“The time to relax is when you don’t have time for it.”
~ Sydney J. Harris
It’s easy to think everything you experience during the menopause journey is related to hormones, especially when you don’t quite feel like yourself. But sometimes stress may be to blame for those so-called “menopause symptoms,” like sleepless nights, mood swings, headaches, and memory issues. They can leave you feeling drained and exhausted, and the hormonal transition is perhaps partly the culprit, but is it all of it? Stress can make menopause symptoms worse and affect your body in other ways too – some obvious and others silent until it’s too late. Knowing what stress can do to your body may be what you need to realize it’s time to slow down, relax, and find a way to take stress seriously.
What You Need To Know: Stress and Menopause
Stress is inevitable, and all the ways it affects you are not always clear. Sometimes you don't realize until it's too late. Some signs of stress can be similar to menopausal symptoms, making it difficult to identify the culprit for how you feel physically and mentally. Stress can also make menopausal symptoms worse. So, be honest with yourself about your stress levels, and don't ignore stress and its very real consequences. It's impacting your body whether you realize it or not.
What is stress?
Stress is how you react, physically and mentally, to a perceived threat or pressure. We all experience stress at some point, but the type of stress has changed over the years.
Thousands of years ago, stress was critical to survival. Your ancestors’ flight-or-fight instinct kicked in to keep them alive during animal encounters, which were short-lived stressful situations.
Now, stressors can be long-lasting, leading to chronic stress. Over time, that can negatively impact your health.
Women+ are more stressed
As a whole, women+ are more affected by stress than men, and it’s increasing, according to surveys.
Women+ are also more likely to experience stress-related symptoms like:
- fatigue
- anxiety
- lack of energy
- headaches
- insomnia
Those are also menopausal symptoms experienced by many women+, making it difficult to distinguish between the two. Plus, if you’re already experiencing any of these symptoms because of menopause, stress can make them worse.
Stress and menopause
In addition to the stressors we already face in day-to-day life, menopause itself can increase stress because you’re dealing with new symptoms and changes in your body related to the hormonal changes taking place during this stage of life.
It’s not just a perception that stress increases throughout the journey; hormonal fluctuations can also increase stress because of the interaction of cortisol and estrogen.

Cortisol and menopause
Cortisol is a stress hormone released by the adrenal glands. It’s usually released during the day, peaking in the morning and then declining.
Cortisol helps you wake up and maintain physical and mental energy throughout the day. But cortisol at high levels (which stress can create) can negatively impact your health.
As you age, cortisol levels (the stress hormone) naturally increase in both men and women.
During the menopause journey, stress hormones are naturally going up while estrogen levels fluctuate until they reach a new and stable low in post-menopause.
Cortisol and estrogen can impact each other and how you feel. The natural fluctuation of estrogen throughout the menopause journey can lead to overall increases or spikes in cortisol. Those spikes may be why you feel different on different days without any apparent reason, independent of your daily stressors.
During the hormonal transition, as estrogen levels go up and down, you may also become more sensitive to stress. What didn’t bother you before may bother you now.
Is it stress or a menopausal symptom?
Given that cortisol and estrogen can affect each other, it’s not surprising that it can sometimes be difficult to tell the difference between a stress symptom and a menopausal symptom.
| Menopause Symptom | Stress Symptom |
|---|---|
| Pain - headache, backache, muscle pain and tension | |
| GI distress | |
| Sleep issues | |
| Negative mindset | |
| Anxiety | |
| Mood swings | |
| Anger and rage | Anger and irritability |
| Dry, itchy skin and acne | Eczema and hives |
| Hair changes - thinning, loss, change in texture | Hair loss |
| Increased cardiovascular disease risks | Increased risk of heart disease and hypertension |
| Impaired response to viral infections, including the flu, HIV, HSV, and CMV | Suppressed immune system |
| Brain fog | Memory impairment |
| Increased risk of dementia | Increased risk of Alzheimer's and other dementias |
| Increased risk of depression, if prior history of or current episode of the condition | Depression |
| Self-medicating, including with alcohol | Self-medicating with alcohol/drugs/tobacco |
| Increased food cravings and weight gain | Increased/decreased appetite and eating, poor nutrition |
| Less activity because of poor sleep, fatigue, aches and pains, depression, or negative mindset | Decreased physical activity |
When you look at this list, all of the menopause-related symptoms can also be stress symptoms, making it more difficult for women+ to identify the root cause or to know if they are actually related to both, with each making the other worse.
Be honest with yourself. To make sure you get the right care, don’t assume your symptoms are related to the menopause journey. It may also be your stress levels.
During a podcast with Under the Sisterhood, Dr. Z. Colette Edwards, Founder and Chief Medical Officer of pausitive health, talked about how stress can impact gut health.
Other symptoms of stress in women+
Stress can also mask itself in other ways, as its impact on the body is widespread.
Women+ can experience changes throughout their reproductive life cycle due to stress.
Your monthly period during perimenopause may:
- stop
- become irregular
- last longer
- become more severe if you experience discomfort during that time of the month
Stress can:
- Complicate reproduction itself, from conception to postpartum
- Decrease your sexual desire
- Worsen certain conditions, like herpes simplex virus (HSV), polycystic ovarian syndrome (PCOS), and menopause
Mental health impact of stress
Looking beyond the physical impact of stress, your mental health can suffer dramatically during times of stress. You may lack motivation, become more irritable or forgetful, have trouble concentrating, or become so overwhelmed you are paralyzed when it comes to making decisions or just getting through the day.
Chronic stress can cause or worsen anxiety as well as lead to burnout. And the higher your stress, the more likely you are to suffer from depression, for which menopausal women+ are already at risk for or exacerbation during the journey in those with a history of the condition.
Once your estrogen levels stabilize (even though it’s at a substantially lower level), you’re less likely to feel stressed, depressed, angry, or enraged.
Women who had a life stressor experienced 21% more hot flashes or night sweats compared to women+ who did not.
This negative impact was present even in the case of women who had emotional support.
Source: PLoS One
Is stress making your menopause symptoms worse?
You’ve had a stressful week. And in case you weren’t dealing with enough, your menopause symptoms are definitely not helping the situation. You can’t help but wonder: can stress cause or worsen menopausal symptoms? The short answer? Yes.
Science shows a link between your level of cortisol and menopause symptoms. The hormonal transition can result in changes to the balance between estrogen, cortisol, and progesterone.
Increased stress also causes cortisol levels to rise.
The end result? Experiencing a stressful event or chronic stress could trigger and/or increase the severity of symptoms or increase your risk for these common menopausal symptoms:
- Hot flashes and night sweats
- Sleeplessness
- Weight gain
- Migraines
- Depression
- Hair loss
Menopause symptoms can also compound stress. If you wake up in the middle of the night, you may be stressed about everything you have to accomplish the next day which will be harder now that you aren’t going to be able to get enough good, quality sleep.
Can stress cause hot flashes?
Hot flashes are one of the most common menopause symptoms, with up to 85% of women experiencing them. The prevalence of hot flashes can vary from group to group, including differences seen relative to geographic locations around the world, stress levels, and race/ethnicity.
Stress can bring on hot flashes or make them more intense. It can also make them last longer, according to the SWAN study.
The study also found that perceived stress, anxiety, and depression are associated with an increased chance of vasomotor symptoms (including hot flashes and night sweats) over the following six years.
And another study indicated high cortisol levels were associated with more frequent hot flashes. When their cortisol levels were flatter throughout the day (remember, they tend to peak in the morning and then decrease), the women+ had more severe hot flashes.

Sleep, stress, and weight gain – a vicious cycle
If the usual cortisol pattern is disrupted, which stress can do, sleep issues may result. Then, a snowball effect can be seen. Stress can lead to higher cortisol levels, which can disrupt sleep, which in turn can increase cortisol levels even more.
Sleep issues can also impact other hormones—leptin and ghrelin—which help control hunger and feelings of satiety (fullness) and signal when it’s time to eat. When these hormone levels are disrupted, weight gain may result and be more difficult to manage.
Weight gain is a common menopause complaint, and excess weight around the belly can increase inflammation in the body and therefore the risk of conditions like heart disease and diabetes.
A Yale study found non-overweight pre-menopausal women who were vulnerable to stress were more likely to have excess internal abdominal fat (visceral fat) and higher levels of the stress hormone, cortisol. Cortisol causes fat to be stored centrally, which can have negative health consequences like increased risk of chronic conditions like cardiovascular disease and metabolic syndrome.
Stress and migraines
Migraines tend to increase during the peri-menopausal stage of the menopause journey, and researchers are studying the impact of stress on these women+.
One study showed that perimenopausal women who had migraines also had higher stress scores. Though it was not conclusive, this finding could indicate an increased risk of migraines with increased stress, particularly given stress is a known trigger for migraines in general.
Is it stress, anxiety, or depression?
During the menopause journey, many women+ develop or experience an exacerbation of preexisting anxiety and/or depression as a result of the hormonal changes which occur during the transition. Stress can make the situation worse.
Since stress is your body’s response to something external, your body should calm down once the stressor is removed.
If you find you’re persistently worrying or feeling on edge, even without an external stressor, then you may have anxiety.
Stress, anxiety, and depression can significantly interfere with your life and health and have overlapping symptoms, so working with your doctor to get to the right diagnosis and identify its root cause is important to get the treatment and resources you need.
Stress and Alzheimer’s
Alzheimer’s disease is a type of dementia, impacting twice as many women+ as men.
Researchers believe the menopause journey increases the risk of developing dementias like Alzheimer’s disease.
And if you’re stressed, you can add it as another potential source of increased risk because researchers believe stress increases the likelihood of developing Alzheimer’s disease as well as other dementias.
Why?
Chronic stress increases the production of plaque and tangles (abnormal buildup of a protein) in your brain, which is associated with Alzheimer’s disease, and damages healthy brain cells around these areas.
We all cope with stress differently, which adds to its complexity. Researchers are still examining the link to dementia, with much of the findings to date coming from animal studies.
However, there’s enough of a concerning link discovered already for women+, that if you tend to get stressed and overwhelmed, make this stage of life the time you make a big change! Practice self-care techniques, including stress management and coping skills you actually enjoy, and make the menopause journey a time to focus on optimizing your health and well-being. You’ll feel better overall, and your menopausal symptoms may also be less severe and frequent.
Stress and cardiovascular risk
Plain and simple. Stress is bad for your heart!
It increases inflammation in your body. A study linked the part of the brain impacted by stress to the subsequent development of cardiovascular disease.
So, stress at higher levels over an extended period of time, combined with the increased risk related to the hormonal transition of the menopause journey, means a compounding effect when it comes to poor heart health.
Talk to your healthcare practitioner. Those who maintain a lower stress level are 24% less likely to die from cardiovascular disease.
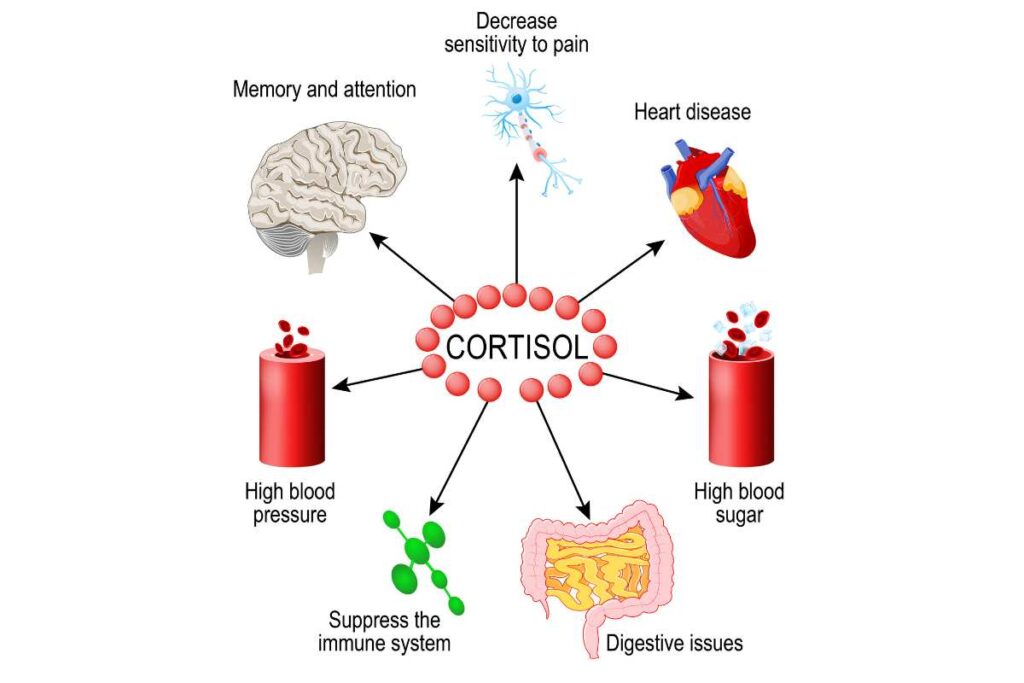
Your body’s response to stress
No matter who you are, stress can affect every part of your body – physically, mentally, and emotionally. We’ve only touched on a few menopausal risk factors, but there are many health conditions associated with stress.
To understand the widespread impact, it’s important to know what stress does to your body.
Your stress response is actually a hormonal response involving several different chemicals, in addition to cortisol. They include:
- epinephrine
- norepinephrine
- adrenaline
- cortisol
A stressor can trigger your “flight-or-fight response” (your sympathetic nervous system). When this happens, your brain releases several hormones, including epinephrine and norepinephrine. These increase your heart rate, blood pressure, and respiratory rate. They also activate your body’s immune response to help fight infection.
While this is happening, your brain releases a chemical messenger that ultimately leads to your adrenal glands releasing cortisol. That increases:
- Blood sugar for energy.
- Heart rate and breathing.
- Blood flow to muscles, but away from non-vital organs (like your gut).
Cortisol remains elevated for hours after a stressful event, continuing to promote alertness and focus.
It can also have an anti-inflammatory effect. This is important since your body’s initial release of norepinephrine and epinephrine triggers an immune response, causing inflammation.
Once your cortisol level begins to drop, your parasympathetic nervous system then helps your body heal and repair from the stressful event. This part of your nervous system is referred to as the “rest-and-digest” component.
It restores blood flow to non-vital organs, builds back your immunity, and replenishes your energy reserves.
Impact of chronic stress
For millennia, stress has been inevitable. It used to be animals that would activate the flight-or-fight response. Those encounters were short.
With modern day stressors, they can be long-term or chronic.
When the stressor doesn’t go away, your body repetitively activates your flight-or-fight response. Your cortisol levels repeatedly spike, eventually leading to cortisol dysfunction and a host of health issues, including burnout.
Signs and symptoms of high cortisol levels
The signs and symptoms of high cortisol levels can be seemingly unrelated, common, and hard to initially identify as related to stress. You may experience:
- fatigue, muscle aches and pain, sleeplessness, and headaches/migraines
- weight gain
- acne, thinning skin, and slowed healing
- Changes to your appetite and gut microbiome that can cause nausea, vomiting, indigestion, diarrhea, and constipation
When cortisol dysregulation happens, you’re:
- More likely to suffer from diabetes, obesity, and autoimmune disorders.
- Your risk of heart disease, especially if you’re post-menopausal, increases as well. This means you’re more likely to have narrowing of your arteries, which can lead to a heart attack, stroke, and high blood pressure.
- Additionally, stress can decrease your bone mineral density, putting you at risk for osteoporosis.
- And cortisol dysregulation can also worsen existing lung conditions, like asthma and COPD (chronic obstructive pulmonary disease – chronic bronchitis and emphysema).

Health disparities in stress during menopause
Stress has been increasing for everyone for the last 30 years, but the Black population as a group has higher stress levels, particularly when compared to their white counterparts.
Ultimately, this could cause faster biological aging, a phenomenon called “weathering,” often associated with a lifetime of inequity and systemic racism, from factors like housing, education, and employment to inadequate access to quality healthcare, from microaggressions to discrimination and hypervigilance related to sensationalized negative stereotypes and fear about physical safety when “living while Black.”
You already know chronic stress can lead to poorer health outcomes. For everyone, higher levels of stress contribute to faster cellular death, aging, and tissue degeneration, along with a multitude of other physical and mental health problems.
But high stress puts non-Hispanic Blacks at a much increased risk of premature death compared to non-Hispanic whites.
For example, consider the study which showed that experiencing recent stressful events is associated with a higher incidence of cardiovascular disease in older Black women. This can be particularly evident during the menopause transition.
And a disproportionately higher overall stress level could explain why this segment of the population has been found to age 6.1 years faster than whites.
Systemic causes of stress
Compared to whites, the stress Black people face is not necessarily directly connected to socioeconomic status in the manner one might expect at first glance.
In general, a higher socioeconomic status is associated with less stress. But Black individuals with a high socioeconomic status often have more stress than their white counterparts.
For those who experience a low socioeconomic status, stress levels have been found to be similar between Blacks and whites.
And overall, older Black people have higher stress levels than older whites, regardless of socioeconomic status. One reason could be they often need to work harder to sustain the same socioeconomic status in situations where systemic racism is alive and well, e.g., face more discrimination throughout their lives.
The stress of discrimination can lead to early menopause
Unfortunately, the stress experienced from discrimination could actually lead to an earlier age of onset of menopause and a more severe and symptomatic transition.
Black women+ tend to go through menopause almost a year earlier than white women+. And they’re 50% more likely to experience hot flashes, with hot flashes often being more severe and lasting for many years.
High blood pressure, depression, and sleeplessness are also more common in Black women+.
Hispanic women+/Latinas tend to have a similar experience with their menopause journey as Black women+ do, but to a lesser extent.
Racial differences seen during the menopause journey exist even when studies correct for other factors that may influence stress, including socioeconomic status and health behaviors, like diet, and exercise.
With other factors accounted for, more studies are concluding discrimination is indeed playing a major role in the health, well-being, and clinical outcomes of marginalized populations.
The power of hope
Despite all these additional challenges when it comes to stress, hope can go a long way to help mitigate its far-reaching, negative impacts. Just as a more neutral or positive attitude about the menopause journey can positively impact the severity and frequency of symptoms for many women+, hopefulness has been found to help decrease stress in Black people who experience discrimination.
So, find a way to believe you can obtain your goals and that your future can be bright despite all odds. Just knowing the years within the menopause journey during which symptoms are most prominent typically don’t last forever and that you have options – hormonal and non-hormonal – to both address them and prepare for a vibrant life ahead can provide a sense of control.
Preparing your personal action plan can be a great first step to decreasing your stress and improving your health, well-being, and menopause journey, both now and in the future.

Coping with stress
While workplaces and society have normalized severe and/or chronic stress and sometimes make it a badge of honor, it is not normal and not healthy. It can silently but negatively impact your life until it’s too late.
Pay attention to common symptoms of stress and:
- insomnia
- unrelenting fatigue
- uncharacteristic irritability or excessive worry
- changes to your appetite or gut microbiome (nausea, vomiting, indigestion, diarrhea, and constipation) thinning skin
- acne
- slow healing
Be honest with yourself and talk to your doctor about your stress levels and the ways they may impact you. Stress is just one factor that can elevate your cortisol levels. For example, certain medications, an overactive pituitary gland, and adrenal and pituitary tumors can also cause it.
Remember, many stress symptoms are also menopausal symptoms which can make it challenging to find the root cause(s) of your symptoms.
Self-medicating with alcohol, tobacco, or other unhealthy behaviors is not the answer and are likely to add to your problems, thereby increasing your stress even further.
There are other options, both hormonal and non-hormonal.
Techniques scientifically proven to make a difference that don’t involve hormones when it comes to stress include mindfulness, tapping (EFT), and having a gratitude practice, as well as living a healthy lifestyle – regular physical activity, getting enough high-quality sleep, and eating well.
Free Digital CBT (d-CBT)
Only available for a limited time!
Become a member of the pausitive health pilot program and get access to complimentary digital cognitive behavioral therapy (d-CBT) from our collaboration partner, SimpleTherapy. These sessions can relieve anxiety, stress, and depressive symptoms.
As a member, you’ll also get access to personalized text messages that focus on topics you select, virtual care, a supportive community, and more!
Can hormone therapy (HT) help your stress?
Studies examining hormone therapy (HT) and stress often come to vastly different conclusions. Because of this mixed picture of results, HT is not used as a primary treatment for stress.
But that doesn’t mean it might not help some women+ who may be taking it to address other symptoms like hot flashes, “brain fog,” and sleeplessness, especially depending on the formulation and delivery type of hormone therapy that is used.
Some studies show estrogen could reduce how active cortisol is in your body. This means even if you have a higher cortisol level, the effects are less.
Additionally, estradiol therapy could help blunt your body’s response to cortisol.
Women+ who took HT experienced fewer memory issues related to stress.
Yet, another study showed estrogen treatment in older women+ increased their negative mood when a stressful event occurred.
Having studies with differing results can be frustrating, as it’s difficult to know what to do.
However, each person’s menopause journey is unique. And just like other medications, the way one person responds, or not, and experiences side effects, or not, may be very different for someone else.
And then when you add factors like the various hormone formulations and dosages available, length of use, reason for use, underlying medical conditions, and menopausal symptoms, it’s not necessarily surprising to find different conclusions from different studies, especially if they are not looking at similar populations.
As always, consult with your healthcare practitioner to look at your entire picture to determine the next best step for you. And if you can find a practitioner in your area who has special training and expertise in menopause management, it might well be worth the search and travel.
You have options!
At the end of the day, your menopause journey is unique, and treatment, including HT, should be individualized to fit your particular situation.
A one-size-fits-all approach does not work well, so speak with your healthcare practitioner about your symptoms to see if HT alone, not at all, or in combination with other non-hormonal options could benefit you.
Consider all your options.
Developing/enhancing coping and self-care techniques, with a strong stress management focus, can make a big difference for you.
You can also try our Be Less Stressed Toolkit as an easy way to start to calm your mind.
Be Less Stressed
Feeling stressed or overwhelmed? Learn life hacks to reduce stress with the Be Less Stressed toolkit.
"*" indicates required fields
Life is too short to suffer when there are lots of options that can help, many of which are inexpensive or even free, are effective, and based in science.
If you don’t take stress seriously, your body often has a funny way of making sure you pay attention by stopping you in your tracks. Heart attack or off-the-rails anxiety, anyone?
Your stress and menopause symptoms are linked, each with the potential to make the other worse. Improving one could bring relief from the other. So, if you’re looking to have a happier menopause journey, try focusing on managing your stress.
Stress By Gender | American Psychological Association
Stress Effects on the Body | American Psychological Association
Stress Symptoms: Effects On Your Body and Behavior | Mayo Clinic
Plieger T, Melchers M, Montag C, Meergmann R, Reuter M. Life stress as potential risk factor for depression and burnout. Burnout Research. 2015, Volume 2, Issue 1, Pages 19-24. https://doi.org/10.1016/j.burn.2015.03.001
Arnot M, Emmott E, Mace R. The relationship between social support, stressful events, and menopause symptoms. PLoS One. 2021. https://doi.org/10.1371/journal.pone.0245444
Bansal R, Aggarwal N. Menopausal Hot Flashes: A Concise Review. J Midlife Health. 2019 Jan-Mar;10(1):6-13. doi: 10.4103/jmh.JMH_7_19. PMID: 31001050; PMCID: PMC6459071.
SWAN Fact Sheet: Hot Flash Fact Sheet | SWAN
Yale University. “Stress May Cause Excess Abdominal Fat In Otherwise Slender Women, Study Conducted At Yale Shows.” ScienceDaily. ScienceDaily, 23 November 2000. <www.sciencedaily.com
Alebna P and Maleki N (2021) Allostatic Load in Perimenopausal Women With Migraine. Front. Neurol. 12:649423. doi: 10.3389/fneur.2021.649423
Maleki N, Becerra L, Borsook D. Migraine: maladaptive brain responses to stress. Headache. 2012 Oct;52 Suppl 2(Suppl 2):102-6. doi: 10.1111/j.1526-4610.2012.02241.x. PMID: 23030541; PMCID: PMC3475609.
I’m So Stressed Out! Fact Sheet | National Institute of Mental Health
Saeedi M, Rashidy-Pour A. Association between chronic stress and Alzheimer’s disease: Therapeutic effects of Saffron. 2021. Biomedicine & Pharmacotherapy. Volume 133. https://doi.org/10.1016/j.biopha.2020.110995
Tawakol Ahmed, Ishai A, Takx R, Figueroa A, Ali Abdelrahman, Kaiser Y. Relation between resting amygdalar activity and cardiovascular events: a longitudinal and cohort study. The Lancet. 2017, Volume 389, Issue 10071, P834-845. DOI:https://doi.org/10.1016/S0140-6736(16)31714-7
Parker H, Abreu A, Sullivan M, Vadiveloo M. Allostatic Load and Mortality: A Systematic Review and Meta-Analysis. American Journal of Preventive Medicine. 2022. Volume 63, Issue 1, Pages 131-140. https://doi.org/10.1016/j.amepre.2022.02.003
‘Weathering’: What are the health effects of stress and discrimination? | Healthline Media
Guidi J, Lucente M, Soninho N, Fava G. Allostatic Load and Its Impact on Health: A Systematic Review. Psychotherapy and Psychosomatics. 2021;90:11-27. DOI: 10.1159/000510696
Howard, J.T., Sparks, P.J. The Effects of Allostatic Load on Racial/Ethnic Mortality Differences in the United States. Popul Res Policy Rev 35, 421–443 (2016). https://doi.org/10.1007/s11113-016-9382-4
Felix A, Lehman A, Nolan T, Sealy-Jefferson S, Breathett K, Hood D, Addison D, Anderson C, Cené C, Warren B, Jackson R, and Williams K. Stress, Resilience, and Cardiovascular Disease Risk Among Black Women. Circulation: Cardiovascular Quality and Outcomes. 2019; 12e005294. https://doi.org/10.1161/CIRCOUTCOMES.118.005284
Cortés Y, Marginean V. Key factors in menopause health disparities and inequities: Beyond race and ethnicity. Current Opinion in Endocrine and Metabolic Research. 2022, 100389. https://doi.org/10.1016/j.coemr.2022.100389
Forrester S, Jacobs D, Zmora R, Schreiner P, Roger V, Kiefe C. Racial differences in weathering and its associations with psychosocial stress: The CARDIA study. SSM – Population Health. 2019, 100319. https://doi.org/10.1016/j.ssmph.2018.11.003
Tobin C, Hargrove T. Race, Lifetime SES, and Allostatic Load Among Older Adults. The Journals of Gerontology: Series A, Volume 77, Issue 2, February 2022, Pages 347–356, https://doi.org/10.1093/gerona/glab160
25 years of research shows insidious effect of racism on Black women’s menopausal transition, health | University of Michigan
Discrimination May Hasten Menopause in Black and Hispanic Women| Scientific American
Mitchell, U. A., Dellor, E. D., Sharif, M. Z., Brown, L. L., Torres, J. M., & Nguyen, A. W. (2020). When Is Hope Enough? Hopefulness, Discrimination and Racial/Ethnic Disparities in Allostatic Load. Behavioral Medicine, 46(3–4), 189–201. https://doi.org/10.1080/08964289.2020.1729086
Ycaza Herrera A, Hodis H, Mack W, Mather M. Estradiol Therapy After Menopause Mitigates Effects of Stress on Cortisol and Working Memory. The Journal of Clinical Endocrinology & Metabolism, Volume 102, Issue 12, 1 December 2017, Pages 4457–4466, https://doi.org/10.1210/jc.2017-00825
Dumas JA, Albert KM, Naylor MR, Sites CK, Benkelfat C, Newhouse PA. The effects of age and estrogen on stress responsivity in older women. Am J Geriatr Psychiatry. 2012 Sep;20(9):734-43. doi: 10.1097/JGP.0b013e31825c0a14. PMID: 22832417; PMCID: PMC3428432.
Find a Menopause Practitioner | The Menopause Society

17 Menopausal Anxiety Treatment Options To Ease Your Mind
Feeling anxious during the menopause journey? Try these 16 anxiety treatment options to ease your mind of worry and fear.

Feeling Anxious? How Anxiety Impacts Menopausal Symptoms and Vice Versa
Are you feeling more anxious during the menopause journey? You are not alone. Learn how it can impact other menopause symptoms too.

What Is Anxiety, and Why Does It Impact More Women+ Than Men?
Are you experiencing anxiety during the menopausal transition for the first time? Learn about the types of anxiety and why it impacts more women.

