to focus on how the symptoms impact a woman’s daily life and well-being.
At pausitive health, we couldn’t agree more! So many menopausal symptoms are interconnected, and everyone’s journey is unique. One treatment may work for you and not for another person.
So, you should consider a healthcare practitioner who can help you take a holistic approach to your health and well-being or use a doctor certified by The Menopause Society for their menopause training and credentials. Find a Menopause Society Certified Practitioner (MSCP) near you.
You can also make an appointment with a specialist. The International Society for Women’s Sexual Health (ISSWSH) has a provider directory that you can search. These are ISSWSH members whose work is at least partially focused on women’s sexual health.
Consult with your healthcare provider so s/he can provide guidance about the pros and cons, recommend products, and help you determine the best option for you.
You have treatment choices that include both hormonal and non-hormonal options.
Investing in the time for that conversation will give you control and the confidence you are making the best decision for you.
And it’s always a good idea to prepare for your medical appointments in advance.
Keep a list of your symptoms and how often you experience them. This information will help your healthcare provider gain a deeper understanding of what you are experiencing and find a solution that is a good fit for your situation.
Questions to Ask Your Doctor
• Do I need any tests to confirm your diagnosis?
• What do you think has caused this in my case?
• Is there anything I can do to prevent my condition from deteriorating further?
• Which treatment do you recommend for my circumstances?
• How long will it take for treatment to start working?
• If this treatment doesn’t work, how long do we need to wait before trying other options?
• Can you recommend any trusted websites where I can learn more about my condition?
• When should I try to have sexual intercourse again?
This stage of your life can be a time of renewal, transformation, and freedom.
Don’t suffer in silence! Take the time now to make a change for the better.
Sheryl A. Kingsberg, Michael Krychman, Shelli Graham, Brian Bernick, Sebastian Mirkin, The Women’s EMPOWER Survey: Identifying Women’s Perceptions on Vulvar and Vaginal Atrophy and Its Treatment, The Journal of Sexual Medicine, Volume 14, Issue 3, 2017, Pages 413-424, ISSN 1743-6095, https://doi.org/10.1016/j.jsxm.2017.01.010.
Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020 Apr 8;12(4):e7586. doi: 10.7759/cureus.7586. PMID: 32399320; PMCID: PMC7212735.
Elagolix – The First FDA-Approved Treatment for Endometriosis and Uterine Fibroids | Eunice Kennedy Shriver National Institute of Child Health and Human Development
Decreased Response and Pleasure | The Menopause Society
Gaspard U, Taziaux M, Jost M, Coelingh Bennink HJT, Utian WH, Lobo RA, Foidart JM. A multicenter, randomized, placebo-controlled study to select the minimum effective dose of estetrol in postmenopausal participants (E4Relief): part 2-vaginal cytology, genitourinary syndrome of menopause, and health-related quality of life. Menopause. 2023 May 1;30(5):480-489. doi: 10.1097/GME.0000000000002167. Epub 2023 Feb 20. PMID: 36809193; PMCID: PMC10155698.
Sarmento ACA, Costa APF, Vieira-Baptista P, Giraldo PC, Eleutério J Jr, Gonçalves AK. Genitourinary Syndrome of Menopause: Epidemiology, Physiopathology, Clinical Manifestation and Diagnostic. Front Reprod Health. 2021 Nov 15;3:779398. doi: 10.3389/frph.2021.779398. PMID: 36304000; PMCID: PMC9580828.
Every Woman Can Benefit From This Pelvic Floor Workout | The New York Times
Kegel exercises – self-care | MedlinePlus
Angelou K, Grigoriadis T, Diakosavvas M, Zacharakis D, Athanasiou S. The Genitourinary Syndrome of Menopause: An Overview of the Recent Data. Cureus. 2020 Apr 8;12(4):e7586. doi: 10.7759/cureus.7586. PMID: 32399320; PMCID: PMC7212735.
Vaginal tamoxifen capsule safe in women with postmenopausal thinning, dryness | Healio
OSPHENA® Highlights of Prescribing Information | Food and Drug Administration

Is Your Pelvic Floor in Perimenopause Too?
Give your pelvic health some love in perimenopause. It’s more than Kegels. Get solutions to improve vaginal and sexual health, your bladder, and pelvic floor.

Pelvic Floor Rehab: 10 Treatment Options During the Menopause Journey
Pelvic floor symptoms can be embarrasing, but don’t have to be. Learn about pelvic floor rehab options. Get treatment that’s right for you.

Menopause Matters: Understanding Pelvic Floor (Bladder and Bowel) Symptoms
Your pelvic floor is the “forgotten core” but your body may remind you of this area during the menopause journey, with bladder and bowel symptoms.

