At the beginning of your menopause journey, you may have thought hot flashes were the worst symptom you’d have to deal with. But perhaps now you’re having difficulty concentrating, and your thinking may be slowed. If you once had a sharp mind and are starting to worry: “Why am I so forgetful?” you’re like a lot of women+ on the menopause journey. Your forgetfulness could be just the variety of cognitive issues that are caused by the hormonal transition, like “brain fog,” or it could be something more concerning, like dementia, which affects more women+ than men. So, what’s the difference? Learn about how the menopause journey changes your brain and when to talk to your doctor about dementia.
Menopause brain fog vs. dementia
During the menopause journey, many women experience “brain fog.” That’s because the hormonal transition affects more than just your ovaries. It also changes your brain! You may even experience other neurological menopause symptoms like depression, anxiety, and even hot flashes.
Brain fog during menopause is usually temporary and typically does not increase your risk of developing dementia later in life.
Still, brain fog can be debilitating, making it hard to remember information and impacting you personally and professionally. And it may leave you asking yourself: how do I know if my brain fog is actually dementia?
People with brain fog and/or dementia most commonly report memory loss as a symptom, but other symptoms of dementia frequently extend far beyond memory loss.
Dementia symptoms often include:
- difficulty communicating
- getting lost in familiar areas
- trouble paying bills or handling money
- trouble planning or completing routine daily tasks
- acting impulsively
Dementia symptoms can also lead to issues with movement or balance.
Even if it’s “just” brain fog that you’re experiencing, it’s important to know about the risks of dementia, as the menopause journey can increase your risk of developing it. And, there are lifestyle factors that can help prevent it which you can jump to now if you want to focus on those healthy brain habits.
What is dementia?
Dementia is the umbrella term for several conditions that impair your ability to think, remember, problem-solve, or socialize. It’s dementia when these declines are severe enough to affect your daily life.
Unfortunately, dementia is a progressive disease that gets worse over time. While symptoms can be delayed and managed to some degree, there is no cure for it.
Dementia disproportionately affects women+.
Source: Alzheimer's Society
In the U.S., dementia was the leading cause of death for women+ from 2014 to 2020. In 2021, it dropped to the third leading cause of death for women+ due to COVID and heart disease.
Types of dementia
There are several types of dementia, all of which affect your brain a bit differently:
- Alzheimer’s disease
- Vascular dementia
- Lewy body dementia
- Frontotemporal dementia (FTD)
- Mixed dementia
Let’s explore each one.
What is Alzheimer’s disease?
Alzheimer’s disease is the most common type of dementia. It makes up 60 to 80% of all dementias and disproportionately affects women+.
It occurs when a certain type of protein builds up in the brain. This accumulation decreases the brain’s ability to send and translate signals.
Impact of Alzheimer’s
With Alzheimer’s, you begin to have memory loss over time. You may also experience:
- Difficulty finding or saying words
- Depression
- Anxiety
- Hallucinations
- Delusions
- Sleep disturbances
- Loss of impulse control, which can lead to inappropriate sexual behaviors or aggressive outbursts like hitting or yelling.
As Alzheimer’s disease progresses, you may experience physical challenges as well. You may walk more slowly and be less steady. You may also have difficulty swallowing and eating or lose control of your bladder or bowels.
For reasons that aren’t clear, twice as many women+ have Alzheimer’s compared to men. While women+ have a greater survival rate, they have more dementia-related disability. Overall, their cognitive issues are more severe and pronounced. So, women+ tend to start to lose their autonomy sooner than men.
Vascular dementia
Vascular dementia is the second most common form of dementia, equally affecting both men and women+. It can develop suddenly or over time.
It’s caused by a decrease in blood flow to certain parts of your brain.
Examples of causes of vascular dementia are stroke and the narrowing of certain arteries that bring blood to your brain.
If you have vascular dementia, you may have trouble:
- Completing tasks that used to be easy
- Learning something new
- Following instructions
You may also notice a change in your mood or behavior. Depression, irritability, and anger are common among those with this type of dementia.
Lewy body dementia
Lewy body dementia occurs when proteins called Lewy bodies deposit in the brain, affecting thinking, movement, and behavior.
This type of dementia is less common in women+ and is usually associated with Parkinson’s disease.
The symptoms are similar to Alzheimer’s disease, but you often also experience visual hallucinations, rapid eye movement, and Parkinsonism symptoms.
These symptoms include rigid muscles, tremors (involuntary shaking), slowed movement, or balance issues.
Frontotemporal dementia (FTD)
Frontotemporal dementia (FTD) is caused by damage to brain cells in your frontal and temporal lobes.
Damage to your frontal lobe can lead to personality changes, loss of impulse control, and difficulty concentrating.
Damage to your temporal lobe can lead to issues with memory, understanding language, recognizing objects, and processing emotions.
Frontotemporal dementia is often experienced as presenile dementia, affecting people younger than 65 years old. Roughly 60% of people with FTD are 45 to 64 years old.
Mixed dementia
Mixed dementia is when you have more than one type of dementia. Most commonly, people have Alzheimer’s disease and vascular dementia.
Experts can’t say how common mixed dementia is because it’s hard to diagnose while you are alive. Evidence of mixed dementia is usually found if an autopsy is performed.
However, some studies suggest that more than 50% of those who are diagnosed with Alzheimer’s disease may have another form of dementia as well.

How is menopause linked to dementia?
During the menopause journey, you may experience cognitive issues like brain fog which can lead to trouble concentrating or forgetfulness.
While some forgetfulness may be part of aging and the menopause journey, dementia is NOT a natural part of getting older.
But there is a possible link between dementia and the menopause journey.
Dementia is just one of several conditions for which women+ are at increased risk during the menopause journey. Osteoporosis and cardiovascular disease are two others.
As you progress to menopause, your estrogen levels decrease rapidly, which means you lose the benefits estrogen has on your body.
Estrogen not only protects your brain but also promotes regeneration and growth. This could put post-menopausal women+ more at risk for developing dementia.
In fact, estrogen could potentially be a reason why dementia is more common in women+ than in men.
As men age, they continue to produce testosterone, which is ultimately converted to estrogen in their brains. This means older men actually have higher estrogen levels in their bodies than post-menopausal women.
But does this mean you are more at risk for developing dementia if you went through menopause early?
Unfortunately, the association between age at menopause and risk of dementia is still unclear. Most studies find that women+ who go through menopause at an age older than 55 years old are less likely to have dementia compared to those who have onset before age 40.
One potential contributory factor to the difference is women+ who go through menopause before age 45 are 50% more likely to have a stroke, which would increase their potential risk of developing vascular dementia.
Other studies suggest that it’s not about your age at menopause. Rather, the length of one’s reproductive years may be a more conclusive marker for dementia risk.
If you have a fertility duration of over 40 years, you may be less likely to develop dementia compared to women+ who had a fertility duration less than 30 years because of more years of the protective benefit of estrogen.
Regardless, more studies are needed to determine just how connected menopause and dementia are.
Can hormone therapy (HT) prevent dementia?
You may have read contrasting claims that hormone therapy (HT) can both increase and decrease your risk of developing dementia. To add to the confusion, HT has fallen in and out of favor for decades now. So, who exactly could lower their dementia risk with HT?
Sadly, evidence for HT continues to be contradictory. However, most studies seem to support the “critical window hypothesis,” which states that there’s an opportune time to start HT, typically earlier rather than later in the journey.
Starting HT closer to menopause may be beneficial to your cognition.
Ideally, HT should be started within a year of menopause onset. But potential benefits could still be seen if it’s started within 5 years. Starting HT more than 5 years out from menopause onset showed no cognitive benefit.
Age may also be a factor.
Some studies found that HT increases your risk of dementia if you’re 65 or older. Other studies showed no benefit in this age group.
In general, HT is not given to older women+ to specifically prevent cognitive decline. Keep in mind that it may be appropriate for other situations.
The type of HT can also make a difference.
HT is usually a form of estrogen or progesterone, given either alone or in combination. There is evidence that using either alone is associated with less risk of dementia compared to using a combination.
Also, taking HT for more than 5 to 10 years was shown to be cognitively protective, which wasn’t the case for shorter durations.
Testosterone for post-menopausal women?
Testosterone has been studied more recently in post-menopausal women. Findings indicate promising results regarding improvement in learning and memory.
Many women also report it improves their mood, concentration, and energy. It may also help with sexual function, especially libido, and overall physical health.
APOE4 genotype and HT
Unfortunately, there are numerous factors to take into account when looking at HT. Studies and analyses that show an increase in risk of dementia with HT tend to be less specific. They often do not focus on sub-groups of women+, such as age at menopause, fertility duration, or when HT was started in relation to menopause onset.
However, we are starting to see promising new studies that reveal a type of gene may make a difference.
While studies remain limited, we are beginning to see some progress in this area.
Some studies showed that women+ who have the APOE4 genotype benefited from HT.
The APOE4 genotype can increase your risk of Alzheimer’s disease by 12 to 15 times compared to those with other types.
Those with the APOE4 genotype who took HT performed better on cognitive tests and had larger brain volumes. Ultimately, HT had the potential to prevent or delay Alzheimer’s disease in this sub-group of women+.
While these findings certainly show that HT can benefit some women+, more studies are needed that specifically focus on the various factors that may influence how beneficial HT is. These include:
- race
- socioeconomic status
- fertility duration
- type of HT
- whether menopause was surgically induced
- other genetic/medical factors

What are other risk factors for dementia?
Beyond menopause, there are other factors that can increase your risk of dementia. These include:
- Older age
- Being a woman+
- Alcohol use disorder
- Being socially isolated
- Low vitamin D levels
- Race/ethnicity
- Hispanic and Black people are 1.5 to 2 times more likely to suffer from dementia compared to non-Hispanic whites.
- Genes
- Being a carrier of APOE4 genotype increases your risk of dementia by 12 to 15 times.
- Not hearing well
- For those with a hearing impairment, the risk is greatest for those who do not wear hearing aids.
- Certain infections
- Studies have found people who had infection-related hospitalization with delirium are more likely to develop dementia.
- Those who had exposure to Helicobacter pylori were 11% more likely to develop Alzheimer’s disease.
- Other medical conditions, including:
- Heart disease
- Stroke
- Parkinson’s disease
- Huntington’s disease
- Head injury
There are groups of people who are disproportionately more likely to suffer from dementia
What health disparities exist in dementia?
Anyone who faces barriers to health may be more at risk for developing dementia. Conversely, a lower risk of dementia is associated with a higher education and income level.
Experiencing cognitive decline is nearly 3 times greater for those who do not have a high school diploma compared to those with a college-level degree.
The reasons why education and income can affect cognitive health aren’t well established. However, some studies suggest it could be because a higher education gives you more cognitive reserves. This can make it easier to compensate for any cognitive declines.
Other studies suggest this has more to do with barriers to healthcare overall, e.g., in Black women.
Race/ethnicity
Another major health disparity when it comes to dementia is race/ ethnicity.
Black and Hispanic people are more likely to suffer from dementia compared to non-Hispanic whites. They are also more likely to have a missed or delayed diagnosis.
Hispanics are almost twice as likely to suffer from dementia compared to non-Hispanic whites. They also tend to be the youngest (79 years old) when diagnosed with dementia, while non-Hispanic whites tend to be the oldest (82 years old). But Hispanics tend to live the longest after being diagnosed.
Getting diagnosed can be a barrier in itself. One study showed that members of the Black population are 35% less likely to be diagnosed with dementia, despite being 1.5 to 3 times more likely to develop it compared to non-Hispanic whites. Time to diagnosis was also 11% longer in Black patients and 40% longer in those who were Hispanic compared to non-Hispanic whites.
Beyond diagnosis, these two groups have other barriers to cognitive health. They’re less likely to be prescribed anti-dementia or other medications for their dementia. And they were more likely to stop taking their medications. The exact reasons behind this are unclear. But one study found a higher percentage of Black and Hispanics believe dementia is a normal part of aging. This misconception could lead them to stop taking their medication if they experience side effects or don’t see the benefits of taking it.
Blacks and Hispanics also have more and longer hospital stays due to their dementia. Additionally, they are more likely to be admitted to a long-term care facility with lower quality scores and higher hospital readmission rates. Ultimately, these disadvantages also lead to higher financial stress.
To compound the issue, studies are emerging that cumulative lifetime stress, early life conditions, and living in a disadvantaged neighborhood could disproportionately contribute to dementia risk for Black people. They were shown to experience about 60% more stressful experiences in their lifetime compared to non-Hispanic whites. They were also found to be at higher risk for dementia if they were born in a state with a high infant mortality rate. Non-Hispanic whites did not have the same dementia risk.
Know your risk and be proactive
Knowing your risk for dementia is important if you belong to a group in which health disparities are seen. Being aware puts you in a better position to combat them and get the care you need and deserve.
It also means that actions you can take to optimize your health and lifestyle over which you have a greater degree of control, like living a healthier lifestyle and managing chronic conditions effectively, become even more critical.
Recognizing the early signs of dementia and seeking help could lead to an earlier diagnosis and potentially a greater quality of life for a longer period of time.
When should I seek medical attention for my cognitive concerns?
Dementia is not a normal part of aging. It affects everyone differently, and it can sometimes be hard to diagnose in its early stages.
However, an early diagnosis can maximize the benefits of medical treatments and lifestyle modifications. So, it’s never too soon to speak with your doctor about your cognitive health concerns.
Some symptoms to keep an eye out for are:
- Changes in your handwriting.
- Confusion with daily tasks like doing the groceries.
- Struggling with language and communication, like forgetting words.
- Changes in behavior, like becoming easily annoyed or anxious, far out of proportion to the trigger for those emotional responses.
Speak with your healthcare provider if you have concerns about your cognition or if your symptoms are getting worse or interfering with your normal daily tasks.
7 ways to help prevent dementia
You can never get started too early to take action to reduce your chances of developing dementia. For example, Alzheimer’s disease actually begins up to 20 years before symptoms appear.
Given the risk to women+ of developing dementia, your cognitive health should be a priority. There are ways to improve your overall memory and brain health.
These tips can help with menopausal brain fog and help reduce your risk of or prevent dementia.
- Exercise.
- Don’t drink alcohol in excess or eliminate it together.
- Eat a balanced diet.
- Get enough vitamin D.
- Take a daily multivitamin.
- Socialize.
- Use hearing aids if needed.
Let’s break down each one.
1. Exercise
Exercise improves memory and cognition by increasing blood flow to your brain. Some studies show that active adults are almost half as likely to experience cognitive decline when compared with inactive adults.
And a recent study found Kundalini yoga had a positive impact on memory and cognition in older women.
For tips on how to stay active, visit the CDC for resources on how to get more physical activity. Here are some exercises for women in menopause to get you started.
2. Don’t drink alcohol in excess or eliminate it altogether.
Drinking alcohol in excess has been shown to increase your risk of dementia by decreasing the amount of your brain’s white matter. White matter helps transmit signals that affect your ability to focus, learn, and problem-solve.
However, a strong link between moderate consumption and dementia has not been established.
That being said, several health-related groups and organizations have indicated a belief there is no safe level of alcohol consumption, even when some of its benefits are taken into account.
If you do decide to drink, limit your alcohol consumption to no more than 1 drink per day for women+.
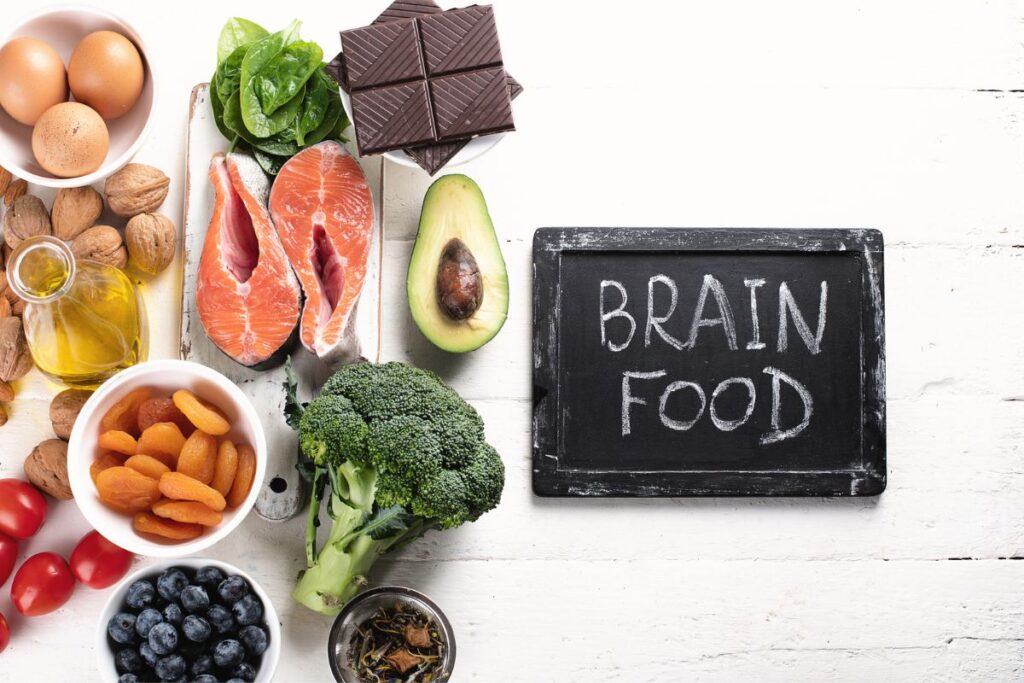
3. Eat a balanced diet.
Like the rest of your body, your brain needs nutrients to work its best. A healthy, well-balanced diet can help.
Current recommendations say sugar and saturated fats should be limited to less than 10% of your diet.
Sodium intake should be limited to less than 2300 mg daily.
You should also incorporate green leafy vegetables, fruits, whole grains, and nuts into your diet. The MIND (Mediterranean-DASH Diet Intervention for Neurodegenerative Delay) diet is one specifically focused on brain health.
4. Get enough vitamin D.
Only about 35% of people in the U.S. have sufficient vitamin D levels. Some studies suggest that low vitamin D could contribute to cognitive issues and dementia, but the reasoning for this is not clear.
While it may be due to direct causes, indirect causes may also be a factor. For instance, low vitamin D may increase your risk of certain infections, which in turn, can put you at risk for developing dementia.
Of note, severe vitamin D deficiency is seen much more commonly in the Black population. Knowing that health disparities are seen in those with dementia, impacting more Black people than non-Hispanic whites, this is something Black women should talk to their doctor about.
In fact, given how common vitamin D deficiency is, all women+ should consult with their healthcare practitioner about getting their levels checked with a blood test.
To maintain adequate vitamin D levels, you should get 10 to 30 minutes of direct sunlight a day. If this is not possible, consider taking a vitamin D supplement and also check out foods that are higher in vitamin D.
5. Take a daily multivitamin.
Taking a daily multivitamin has been shown to improve general cognition and memory. It also appears to help prevent further cognitive decline.
Even though it does not help with attention or focus, you may want to consider taking a daily multivitamin for your overall brain health.
6. Socialize
Social isolation can increase your risk of developing dementia by as much as 50%. Unfortunately, even before the COVID-19 pandemic, nearly 25% of older adults were considered socially isolated. And 1 in 3 adults felt lonely.
Social isolation affects more than your brain health. It can also increase your risk of heart disease, stroke, and mental health conditions.
So, it’s important to find activities in which you can engage on a regular basis. For tips on how to improve social connection, visit the CDC.
7. Use hearing aids if needed.
Hearing loss can increase your risk of dementia. The reason is believed to be that people with hearing loss have less brain stimulation. They can also become socially isolated because communicating is more difficult or frustrating.
If you are experiencing hearing loss, using hearing aids may reduce your risk of developing dementia.
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
"*" indicates required fields

Don’t wonder and worry. Take action.
So, if you find yourself wondering “Why am I forgetting things?”, it could be related to the menopause journey. But it could also be something more serious. If you have concerns about memory loss or cognitive health, speak with your doctor and advocate for the care you need and deserve.
The hormonal transition is an important stage of life to focus on your health and well-being. Doing so can help reduce the severity of menopausal symptoms and the risk of chronic conditions, including dementia. It also sets you up for a more vibrant life in the years ahead. Don’t wait to make a change for the better!
What is Dementia? Symptoms, Types, and Diagnosis | National Institute on Aging
What Is Dementia? | Alzheimer’s Association
Hormones and dementia risk | Alzheimer’s Society
Tai S, Chi Y, Lo Y, Chien Y, Kwachi I, Lu T. Ranking of Alzheimer’s disease and related dementia among the leading causes of death in the US varies depending on NCHS or WHO definitions. Alzheimers Dement Diagn Assess Dis Monit. 2023;15(2):e12442. doi:10.1002/dad2.12442
The later stage of dementia | Alzheimer’s Society
Why is dementia different for women? | Alzheimer’s Society
Derreberry TM, Holroyd S. Dementia in Women. Med Clin North Am. 2019;103(4):713-721. doi:10.1016/j.mcna.2019.02.004
What Is Lewy Body Dementia? Causes, Symptoms, and Treatments | National Institute on Aging
What Are Frontotemporal Disorders? Causes, Symptoms, and Treatment | National Institute on Aging
Mixed Dementia | Alzheimer’s Association
Conde DM, Verdade RC, Valadares ALR, Mella LFB, Pedro AO, Costa-Paiva L. Menopause and cognitive impairment: A narrative review of current knowledge. World J Psychiatry. 2021;11(8):412-428. doi:10.5498/wjp.v11.i8.412
Brann DW, Dhandapani K, Wakade C, Mahesh VB, Khan MM. Neurotrophic and Neuroprotective Actions of Estrogen: Basic Mechanisms and Clinical Implications. Steroids. 2007;72(5):381-405. doi:10.1016/j.steroids.2007.02.003
Vermeulen A, Kaufman JM, Goemaere S, van Pottelberg I. Estradiol in elderly men. Aging Male Off J Int Soc Study Aging Male. 2002;5(2):98-102.
Hao W, Fu C, Dong C, et al. Age at menopause and all-cause and cause-specific dementia: a prospective analysis of the UK Biobank cohort. Hum Reprod. 2023;38(9):1746-1754. doi:10.1093/humrep/dead130
Liao H, Cheng J, Pan D, et al. Association of earlier age at menopause with risk of incident dementia, brain structural indices and the potential mediators: a prospective community-based cohort study. eClinicalMedicine. 2023;60. doi:10.1016/j.eclinm.2023.102033
Yoo JE, Shin DW, Han K, et al. Female reproductive factors and the risk of dementia: a nationwide cohort study. Eur J Neurol. 2020;27(8):1448-1458. doi:10.1111/ene.14315
Conde DM, Verdade RC, Valadares ALR, Mella LFB, Pedro AO, Costa-Paiva L. Menopause and cognitive impairment: A narrative review of current knowledge. World J Psychiatry. 2021 Aug 19;11(8):412-428. doi: 10.5498/wjp.v11.i8.412. PMID: 34513605; PMCID: PMC8394691.
Nerattini M, Jett S, Andy C, Carlton C, Zarate C, Boneu C, Battista M, Pahlajani S, Loeb-Zeitlin S, Havryulik Y, Williams S, Christos P, Fink M, Brinton RD and Mosconi L (2023) Systematic review and meta-analysis of the effects of menopause hormone therapy on risk of Alzheimer’s disease and dementia. Front. Aging Neurosci. 15:1260427. doi: 10.3389/fnagi.2023.1260427
Vinogradova Y, Dening T, Hippisley-Cox J, Taylor L, Moore M, Coupland C. Use of menopausal hormone therapy and risk of dementia: nested case-control studies using QResearch and CPRD databases. BMJ. 2021 Sep 29;374:n2182. doi: 10.1136/bmj.n2182. PMID: 34588168; PMCID: PMC8479814.
Testosterone improves verbal learning and memory in post-menopausal women. Endocrine Society. 2013.
Scott A, Newson L. Should we be prescribing testosterone to perimenopausal and menopausal women? A guide to prescribing testosterone for women in primary care. Br J Gen Pract. 2020;70(693):203-204. doi:10.3399/bjgp20X709265
Wu M, Li M, Yuan J, et al. Postmenopausal hormone therapy and Alzheimer’s disease, dementia, and Parkinson’s disease: A systematic review and time-response meta-analysis. Pharmacol Res. 2020;155:104693. doi:10.1016/j.phrs.2020.104693
Sung YF, Tsai CT, Kuo CY, et al. Use of Hormone Replacement Therapy and Risk of Dementia. Neurology. 2022;99(17):e1835-e1842. doi:10.1212/WNL.0000000000200960
Saleh RNM, Hornberger M, Ritchie CW, Minihane AM. Hormone replacement therapy is associated with improved cognition and larger brain volumes in at-risk APOE4 women: results from the European Prevention of Alzheimer’s Disease (EPAD) cohort. Alzheimers Res Ther. 2023;15(1):10. doi:10.1186/s13195-022-01121-5
Depypere H, Vergallo A, Lemercier P, et al. Menopause hormone therapy significantly alters pathophysiological biomarkers of Alzheimer’s disease. Alzheimers Dement. 2023;19(4):1320-1330. doi:10.1002/alz.12759
Wong GRM, Lee EJA, Liaw QY, Rajaram H. The role of oestrogen therapy in reducing risk of Alzheimer’s disease: systematic review. BJPsych Open. 2023 Oct 17;9(6):e194. doi: 10.1192/bjo.2023.579. PMID: 37846476; PMCID: PMC10594166.
Stefanowski B, Kucharski M, Szeliga A, et al. Cognitive decline and dementia in women after menopause: Prevention strategies. Maturitas. 2023;168:53-61. doi:10.1016/j.maturitas.2022.10.012
MD AEB. A fresh look at risks for developing young-onset dementia | Harvard Health
Sommer I, Griebler U, Kien C, et al. Vitamin D deficiency as a risk factor for dementia: a systematic review and meta-analysis. BMC Geriatr. 2017;17(1):16. doi:10.1186/s12877-016-0405-0
Cantuaria ML, Pedersen ER, Waldorff FB, et al. Hearing Loss, Hearing Aid Use, and Risk of Dementia in Older Adults. JAMA Otolaryngol– Head Neck Surg. 2024;150(2):157-164. doi:10.1001/jamaoto.2023.3509
Kornblith E, Bahorik A, Boscardin WJ, Xia F, Barnes DE, Yaffe K. Association of Race and Ethnicity With Incidence of Dementia Among Older Adults. JAMA. 2022 Apr 19;327(15):1488-1495. doi: 10.1001/jama.2022.3550. PMID: 35438728; PMCID: PMC9020215.
Study reveals how APOE4 gene may increase risk for dementia | National Institute on Aging
Pendlebury ST, Luengo-Fernandez R, Seeley A, Downer MB, McColl A, Rothwell PM. Infection, delirium, and risk of dementia in patients with and without white matter disease on previous brain imaging: a population-based study. Lancet Healthy Longev. 2024;5(2):e131-e140. doi:10.1016/S2666-7568(23)00266-0
Douros A, Ante Z, Fallone CA, et al. Clinically apparent Helicobacter pylori infection and the risk of incident Alzheimer’s disease: A population-based nested case-control study. Alzheimers Dement. n/a(n/a). doi:10.1002/alz.13561
Social Determinants of Health and Alzheimer’s Disease and Related Dementias | Centers for Disease Control and Prevention. Published September 1, 2023. Accessed March 7, 2024.
Wilson RS, Yu L, Lamar M, Schneider JA, Boyle PA, Bennett DA. Education and cognitive reserve in old age. Neurology. 2019 Mar 5;92(10):e1041-e1050. doi: 10.1212/WNL.0000000000007036. Epub 2019 Feb 6. PMID: 30728309; PMCID: PMC6442015.
Findley CA, Cox MF, Lipson AB, Bradley R, Hascup KN, Yuede C and Hascup ER (2023) Health disparities in aging: Improving dementia care for Black women. Front. Aging Neurosci. 15:1107372. doi: 10.3389/fnagi.2023.1107372
Lin PJ, Daly AT, Olchanski N, et al. Dementia Diagnosis Disparities by Race and Ethnicity. Med Care. 2021;59(8):679-686. doi:10.1097/MLR.0000000000001577
Chen Y, Crimmins E, Ferido P, Zissimopoulos JM. Racial/Ethnic Disparities in Length of Life after Dementia Diagnosis: an 18-Year Follow-up Study of Medicare Beneficiaries. Lancet Reg Health – Am. 2022;8. doi:10.1016/j.lana.2021.100179
Findley CA, Cox MF, Lipson AB, et al. Health disparities in aging: Improving dementia care for Black women. Front Aging Neurosci. 2023;15:1107372. doi:10.3389/fnagi.2023.1107372
Hinton L, Tran D, Peak K, Meyer OL, Quiñones AR. Mapping racial and ethnic healthcare disparities for persons living with dementia: A scoping review. Alzheimers Dement. n/a(n/a). doi:10.1002/alz.13612
Chin AL, Negash S, Hamilton R. Diversity and disparity in dementia: the impact of ethnoracial differences in Alzheimer disease. Alzheimer Dis Assoc Disord. 2011 Jul-Sep;25(3):187-95. doi: 10.1097/WAD.0b013e318211c6c9. PMID: 21399486; PMCID: PMC3396146.
Stressful Life Experiences Age the Brain by Four Years, African Americans Most at Risk | AAIC 2018. AAIC. Accessed February 18, 2024.
Five things you should know about dementia | Alzheimer’s Society
Saha R et.al. Handwriting Analysis for Early Detection of Alzheimer’s Disease. 02 June 2020 https://doi.org/10.1002/9781119544487.ch18
Alzheimer’s Association. 2024 Alzheimer’s Disease Facts and Figures. Alzheimers Dement 2024;20(5)
Konopka LM. How exercise influences the brain: a neuroscience perspective. Croat Med J. 2015;56(2):169-171. doi:10.3325/cmj.2015.56.169
University of California – Los Angeles Health Sciences. Yoga provides unique cognitive benefits to older women at risk of Alzheimer’s disease. February 2024
Omura JD, Brown DR, McGuire LC, Taylor CA, Fulton JE, Carlson SA. Cross-sectional association between physical activity level and subjective cognitive decline among US adults aged ≥45 years. 2015. Prev Med. 2020;141:106279. doi:10.1016/j.ypmed.2020.106279
Physical Activity Basics | Centers for Disease Control and Prevention
Alcohol and the risk of dementia | Alzheimer’s Society
Rheumatology TL. Alcohol and health: all, none, or somewhere in-between? Lancet Rheumatol. 2023;5(4):e167. doi:10.1016/S2665-9913(23)00073-5
Alcohol Use and Your Health| Centers for Disease Control and Prevention
Top 10 Things You Need to Know About the Dietary Guidelines for Americans, 2020-2025 | Dietary Guidelines for Americans
Diet Review: MIND Diet | The President and Fellows of Harvard College
Cui A, Xiao P, Ma Y, Fan Z, Zhou F, Zheng J, Zhang L. Prevalence, trend, and predictor analyses of vitamin D deficiency in the US population, 2001-2018. Front Nutr. 2022 Oct 3;9:965376. doi: 10.3389/fnut.2022.965376. PMID: 36263304; PMCID: PMC9573946.
Sommer, I., Griebler, U., Kien, C. et al. Vitamin D deficiency as a risk factor for dementia: a systematic review and meta-analysis. BMC Geriatr 17, 16 (2017). https://doi.org/10.1186/s12877-016-0405-0
Gunville CF, Mourani PM, Ginde AA. The Role of Vitamin D in Prevention and Treatment of Infection. Inflamm Allergy Drug Targets. 2013;12(4):239-245.
Ames BN, Grant WB, Willett WC. Does the High Prevalence of Vitamin D Deficiency in African Americans Contribute to Health Disparities? Nutrients. 2021 Feb 3;13(2):499. doi: 10.3390/nu13020499. PMID: 33546262; PMCID: PMC7913332.
Vitamin D | The President and Fellows of Harvard College
Vyas CM, Manson JE, Sesso HD, et al. Effect of multivitamin-mineral supplementation versus placebo on cognitive function: results from the clinic subcohort of the COcoa Supplement and Multivitamin Outcomes Study (COSMOS) randomized clinical trial and meta-analysis of 3 cognitive studies within COSMOS. Am J Clin Nutr. 2024;0(0). doi:10.1016/j.ajcnut.2023.12.011
Loneliness and Social Isolation Linked to Serious Health Conditions | Centers for Disease Control and Prevention
Improving Social Connectedness | Centers for Disease Control and Prevention
Cantuaria ML, Pedersen ER, Waldorff FB, Wermuth L, Pedersen KM, Poulsen AH, Raaschou-Nielsen O, Sørensen M, Schmidt JH. Hearing Loss, Hearing Aid Use, and Risk of Dementia in Older Adults. JAMA Otolaryngol Head Neck Surg. 2024 Feb 1;150(2):157-164. doi: 10.1001/jamaoto.2023.3509. PMID: 38175662; PMCID: PMC10767640.
Hearing aids slow cognitive decline in people at high risk | National Institutes of Health (NIH). Published August 7, 2023. Accessed February 8, 2024.
You may also like…

Power Through Menopausal Changes with this RAIN Mindfulness Technique
The RAIN mindfulness technique can help you power through menopausal changes with a positive mindset. Read or listen to this script.

Missing Your Life Before Menopause? How to Manage The Grief and Loss
Do you ever think about life before menopausal symptoms? If you feel a sense of loss or grief, try these emotional coping strategies.

17 Menopausal Anxiety Treatment Options To Ease Your Mind
Feeling anxious during the menopause journey? Try these 16 anxiety treatment options to ease your mind of worry and fear.

