Since you’ve started your menopause journey, have your fear and worry skyrocketed? Is your mind dwelling on everything going wrong, or what could go wrong? Perhaps racing thoughts keep you up at night. On bad days, it may be hard to leave the house. Sometimes, it’s hard to breathe. Or you feel like your heart is pounding and your chest is being crushed. Thoughts that seem irrational won’t go away. And your relationships are suffering.
Know that you are not alone! Anxiety and menopause can go hand in hand. While you may be overwhelmed with anxiety, it does not have to define you. You have SUPERpowers, and pausitive health is here to help you make sense of your anxiety and how it can affect other menopausal symptoms.
Does menopause cause anxiety?
Given the hormonal connection to anxiety, it’s not surprising it’s one of the many menopausal symptoms you may experience during this stage of life.
Those who have more severe menopausal symptoms tend to have worse anxiety. For example, hot flashes can trigger anxiety.
You are not alone!
25% of menopausal women+ suffer from anxiety.
Can anxiety cause menopause symptoms?
Yes. Anxiety can be connected to menopausal symptoms, e.g., palpitations, both causing and/or exacerbating them.
Anxiety is most often associated with these menopausal symptoms:
- hot flashes
- heart palpitations
- panic attacks
- body pain
- genitourinary syndrome of menopause (GSM)
- depression
- stress
Anxiety and hot flashes
While anxiety and hot flashes are strongly linked, determining which came first is hard. They can both actually make the other worse.
You’re 3 times more likely to have hot flashes if your anxiety symptoms are physical ones.
The physical anxiety symptoms that can cause hot flashes include:
- fatigue
- headaches
- muscle aches
- stomach upset
If your anxiety levels are high, your risk of having anxiety-related hot flashes increases.
Heart palpitations
In addition to hot flashes, you may also experience heart palpitations.
Heart palpitations may feel like your heart is:
- racing
- fluttering
- pounding
- skipping beats
Both anxiety and hot flashes can increase the likelihood of having heart palpitations.
If your vasomotor symptoms (hot flashes and night sweats) are severe, your heart palpitations may be more severe or more frequent. This is true regardless of the stage of menopause you’re in.
The question to be answered is whether it’s your heart (which can also be impacted during the menopause journey) or anxiety?
When a person experiences these symptoms, they may be referred to a cardiologist who will determine if a cardiac stress test or other procedures are needed to evaluate their heart.

Panic attacks
Anxiety can also cause panic attacks, often referred to as panic disorder, a type of anxiety.
As you go through the menopause journey, your risk of panic attacks goes up.
In one study, 20% of post-menopausal women+ reported a panic attack in the last 6 months.
Symptoms of a panic attack include:
- chest pain
- rapid heart beat
- shortness of breath
- sweating
- a sense of impending doom
It’s not uncommon for people to think they’re having a heart attack.
Studies have found that those sent for a cardiac stress test to rule out a heart problem due to chest pain which turns out to be negative have been found to have a higher prevalence of anxiety (and depression) than people with a positive stress result.
Genitourinary symptoms
Anxiety can also impact urogenital symptoms included in a condition known as genitourinary syndrome of menopause (GSM) like:
- sexual problems
- bladder issues
- vaginal dryness
If you’re experiencing these, talk to your doctor. You don’t have to suffer in silence. Treatment is available!
In fact, during a recent pausitive health webinar, K. Lauren de Winter, MD, FACOG, URPS of Praxis Urogynecology, talked about bladder and vagina symptoms during menopause and possible treatment options.
Body pain
Anxiety can also cause sleep disturbances and body pain.
Anxiety body pain can include aches or stiffness along your:
- spine
- neck
- back
And it can make the aches and pains of conditions like arthritis, migraines, and fibromyalgia, (all of which are more common in women) worse. Anxiety can cause you to tighten your body and also negatively impact your motivation to engage in physical activity, which can increase the frequency and severity of musculoskeletal pain.
These symptoms can certainly make you miserable. But you don’t need to just “suck it up.”
When you become a pausitive health member, you can take advantage of a consultation with a physical therapist and access a library of physical therapist-led videos to address the musculoskeletal discomfort experienced by many women+ as a result of the hormonal changes which occur during the menopause journey These symptoms are known as musculoskeletal syndrome of menopause (MSM).
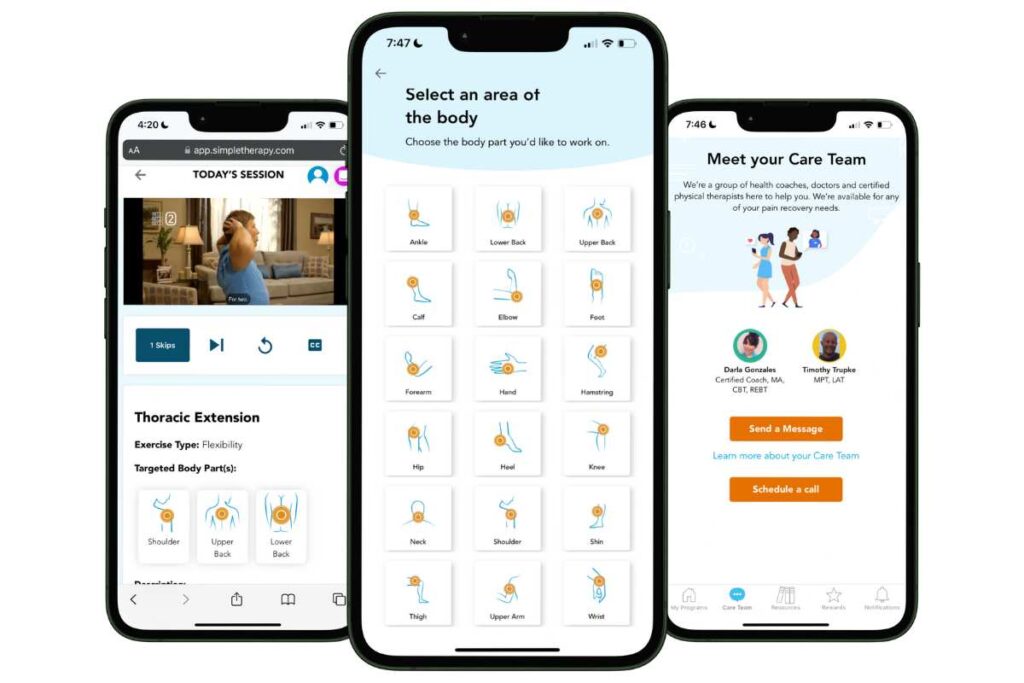
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!
Is it anxiety? Or could it be stress or depression?
During the menopause journey, stress can increase, and your risk of depressive symptoms can increase as well. If you experience either or both, there may be overlapping symptoms with anxiety, which can make it more difficult to identify the root cause(s).
Suffering from one could cause another or make it worse. So, speak with your doctor if you have any signs or symptoms, especially if they’re consistently interfering with your day. Identifying the root cause is important to getting appropriate treatment and resources.
Stress
Stress is your body’s response to an external stressor. It can be acute, like stress related to tight deadlines at work, or chronic, like stress associated with a challenging illness.
If you persistently feel worried or on edge without an external stressor, then your symptoms may be more likely to be related to anxiety.
Depression
Anxiety and depression often happen together. About 50% of people who suffer from one also suffer from the other.
Anxiety and depression also have many symptoms in common, like:
- Fatigue
- Irritability
- Physical discomfort (aches and pains)
- Difficulty concentrating
- Sleep issues
But with depression, you may feel persistently sad. You could feel guilty, worthless, or hopeless. Or have suicidal ideation. Depression could also show up as anger.
Call 9-8-8
How does mental health impact physical health?
People often talk about their mental and physical health as being two separate categories. But they’re highly intertwined.
Physical health conditions, especially ones that are long-lasting, can increase your risk of mental health issues. For example, people with chronic conditions are more likely to experience depression and/or anxiety.
On the flip side, if you suffer from depression or anxiety, you’re more likely to have:
- Chest pain
- Heart disease (high blood pressure, heart attack, stroke)
- Diabetes
- Asthma
- Arthritis
- Cancer
Mental health issues can also increase your chances of making poor lifestyle choices, like:
- Smoking
- Self-medicating with alcohol
- Soothing with food
- Lacking motivation to exercise
Ultimately, these habits lead to poorer health and a higher risk of premature death.
Therefore, it’s essential to work with your doctor to get an accurate diagnosis and the treatment you need in a timely fashion to live a happier and healthier life.
Do something about menopause and anxiety
You have options and do not have to suffer! The interconnectedness of the two can make it difficult to pinpoint what’s causing you to feel a certain way.
Talk with your healthcare practitioner, and consider a menopause-trained clinician from The Menopause Society. You can also access a menopause-trained clinician thorugh our collaboration with Pandia Health. The cost is discounted through the pausitive health membership program.
Make a change for the better with pausitive health! We also offer members complimentary access to SimpleTherapy, which can help ease anxiety, stress, depression, and any related aches and pains.
Don’t miss out on these features, available for a limited time!
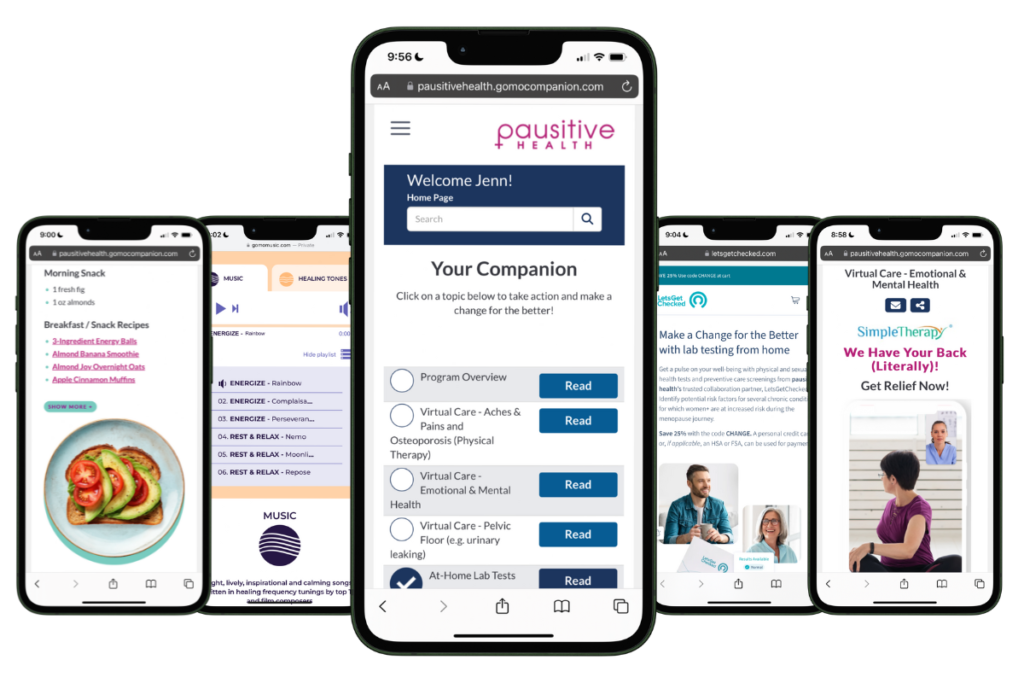
Free Support
For Your Menopause Journey!
Only available for a limited time!
Access a one-stop menopause journey digital destination that provides personalized text messages that focus on educational topics you select and offers many other features such as a diet assessment with recommendations, solutions from collaboration partners to address menopausal aches and pains (the musculoskeletal syndrome of menopause – MSM), pelvic floor issues, virtual care, lifestyle tools, and a supportive community.
Generalized Anxiety Disorder | National Institute of Mental Health
Bremer E. Anxiety in Menopause: A Qualitative Inquiry. 2018. Dissertation Virginia Commonwealth University.
Freeman, Ellen W. PhD; Sammel, Mary D. ScD. Anxiety as a risk factor for menopausal hot flashes: evidence from the Penn Ovarian Aging cohort. Menopause 23(9):p 942-949, September 2016. | DOI: 10.1097/GME.0000000000000662
Enomoto, Haruka BS; Terauchi, Masakazu MD, PhD, NCMP; Odai, Tamami MD, PhD; Kato, Kiyoko BS; Iizuka, Makoto MD, PhD; Akiyoshi, Mihoko PhD; Miyasaka, Naoyuki MD, PhD. Independent association of palpitation with vasomotor symptoms and anxiety in middle-aged women. Menopause 28(7):p 741-747, July 2021. | DOI: 10.1097/GME.0000000000001776
Exercise Stress Test | Cleveland Clinic
Smoller JW, Pollack MH, Wassertheil-Smoller S, Barton B, Hendrix SL, Jackson RD, Dicken T, Oberman A, Sheps DS; Women’s Health Initiative Investigators. Prevalence and correlates of panic attacks in postmenopausal women: results from an ancillary study to the Women’s Health Initiative. Arch Intern Med. 2003 Sep 22;163(17):2041-50. doi: 10.1001/archinte.163.17.2041. PMID: 14504117.
Home | Praxis Urogynecology
Chronic Pain | Anxiety & Depression Association of America
Kalin, N. H. The Critical Relationship Between Anxiety and Depression. American Journal of Psychiatry. 2020; 177(5), 365–367. https://doi.org/10.1176/appi.ajp.2020.20030305
Depression and Anger: What’s the Connection? | HealthCentral
Roohafza H, Yavari N, Feizi A, Khani A, Saneian P, Bagherieh S, Sattar F, Sadeghi M. Determinants of depression in non-cardiac chest pain patients: a cross sectional study. Korean J Pain. 2021 Oct 1;34(4):417-426. doi: 10.3344/kjp.2021.34.4.417. PMID: 34593659; PMCID: PMC8494964.
Rohani A, Akbari V, Zarei F. Anxiety and depression symptoms in chest pain patients referred for the exercise stress test. Heart Views. 2011 Oct;12(4):161-4. doi: 10.4103/1995-705X.90903. PMID: 22574242; PMCID: PMC3345151.
Ohrnberger J, Fichera E, Sutton M. The relationship between physical and mental health: A mediation analysis. Soc Sci Med. 2017 Dec;195:42-49. doi: 10.1016/j.socscimed.2017.11.008. Epub 2017 Nov 8. PMID: 29132081.
Find a Menopause Practitioner | The Menopause Society
You may also like…

17 Menopausal Anxiety Treatment Options To Ease Your Mind
Feeling anxious during the menopause journey? Try these 16 anxiety treatment options to ease your mind of worry and fear.

What Is Anxiety, and Why Does It Impact More Women+ Than Men?
Are you experiencing anxiety during the menopausal transition for the first time? Learn about the types of anxiety and why it impacts more women.

How Stress Affects Your Body and Makes Menopause Symptoms Worse
Did you know stress symptoms and menopausal symptoms are similiar?Learn how stress affects your body and how it can mkae menopause symptoms worse.

