Cognitive behavioral therapy (CBT) doesn’t exactly roll off your tongue, but it should if you’re going through the menopause transition. Perhaps that’s the name you need to focus on saying ten times in the middle of the night to lull yourself back to sleep. Forget the alphabet or counting sheep! CBT is a powerful and transformative technique that can help you sleep better and reduce bothersome perimenopausal symptoms like hot flashes. CBT techniques can also be helpful for other issues unrelated to your menopause journey.
What is cognitive behavioral therapy (CBT)?
Cognitive behavioral therapy (CBT) is a form of psychotherapy that helps you examine and reframe your thoughts, feeling, and behaviors.
This technique is a drug-free way to treat perimenopausal symptoms like low mood, hot flashes, night sweats, stress, and sleep issues, including insomnia. (The Sleep Foundation indicates a diagnosis of insomnia “requires sleep troubles to cause daytime impairments, such as sleepiness or difficulty concentrating.”)
Cognitive behavioral therapy for insomnia (CBT-I) is a technique recommended by The American College of Physicians to be used as an initial treatment as it’s been found to be more effective than medications.
CBT-I appears to be safe to use long-term, unlike sleeping pills.
It also addresses some underlying issues that might prevent you from getting enough sleep, like depression or anxiety.
Finally, with CBT you can learn how to eventually implement the techniques on your own as needed, whether that’s in the middle of the night or a stressful situation.
So, if you’ve tried all the other sleep hygiene techniques and still can’t sleep – cognitive behavioral therapy may be one to explore.
How does CBT work?
CBT works to change your thinking and behavioral patterns. It is typically delivered in concert with a therapist.
You’ll explore what’s holding you back from getting enough sleep. Is it your daily routine, a previous experience, an unrealistic expectation, stress, or anxiety?
The treatment plan may help you change your thinking patterns so you can:
-
- Utilize problem-solving skills when life gets complicated.
- Recognize one’s distortions in thinking that lead to problems and re-evaluate them in a new light.
- Gain a better understanding of the behavior and motivation of others.
- Develop a greater sense of confidence in your abilities.
CBT may help you change behavioral patterns so you can:
-
- Face your fears rather than avoid them.
- Use role-play to prepare for future issues.
- Learn to calm your mind and relax your body.

Establishing positive affirmations
CBT also works on restructuring thoughts. It may be challenging to flip a negative thought into a positive one in the heat of the moment (pun intended), such as a hot flash, sleepless night, or everyday conflict. So, think about ways you can redirect your thoughts ahead of time.
Create positive affirmations by reflecting on how you commonly feel during a hot flash or a middle-of-the-night awakening. Write down your thoughts. Are they as positive as they realistically could be?
According to a study by King’s College London, most thoughts fall into one of three negative categories:
- Social context.
Example: “These hot flashes are embarrassing and shameful.” - Lack of perceived control over hot flashes.
Example: “They will never end. I can’t cope.” - Worry over the ripple effect.
Example: “If I wake up, I’ll never fall back asleep.”
Example: “If I have night sweats, I’ll feel awful the next day.”
You can change the negative thoughts with positive affirmations.
In a clinical setting, you may also learn about symptom perception and self-regulation techniques.
Write down your affirmations and keep them near your bed, so you can repeat them when you’re experiencing sleeplessness.
Put them in the notes on your phone so that you can reflect on them during a hot flash at work.
Tell yourself you can do it!
Examples of positive affirmations
- I will make it through the day tomorrow. I’ve done it before and will do it again.
- I will prioritize my day and overcome this.
- The menopause journey is a time of awakening and contemplation of what the future holds for you. I will come out of this stronger.
- This too shall pass, with time.
- I can only control what I can control.
- I am awake, but I can fall back asleep.
You can apply these strategies and mental frameworks during the day when a hot flash comes on during a business meeting and at night when you can’t sleep.

CBT strategies for hot flashes and night sweats
Let’s go through a few examples of how a woman+ can use CBT to reduce symptoms like hot flashes, night sweats, and even cold flashes.
When using CBT for hot flashes, you focus on changing the way you think about them. In turn, those reframed thoughts can reduce the intensity of the hot flashes.
Think about it for a second. When you feel a hot flash coming on, what goes through your mind?
Does it make you nervous? Stress you out? Make you want to run out of the room, especially if you’re at work? Do you get frustrated by yet another hot flash at an inopportune time?
Those negative and judgmental thoughts can make your face more flushed and make you sweat even more.
Instead, change your mindset.
Reassure yourself. Tell yourself you will make it through this hot flash just like the one before it.
Accept it for what it is – a moment in your life that you can control and that won’t last forever.

CBT for Insomnia (CBT-I)
Hot flashes, night sweats, leg pain, and RLS are just some of the things that can keep you up at night. Sometimes that can lead to insomnia.
One in four women have insomnia symptoms, like having trouble falling asleep, staying asleep, or both.
CBT for insomnia (CBT-I) focuses on techniques like sleep compression, sleep restriction, stimulus control, and relaxation techniques like paced breathing.
Sleep restriction helps with sleeplessness or awakenings in the middle of the night by restricting how long you are awake in bed.
If you’re trying to get eight hours of sleep a night but only get five, then adjust your bedtime so you only spend five hours in bed at night. That way, you don’t lie awake as long. As your sleep improves, you increase your time in bed.
Sleep compression follows the same concept, but the time in bed is slowly adjusted rather than abruptly. Over time, you work toward the goal of the recommended 7 – 9 hours spent asleep in bed.
With stimulus control, you only use your bedroom for sleep and sex. Don’t watch TV, check your phone, work out, or read in bed.
You can also set the mood for sleep with techniques like binaural beats. This sleep hygiene hack tunes your brain for better sleep with brain wave music.
Finally, relax. Don’t worry about not falling back asleep. That’s only going to make it harder to do just that.
Take slow, deep breaths. Paced breathing taps into the power of your brain with your breath. You can use it to take control of sleeplessness or during the day when you have a hot or cold flash.
It can reduce feelings of anxiety, anger, and depression by slowing your heart rate and breathing.
Paced breathing is a rhythmic way of breathing from your stomach slowly and deliberately while accepting the hot flash or sleepless night, knowing you can breathe through it, and it will pass.
This technique should be practiced throughout the day, so you’re prepared when you need it at night.
Restless leg syndrome is also a common menopause symptom that disrupts sleep due to the uncontrollable urge to move your legs. It’s more common in women than men. CBT for insomnia has also been shown to help RLS patients. What are your thoughts when your legs are moving uncontrollably at night and you’re awake rather than asleep? Are you telling yourself you’re never going to go back to sleep due to the movement? Are you obsessing over the movement? Shift your mindset from the leg pain or movement to positive thoughts like that you will fall asleep, and will make it through tomorrow.
CBT apps
You can seek the help of a trained CBT therapist or go the self-help route.
The app, CBT-I Coach, developed by the U.S. Department of Veterans Affairs, can guide you through CBT techniques.
It was developed by the VA’s National Center for PTSD in partnership with clinical and government agencies. The app can be used on its own, but it’s not intended to replace clinical care for those who need it. The app provides information about CBT-I and how it works, a sleep diary, tips to develop positive sleep habits, and tools to relax when going to sleep or trying to fall back asleep in the middle of the night.
If you have insomnia and are not working with a therapist to learn CBT-I, the VA recommends Insomnia Coach. It’s for everyone, including veterans. It’s a free, self-help app to help you develop better sleep habits.
The VA has an educational course to guide you along the “Path to Better Sleep.” You learn about quieting your mind, challenging your thoughts, stimulus control, and creating a sleep schedule. Start your learning journey.
CBT self-help
Self-help can work. A small British study by researchers at King’s College London of 124 working postmenopausal women who experienced at least ten hot flashes or night sweats per week provided women+ with a self-help CBT booklet and a breathing/relaxation CD.
Hot flashes and night sweats decreased on average by 24% in six weeks and 35% after 20 weeks. The women also saw significant improvements in sleep quality.
Researchers noted the dropout rate was unexpectedly high, as is often the case when we try to change well-established behavior patterns and ways of thinking. Change takes time and commitment. The study found participants viewed menopause as more “controllable and curable.”
Participants also said they were more confident and open to discussing their menopause journey, even at work.
So, consider CBT-I Coach or one of the other self-help approaches as a potential option for managing and controlling your night sweats and sleepless nights.
Finding CBT support
If self-help doesn’t work or you’d rather consult an expert for a more effective solution, search for a therapist through the Academy of Cognitive and Behavioral Therapies database. A treatment plan can be developed in as few as 4 or 5 sessions, according to the Society of Behavioral Sleep Medicine. Providers may have different approaches tailored to the needs of the individual.
While CBT won’t eliminate hot flashes, it’s a technique that allows you to gain a sense of control over them so they don’t control you!
Armed with day and night mind-body sleep strategies and good sleep hygiene, you have the power to help get the sleep you need and survive your next hot flash.
Free Support
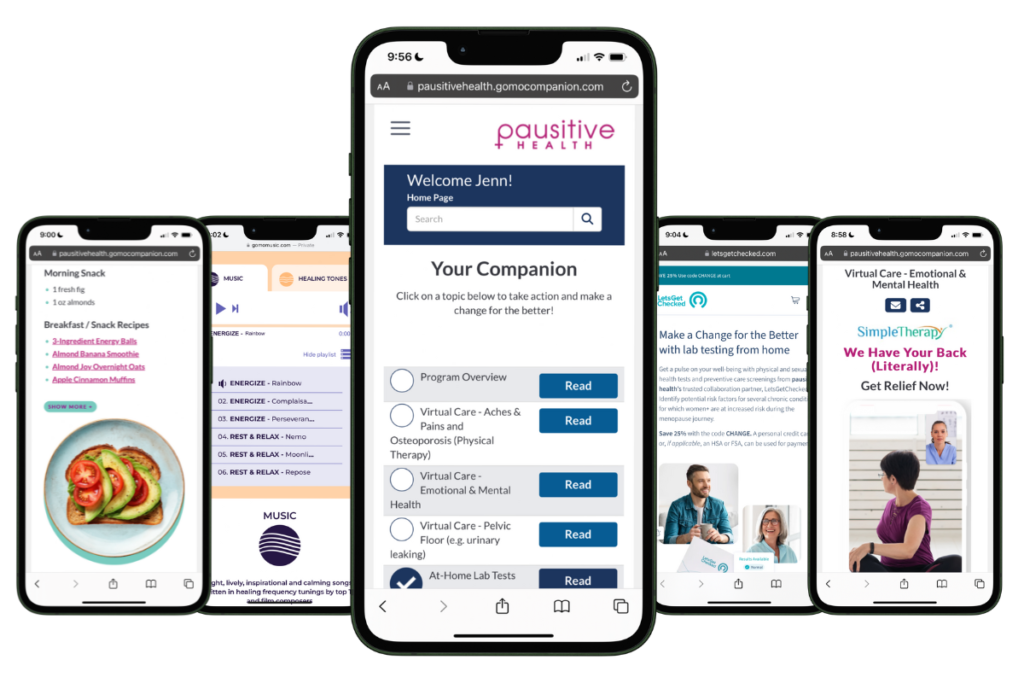
For Your Menopause Journey!
Only available for a limited time!
Access a one-stop menopause journey digital destination that provides personalized text messages that focus on educational topics you select and offers many other features such as a diet assessment with recommendations, solutions from collaboration partners to address menopausal aches and pains (the musculoskeletal syndrome of menopause – MSM), pelvic floor issues, virtual care, lifestyle tools, and a supportive community.
Insomnia | Sleep Foundation
ACP Recommends Cognitive Behavioral Therapy as Initial Treatment for Chronic Insomnia | American College of Physicians®
What is Cognitive Behavioral Therapy? | American Psychological Association
Song ML, Park KM, Motamedi GK, Cho YW. Cognitive behavioral therapy for insomnia in restless legs syndrome patients. Sleep Med. 2020 Oct;74:227-234. doi: 10.1016/j.sleep.2020.07.011. Epub 2020 Jul 19. PMID: 32861015.
Insomnia | Office on Women’s Health at the U.S. Department of Health and Human Services
CBT-I Coach from the U.S. Department of Veterans Affairs | Apple Store
PTSD: National Center for PTSD VA Mobile Apps | U.S. Department of Veterans Affairs
Hardy, C., Griffiths, A., Norton, S., & Hunter, M. S. (2018). Self-help cognitive behaviour therapy for working women with problematic hot flushes and night sweats (MENOS@Work): a multicentre randomised controlled trial. Menopause: The Journal of The Menopause Society, 508-519.
https://doi.org/10.1097/GME.0000000000001048
Find a CBT Therapist | Academy of Cognitive and Behavioral Therapies
Adult Insomnia | Society of Behavioral Sleep Medicine
Hunter, M. S., & Chilcot, J. (2021). Is cognitive behaviour therapy an effective option for women who have troublesome menopausal symptoms? British Journal of Health Psychology, 26(3), 697-708.
https://doi.org/10.1111/bjhp.12543
You may also like...

Hormone-Free Hot Flash Relief: 12 Non-Hormonal Medications To Try
Want to beat the heat from hot flashes hormone-free? Try these non-hormonal hot flash medications that are FDA-approved or used off-label.

Black Women and Menopause: Why Symptoms Can Be Longer and More Severe
As a Black woman, menopause symptoms, including hot flashes, can be longer and more severe. Learn why and what you can do.

Which Herbal Remedies Offer Relief From Hot Flashes And Other Menopause Symptoms?
Can herbal remedies help menopause symptoms like hot flashes? Get the latest science, risks, and reported health benefits.