Osteoporosis is a “silent” condition, with few symptoms. In fact, sometimes women+ don’t realize they have osteoporosis until they break a bone! Don’t wait for a fall to discover the importance of bone health, because it’s not curable. You can help prevent it. You can also manage its progression if you already have osteoporosis or osteopenia (the stage before osteoporosis). If you’re diagnosed, take the time to learn your treatment options.
What is osteoporosis?
Osteoporosis means “porous bones.” It is a bone disease that develops when:
- the structure and strength of your bone change and/or
- bone mineral density and bone mass decrease
Half of post-menopausal women+ will have osteoporosis.
As you age, your body loses more bone mass than it creates. And for those on the menopause journey, the drop in estrogen levels can also contribute to bone loss.
Osteoporosis weakens your bones and increases your risk of breaking a bone even after a minor fall or bump. Every 3 seconds, someone breaks a bone worldwide because of osteoporosis.
80% of patients are undiagnosed and untreated even after a fracture. That’s why it’s important to get screened and understand risk factors.
Osteoporosis is one of several musculoskeletal conditions women+ may experience on the menopause journey. In 2024, the muscle aches and pains and bone loss and thinning associated with the drop in estrogen became known as the musculoskeletal syndrome of menopause (MSM).
Signs of osteoporosis
Osteoporosis commonly shows up as:
- Loss of height (just over an inch).
- Curved or stooped upper back.
- You may also experience back pain.
- Bone fracture (hip, wrist, spine).
Risk factors
Osteoporosis can be a concern at any stage of the menopause journey, but it’s common in post-menopause, with 50% of women+ having it at that point of the menopausal transition.
Risk factors include:
- Family history
- Gender (80% of those with osteoporosis are women.)
- Menopause (up to 20% bone loss during this time)
- Specific menopause symptoms like hot flashes
- Hysterectomy
- Early menopause
- Age
- Previous break due to a minor fall
- Medications (such as certain antidepressants, steroid hormones, diabetes, thyroid, proton pump inhibitors, certain types of chemotherapy)
- Other diseases (such as rheumatoid arthritis, GI conditions like celiac disease, COPD, asthma, endocrine disorders, immobility, certain cancers like multiple myeloma, and dementia)
- Cancer that spreads to the bone
- Excessive alcohol (drinking two or more glasses of alcohol a day increases the risk of fracture)
- Smoking
- Low body mass index (below 19 is a significant risk factor)
- Poor nutrition, malnutrition, and eating disorders
- Low calcium intake (e.g., those who avoid dairy products due to lactose intolerance or milk sensitivity, vegans)
- Vitamin D deficiency
- Physical inactivity
- Frequent falls
- Race
Health inequities
Osteoporosis is more likely to occur in white and Asian women, with the highest fracture rates in white women.
| Race | Have Osteoporosis |
|---|---|
| Asian | 20% |
| White | 20% |
| Native American | 12% |
| Hispanic/Latina | 10% |
| Black | 5% |
While Black women are less likely to break a bone because their bone mineral density tends to be higher, when it does happen, recovery is more complicated.
Black women:
- stay in the hospital longer.
- are less likely to be able to walk at discharge.
- are more likely to die after breaking a hip.
This Bone Health & Osteoporosis Foundation infographic includes practical tips and action about osteoporosis in the Black community.

Talk to your doctor about the risks
In women over age 45, fractures due to osteoporosis lead to more days in the hospital than diseases like diabetes, heart attack, and breast cancer. Screening is critical to avoid costly medical bills, debilitating injuries, and potentially life-threatening complications.
The International Osteoporosis Foundation has an interactive risk check that raises awareness of risk factors that you can change to lower the chance of developing osteoporosis and experiencing a fracture.
It is not a diagnostic tool, but it can give you an understanding of the issue and your risk factors.
Talk to your doctor about risk factors and when you should have an osteoporosis screening based on your particular situation.
Should I be screened for osteoporosis?
Screening is recommended for women:
- Age 65 years or older, regardless of risk factors
- Age 50 to 64 who have certain risk factors like a family history or a broken hip
- With a broken bone after age 50
If you fall into these categories, talk to your doctor about osteoporosis during an annual wellness visit and preventive care exam.
Remember, osteoporosis is treatable, and there are steps you can take to help prevent it.
How do doctors screen for osteoporosis?
There are two common ways to screen and diagnose osteoporosis:
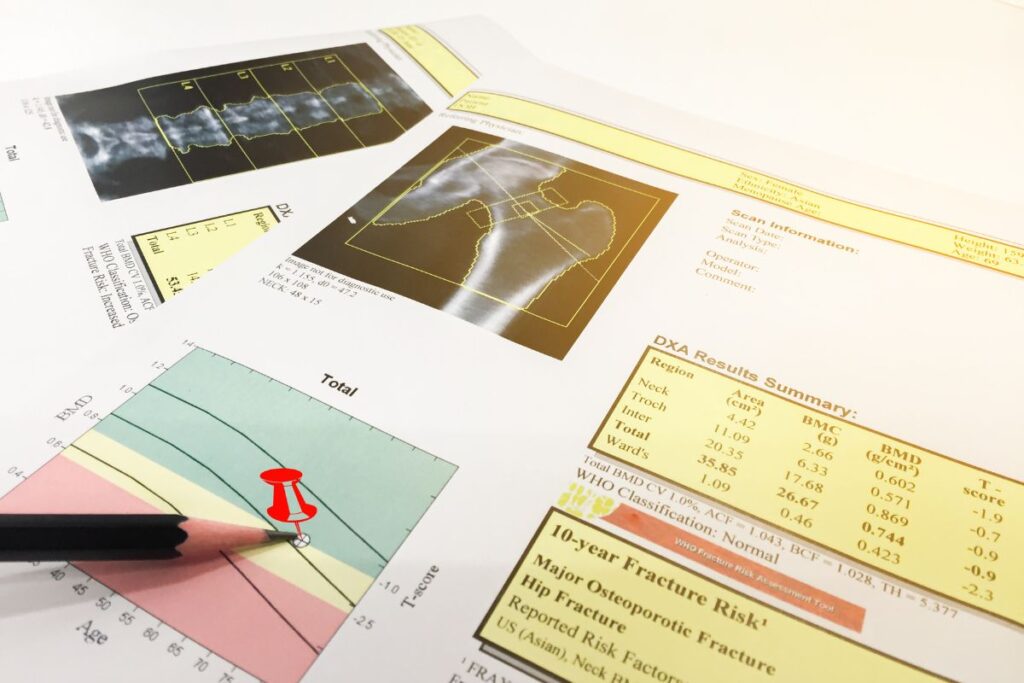
Bone Mineral Density (BMD) Test
BMD is a simple and painless test, using a low-level X-ray known as DEXA – dual-energy X-ray absorptiometry – or DXA for bone densitometry test. You lie on a table and follow the technician’s instructions as the arm of the DXA machine moves over your body.
It helps determine if you have osteoporosis or are at risk of developing it. Your doctor may also use this test during and after treatment to determine your body’s response.
You’ll get a T-score in a range that shows a normal bone density, osteopenia (in-between stage), or osteoporosis.
BMD is generally recommended in the U.S. for women+ age 65 and older, regardless of risk factors. However, your healthcare practitioner may amend the timing and frequency of testing depending on your risk factors, medical history, and if you have had a fracture after age 50, among other considerations that may be considered.
Fracture Risk Assessment Tool
The FRAX Risk Assessment Tool determines an individual’s 10-year fracture risk by considering their age, sex, weight, height, previous fracture, and family history.
It also factors in smoking, osteoporosis-related disorders, alcohol use, and bone mineral density (BMD) scores, if available.
You don’t need a BMD test to complete the FRAX assessment.
While the assessment tool is helpful, the Bone Mineral Density (BMD) test is typically used to diagnose osteoporosis.
Your doctor may also order other tests to diagnose osteoporosis, e.g., CT scan, especially if there’s an area of the body of particular concern.
T-Scores: What do they mean?
When you have a bone mineral density test, you’ll receive a T-score. So, what does it mean?
| Status | T-Score |
|---|---|
| -1 and above | Normal |
| -1 and -2.5 | Osteopenia |
| -2.5 and lower | Osteoporosis |
|
-2.5 and lower and the presence of one fragility fracture (a fracture resulting from a fall from standing height or less) |
Severe Osteoporosis |
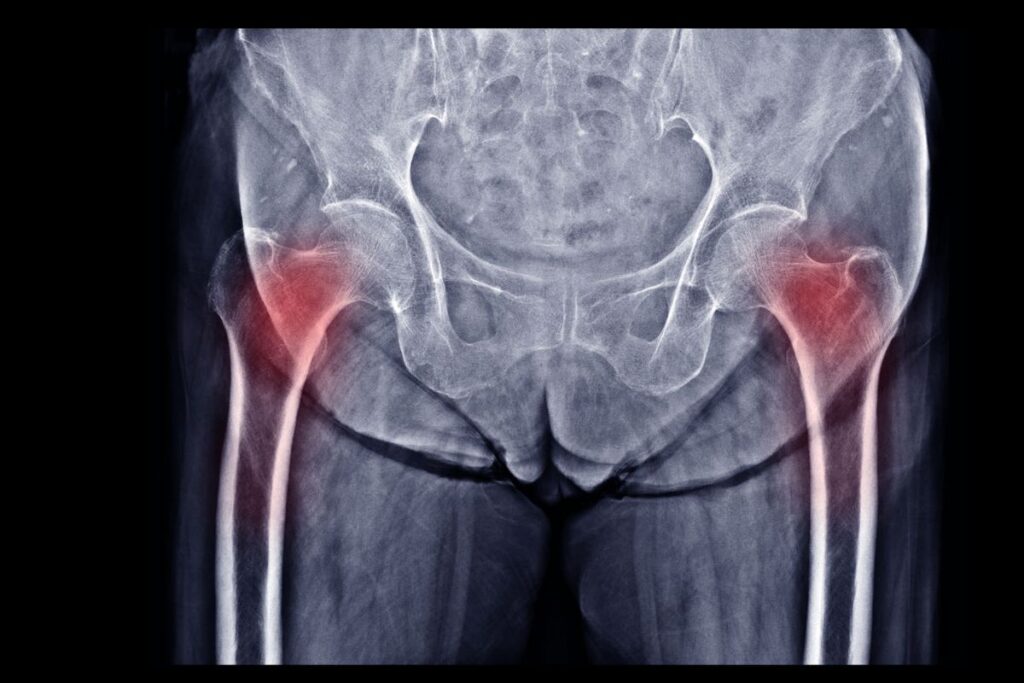
Hip and spine fractures could be a sign of osteoporosis
While the T-score is used to diagnose osteoporosis, regardless of that score, you likely have osteoporosis if you’ve had a hip or spine fracture.
If you’re over 50 and have a broken rib, pelvis, wrist, or shoulder, you may also have it, according to the Bone Health & Osteoporosis Foundation.
75% of hip fractures happen in women, which is concerning because it can lead to death in the first year of your recovery.
But it’s not the only concern. According to the American Academy of Orthopaedic Surgeons, spine fractures occur nearly twice as often as other osteoporosis-related breaks, like broken hips and wrists.
How is osteoporosis treated?
There are several medications to treat osteoporosis. They can help reduce bone loss or stimulate growth. Treatment can reduce the risk of a hip fracture by up to 40% but will not cure osteoporosis. That’s why prevention is critical.
Talk to your doctor about the potential risks and benefits.
The Bone Health & Osteoporosis Foundation lists some of the common medications for the treatment of osteoporosis:
- Bisphosphonates (alendronate, risedronate, ibandronate, zoledronic acid)
- Selective estrogen receptor modulators (SERMS) – Raloxifene
- Tissue-Specific Estrogen Complex – bazedoxifene
- Parathyroid Hormone (PTH) – Teriparatide
- Parathyroid Hormone-Related Protein (PTHrp) – abaloparatide
- Sclerostin Inhibitor – Romosozumab
- Calcitonin
- Monoclonal antibody targeting RANK ligand (RANKL) – Denosumab
If/which medication is the best option for you, it will depend on factors such as the area of the body of most concern and the type of risks you may have for osteoporosis.
Hormone therapy and bone loss
Hormone therapy can also help with bone loss and is FDA-approved as a preventive option. However, it’s important to discuss the benefits and risks with your doctor based on your particular situation, as there remains controversy in the medical community regarding its use for the primary prevention of osteoporosis.

How can I reduce the risk with food?
At pausitive health, we often talk about the impact of a healthy lifestyle on symptoms during the menopause journey. It can also help prevent or mitigate the impact and complications of osteoporosis.
Food can be a powerful medicine. And it’s seldom too late to start a healthy lifestyle.
First, eat foods that can help improve your menopause journey.
At a bare minimum, focus on foods rich in:
- Calcium – milk, yogurt, meat, fish, eggs, cheese – feta, mozzarella, cottage, ricotta, cheddar, parmesan; and if you are vegan, beans/lentils, nuts/seeds, and vegetables
- Lean protein – most types of fish, Greek yogurt, nuts, Brussel sprouts, broccoli, collards/mustard greens, cauliflower, lima beans, spinach, beans,
- Vitamin D – salmon, egg yolk, shitake mushrooms, tuna, sardines; very few food foods have enough vitamin D, which is why you see foods fortified with vitamin D; you’ll likely need a supplement and/or spend sufficient time in the sunshine
If you’re a woman+ of color, talk to your doctor about your Vitamin D levels. Lactose intolerance is common, sometimes making it more difficult to get enough vitamin D, which is critical for preventing osteoporosis.
| Race | Have Lactose Intolerance |
|---|---|
| Asian | 90% |
| White | 25% |
| Native American | ~100% |
| Hispanic/Latina | 50-80% |
| Black | 70% |
Source: Lactose intolerance [The BMJ]
While those are the three primary nutrients, you should also eat:
- Vitamin B12 – meat, fish, dairy, fortified breakfast cereal
- Vitamin K2 – green leafy vegetables like spinach, kale, broccoli, and Brussels sprouts
- Zinc – meat, shellfish, nuts, legumes, sweet potato, white potato with skin
- Magnesium – pumpkin and chia seeds, almonds, cashews, and peanuts, spinach, soy milk, edamame, black beans; Magnesium can also help with restless leg syndrome.
- Probiotics – there’s a gut connection with bone health. A healthy gut can help your body absorb vitamin D and calcium. Preliminary studies in humans, and laboratory research suggests probiotics can help prevent bone loss. Despite the initial evidence, The Menopause Society highlights probiotics in its 2021 position statement.
Osteoporosis foods
Research shows certain foods can positively impact bone health and improve bone mineral density, thus lowering fracture risk. These foods include a diet packed with:
- fruits
- vegetables
- low-fat dairy
- whole grains
- poultry
- fish
- nuts
- legumes
Fruits and vegetables are packed with nutrients like vitamin K, folate, magnesium, potassium, and antioxidants like vitamin C. Diets packed with fruits and vegetables can lead to higher bone mineral density over time.
A Swedish study found that eating less than five servings daily led to a higher risk of hip fracture in men and women.
Want a list of fruits, vegetables, and other foods rich in calcium, protein, and vitamin D? Download the pausitive health grocery list.
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
"*" indicates required fields
Once you have the right foods in your kitchen, you can find recipes from the Bone Health & Osteoporosis Foundation. These include ricotta pancakes, hummus, stuffed mushrooms, and a mango smoothie.
Diets around the world and the impact on bone health
In Asian populations, diets rich in fruits, vegetables, and soy helped lower risks of fracture and osteoporosis.
Fish is also popular in the Asian diet, and it’s thought that soy and fish significantly contribute to lower incidences of osteoporosis fractures in Asian women+. And a potential higher intake of soy is believed to be a potential reason for the report of fewer/less severe menopause symptoms like hot flashes in the general Asian women+ population.
Korean women who eat a lot of fruits and dairy products have been found to decrease the risk of osteoporosis compared with those who consume a diet of meat, alcohol, and sugar.
Postmenopausal Spanish women saw positive benefits from eating the Mediterranean diet. Olive oil is at the heart of the Mediterranean diet, and the olive oil’s phenols can help prevent the loss of bone mass.
In contrast, women typically have lower bone mineral density when they follow a Western diet, which often consists of processed proteins, including processed meat, and foods high in fat, sugar, salt, and refined grains like pizza, French fries, snacks, and pastries.
The U.S. Department of Agriculture developed My Plate, to help you eat the right amount of food from each food group. Your meal should contain, fruits, vegetables, grains, protein, and dairy. You can find recipes based on food groups, and you can also search for nutrients on MyPlate.
Herbs and supplements that may help with osteoporosis
Many women turn to herbs as an alternative option to treat menopausal symptoms. They can also help prevent osteoporosis, although studies are typically more limited and more research is needed.
Some of these herbs belong to foods that can help with osteoporosis, like legumes, or contain phytoestrogens.
There are also studies showing the benefits of these botanicals:
- Red clover – legume with isoflavones
- Soybeans – contain isoflavones
- Hops – contain phytoestrogens
- Labisia pumila – phytoestrogen used in Asia
- Alfalfa – legume contains phytoestrogens
- Red sage – been used in traditional Chinese medicine
- Dried rhizome – helps with age-associated bone loss
- Black cohosh – helps bone mineral density
- Dried plums – vitamins like potassium and vitamin K and polyphenols
- Epimedium – used in traditional Chinese medicine to treat bone fractures, bone loss, and menopause-related disorders
Always talk to your doctor before taking an herb or supplement, as they can interact with other medications or be problematic if you have certain underlying conditions.
Other lifestyle factors
In addition to food as medicine, focus on other lifestyle factors, including:
Exercise
Focus on resistance training, muscle strengthening, and weight-bearing exercises. Balance and posture are just as important. Try these exercises designed for menopausal women, including chair exercises.
You can work with a trainer or use a BoneFitTM professional with the training to work with individuals with low bone density. Find a BoneFit professional near you.
Manage other menopausal symptoms like hot flashes, which are known to increase osteoporosis.
Interestingly, some studies have shown menopause symptoms like hot flashes are associated with lower bone mineral density.
Another study found hot flashes nearly double the risk of hip fracture.
So, managing these symptoms with HT or non-hormonal options is important.
Maintain a healthy body weight.
Your risk increases if you’re underweight [have a body mass index (BMI) less than 19].
If you’re trying to lose weight during menopause, you need to pay attention to the foods you eat so you’re not eliminating foods important to bone health.
Being obese is a mixed picture when it comes to osteoporosis. Although you’re more likely to have a higher bone mineral density, you’re also more likely to have a fracture. And, of course, your goal would be to achieve a healthy weight, as obesity is hard on your joints and increases the risk of conditions like heart disease, diabetes, hypertension, and metabolic syndrome.
Stop smoking
Smoking is a risk factor for osteoporosis (not to mention lung cancer as well as reaching menopause up to 2 years earlier than non-smokers or experiencing early menopause) and fractures and is part of the Fracture Risk Assessment Tool. The tobacco in cigarettes can impact the skeletal system by causing an imbalance in bone turnover, leading to lower bone mass and bone density.
Avoid heavy drinking
New research shows any amount of alcohol can negatively impact your health. In this case, heavy drinking and long-term alcohol use can affect bone growth, decreasing bone density.
Don’t underestimate this silent disease
Since osteoporosis is a silent disease, it’s easy to underestimate the impact of it. But think about it for a second. Nearly a quarter (20-24%) of patients who fracture their hip, die in the first year of recovery.
Breaking your hip also impacts you physically, mentally, and emotionally. A year after the break, 60% of patients still need help.
Don’t let a fall be your wake-up call.
Plus, osteoporosis may be just one of a number of musculoskeletal issues you experience during the journey. New research shows women may also suffer from frozen shoulder, tendon, and ligament injuries and joint pain. This group of conditions is now known as the musculoskeletal syndrome of menopause.
Many of the same proactive measures for osteoporosis prevention can also help with overall aches and pains. In our pausitive health membership program, we offer personalized physical therapist-led exercises to keep you moving and help with any joint or muscle pain.
Take action today and make a change for the better!
Free Support
For Your Menopause Journey!
Only available for a limited time!
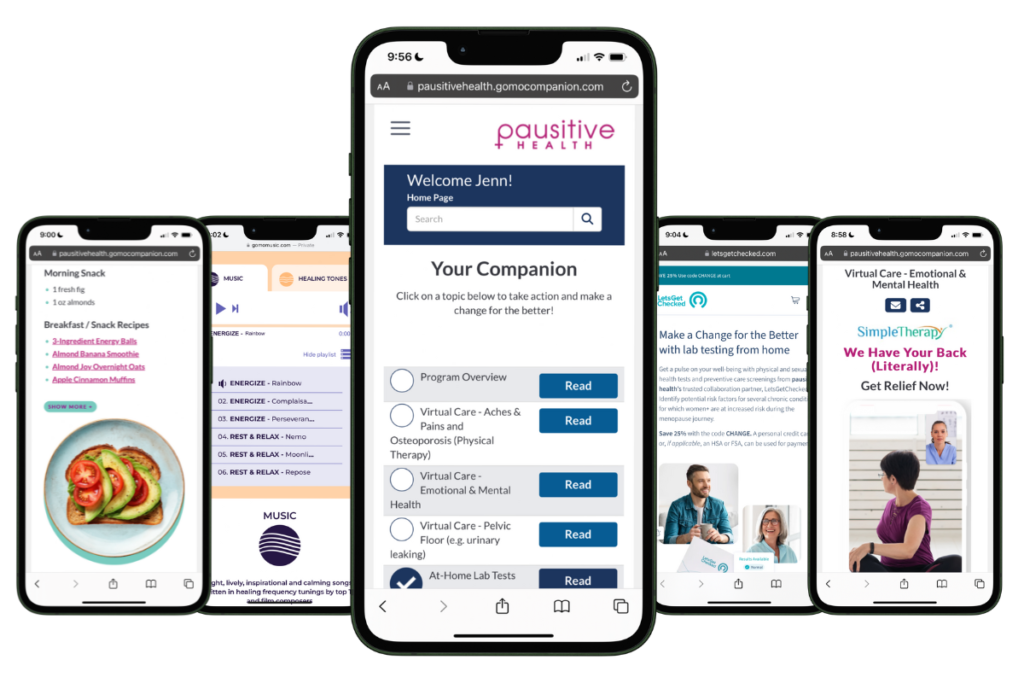
Access a one-stop menopause journey digital destination that provides personalized text messages that focus on educational topics you select and offers many other features such as a diet assessment with recommendations, solutions from collaboration partners to address menopausal aches and pains (the musculoskeletal syndrome of menopause – MSM), pelvic floor issues, virtual care, lifestyle tools, and a supportive community.
What Women Need to Know | Bone Health & Osteoporosis Foundation
Epidemiology of Osteoporosis and Fragility Fractures | International Osteoporosis Foundation
About Osteoporosis | International Osteoporosis Foundation
Shoback D, Rosen C, Black D, Cheung A, Murad M H, Eastell R. Pharmacological Management of Osteoporosis in Postmenopausal Women: An Endocrine Society Guideline Update. The Journal of Clinical Endocrinology & Metabolism, Volume 105, Issue 3, March 2020, Pages 587–594. https://doi.org/10.1210/clinem/dgaa048
Risk Factors | International Osteoporosis Foundation
Bone Health and Postmenopausal Women | Endocrine Society
Keen MU, Reddivari AKR. Osteoporosis in Females. [Updated 2023 Jun 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing.
Cauley JA. Defining ethnic and racial differences in osteoporosis and fragility fractures. Clin Orthop Relat Res. 2011 Jul;469(7):1891-9. doi: 10.1007/s11999-011-1863-5. PMID: 21431462; PMCID: PMC3111798.
Osteoporosis Risk Check | International Osteoporosis Foundation
FRAX® – Fracture Risk Assessment Tool | Centre for Metabolic Bone Diseases
Evaluation of Bone Health/Bone Density Testing | Bone Health & Osteoporosis Foundation
Osteoporosis and Spinal Fractures | OrthoInfo
Medicines for Prevention and Treatment | Bone Health & Osteoporosis Foundation
The North American Menopause Society. The 2022 hormone therapy position statement of The North American Menopause Society (now The Menopause Society). Menopause: The Journal of The North American Menopause Society. 2022. Vol. 29, No. 7, pp. 767-794. DOI: 10.1097/GME.0000000000002028
Sun Protect and Vitamin D | Skin Cancer Foundation
Bhatnagar S, Aggarwal R. Lactose intolerance. BMJ. 2007 Jun 30;334(7608):1331-2. doi: 10.1136/bmj.39252.524375.80. PMID: 17599979; PMCID: PMC1906652.
Vitamins for Bone Health | American Bone Health™
Muñoz-Garach A, García-Fontana B, Muñoz-Torres M. Nutrients and Dietary Patterns Related to Osteoporosis. Nutrients. 2020 Jul 3;12(7):1986. doi: 10.3390/nu12071986. PMID: 32635394; PMCID: PMC7400143.
Sahni S, Mangano KM, McLean RR, Hannan MT, Kiel DP. Dietary Approaches for Bone Health: Lessons from the Framingham Osteoporosis Study. Curr Osteoporos Rep. 2015 Aug;13(4):245-55. doi: 10.1007/s11914-015-0272-1. PMID: 26045228; PMCID: PMC4928581.
Byberg L, Bellavia A, Orsini N, Wolk A, Michaëlsson K. Fruit and vegetable intake and risk of hip fracture: a cohort study of Swedish men and women. J Bone Miner Res. 2015 Jun;30(6):976-84. doi: 10.1002/jbmr.2384. PMID: 25294687.
Shin S, Joung H. A dairy and fruit dietary pattern is associated with a reduced likelihood of osteoporosis in Korean postmenopausal women. Br J Nutr. 2013 Nov;110(10):1926-33. doi: 10.1017/S0007114513001219. Epub 2013 Apr 12. PMID: 23578480.
García-Martínez O, Rivas A, Ramos-Torrecillas J, De Luna-Bertos E, Ruiz C. The effect of olive oil on osteoporosis prevention. Int J Food Sci Nutr. 2014 Nov;65(7):834-40. doi: 10.3109/09637486.2014.931361. Epub 2014 Jun 30. PMID: 24975408.
Sahni S, Mangano KM, McLean RR, Hannan MT, Kiel DP. Dietary Approaches for Bone Health: Lessons from the Framingham Osteoporosis Study. Curr Osteoporos Rep. 2015 Aug;13(4):245-55. doi: 10.1007/s11914-015-0272-1. PMID: 26045228; PMCID: PMC4928581.
MyPlate | U.S. Department of Agriculture
Słupski W, Jawień P, Nowak B. Botanicals in Postmenopausal Osteoporosis. Nutrients. 2021 May 11;13(5):1609. doi: 10.3390/nu13051609. PMID: 34064936; PMCID: PMC8151026.
BONEFIT – Find a Professional | Bone Health & Osteoporosis Foundation
Gast GC, Grobbee DE, Pop VJ, Keyzer JJ, Wijnands-van Gent CJ, Samsioe GN, Nilsson PM, van der Schouw YT. Vasomotor symptoms are associated with a lower bone mineral density. Menopause. 2009 Mar-Apr;16(2):231-8. doi: 10.1097/gme.0b013e318185e25b. PMID: 19034053.
Study finds strong association between hot flashes, bone health | University at Buffalo
Sampson HW. Alcohol’s harmful effects on bone. Alcohol Health Res World. 1998;22(3):190-4. PMID: 15706795; PMCID: PMC6761900.
Al-Bashaireh AM, Haddad LG, Weaver M, Chengguo X, Kelly DL, Yoon S. The Effect of Tobacco Smoking on Bone Mass: An Overview of Pathophysiologic Mechanisms. J Osteoporos. 2018 Dec 2;2018:1206235. doi: 10.1155/2018/1206235. PMID: 30631414; PMCID: PMC6304634.
No level of alcohol consumption is safe for our health | World Health Organization
IOF urges action for prevention as study predicts global hip fractures to almost double by 2050 | International Osteoporosis Foundation
You may also like…

What You Need to Know About the Musculoskeletal Syndrome of Menopause
Feeling new joint pain even though you don’t have an injury? Musculoskeletal syndrome of menoapuse can cause aches and pains. Get treatment.

Don’t Let Osteoporosis Knock You Down: Medications That Can Help
If you’ve been diagnosed with osteoporosis, medication can help. Learn about the pros and cons of osteoporosis medications.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.