All women should be on alert for depressive symptoms, as it’s more prevalent among women than men. Plus, there’s an increased risk during the perimenopuase stage of the journey. There are other factors, too, including socioeconomic and lifestyle factors. Understanding if you’re at increased risk for depression during the menopausal transition can help you get treatment sooner so you can improve your overall well-being.
Depression and perimenopause
Depression is common during perimenopause. Depressive symptoms impact 45-68% of women, according to The Menopause Society. The risk typically decreases as you transition through menopause.
There’s nothing to be ashamed of if you’re depressed.
It is a condition that should not be viewed differently than if you had a medical condition like heart disease.
Although significant progress has been made, it is still all too common that society views mental health conditions differently than physical ones. And given the two are inextricably intertwined, trying to separate one from the other is even more counterproductive.
For example, if you are suffering from depression when you have a heart attack, it is more likely you will have a second heart attack than someone who was not depressed at the time. Additionally, depression often follows a heart attack and may negatively impact motivation for engaging in cardiac rehab.
Depression signs during menopause
Depression typically manifests as persistent sadness, withdrawal from activities you once enjoyed, difficulty sleeping, and slowing down. In some people, it may be manifest in irritability, anxiety, anger, or even rage.
It gets complicated during menopause because the traditional notion of “feeling blue” is not necessarily the most common symptom.
According to the Study of Women Across the Nation (SWAN) data, the most common signs of depression during menopause are nervousness, irritability, and mood swings.
It’s common for these symptoms to accompany other frequent menopausal symptoms like difficulty sleeping, night sweats, and hot flashes.
Understand your risk factors, track your symptoms, and talk to your doctor.

Depression risks
Below are some of the common risk factors for depression during the menopause transition:
1. History of depression
A history of depression is one of the strongest predictors of menopausal depression. Women who’ve had the condition in the past are up to 5 times more likely to have a diagnosis of major depressive disorder (MDD) during this time of life. Symptoms may reoccur early in the transition during the perimenopause stage of the journey, as well as later in the transition.
Watch for warning signs, and seek treatment if it reoccurs.
A history of depression increases your chance of earlier perimenopause.
Be sure to contact your healthcare provider both to make sure your symptoms don’t have another cause as well as to get started on a treatment regimen that is a fit for your situation as soon as possible.
2. Hormones
If you’re feeling depressed, you’ve probably blamed your hormones. It’s perhaps the least surprising risk factor.
Changes in estradiol and progesterone levels contribute to perimenopausal depressive symptoms.
Different studies characterize the risk differently, but most studies have shown you double your risk of depression during the menopause transition.
The European Menopause and Andropause Society (EMAS) found in an eight-year study that a depression diagnosis was 2.5 times more likely to occur in the menopausal transition than during the pre-menopausal stage of life. The risk goes down after menopause, but it still exists, particularly given the increased risk of chronic conditions as hormones reach menopausal levels or as one gets older.
3. PMS
Both PMS and menopause are related to hormonal changes in the brain, thus increasing your chance of depression.
Is your history of depression linked to premenstrual syndrome or PMS? It’s a common combination.
Even if your physical, emotional, and behavioral PMS symptoms did not rise to the level of depression during your menstrual cycle, just having PMS may increase your chances of depression during menopause.
4. Menopausal status
You’re at risk for depression throughout the menopausal transition, but perhaps more so during perimenopause. That risk is present even if you have no history of depression.
And premature menopause (onset of menopause at an age younger than 40) is a risk factor for depression during the menopause transition.
5. Age when you hit menopause
Menopause typically hits between the ages of 45 and 55. But, it can come early or later.
Premature menopause has been shown to increase your risk for depression, whether natural, due to chemo, radiation, hysterectomy, or ovarian insufficiency.
The older you are when you hit menopause, the lower your risk for depression.
The risk of severe depression goes down as you age because your reproductive years and premenopausal level of hormones last longer.
50% decreased risk of depression
6. Hysterectomy
There are conflicting thoughts, as research is still ongoing into the causes of menopausal symptoms and the impact on women. Historical data conflicts on whether hysterectomy increases or decreases the risk of depression.
However, recent studies indicate a link between hysterectomy and mental health issues.
Even if your ovaries are not removed during a hysterectomy, the increased risk of mental health problems can last up to 30 years.
Mayo Clinic researchers found hysterectomy in women whose ovaries were preserved at the time of removal of the uterus was still associated with an increased risk of long-term mental health issues, especially depression and anxiety.
They observed that over a 30 year period, the overall risk increased 6.6% for depression. The risk increased to 12% for women who had a hysterectomy between the ages of 18 and 35.
7. Convergence of life changes and the toll of stress
In addition to the biological changes that can cause depression, the psychological and physical toll of menopause can contribute to having depression.
Menopause can be a life-altering time, and you may experience mental, physical, and emotional problems for the first time.
Plus, you’re likely experiencing other life changes. Children may be leaving the house, you may be caring for a family member, experiencing changes to marital status, or maybe thinking about retirement. All these changes add up and can result in a major disruption in the life you have been leading.
Studies have found changes to your body, sexuality, fitness, social and gender roles, relationships, family structure, and professional position are additional stressors that can increase feelings of overwhelm, lost self-esteem, and lack of motivation and contribute to depression.
8. Socioeconomic status (SES)
In addition to lifestyle factors, socioeconomic status may also put you at higher risk.
According to SWAN data, racial and ethnic disparities in depressive symptoms are primarily related to low socioeconomic status (SES), which in turn can result in financial stressors, physical inactivity, low social support, stress, and poor physical health. Health-related factors may also be contributory.
The study found Hispanic and African American women had the highest odds of depression and the highest percentage of women with low SES. Hispanic women were more at risk, with the average woman experiencing a 1.74-fold increased odds. And when low SES were present the increased risk was 2.45 times higher for Hispanic women.
Chinese and Japanese women had the lowest odds of depression and the fewest percentage of women with low SES.
Researchers also point to additional issues, including unemployment and being unmarried or single with no partner as risk factors.
9. Menopausal symptoms
Symptoms also play a role in your risk for depression, specifically hot flashes, night sweats, and sleep disturbances.
While there’s controversy regarding the link between hot flashes and depressive symptoms, the association between hot flashes and sleep, and the association between sleep disturbance and depressive symptoms makes hot flashes concerning.
Moderate-severe VSMs are significantly associated with moderate-severe depressive symptoms, regardless of the controversy.
10. Sleep issues
There is a strong connection between sleep issues and depression.
One sign of depression can be sleep issues. It can take the form of having problems getting sleep in some people and sleeping too much in others or going back and forth between the two.
And having chronic insomnia can increase the risk of depression.
Studies indicate up to 80% of patients with depression experience insomnia, and approximately 40% of people with insomnia have clinical depression.
During the menopause journey, associated symptoms like hot flashes, night sweats, palpitations, and aches and pains can make getting enough good quality sleep challenging. In turn, that challenge can increase the risk of as well as exacerbate depression.
11. Your overall health
A healthy lifestyle becomes even more critical as you age, and in addition to helping you manage menopause symptoms, it can help you live longer, and minimize the risk of health conditions.
When your health goes downhill, there can be a downward spiral.
Having a chronic medical condition can increase the risk for depression. And if you suffer a severe medical event, like a stroke or heart attack, your risk increases even more. In fact, those who are depressed at the time of a heart attack are more likely to suffer a second one compared to patients without preexisting depression.
In addition, other risk factors can include being overweight/obese or smoking.
Remember, eating the right foods, exercising, and getting enough sleep are keys to success throughout your life.
Get depression help early
If you suspect you’re depressed, no matter how significant or minor your symptoms may be, make it a priority to get the advice of a doctor.
If your depression diagnosis is made during the menopause transition, know the symptoms may be temporary, can be managed, and typically improve as you transition through menopause.
Call 9-8-8
Even though they may be temporary, please don’t ignore them. With early treatment, you may be able to help prevent the problem from becoming more serious. Remember, the lifetime risk of suicide in those with untreated depression is 20%. And if you have suicidal thoughts, don’t hesitate to dial 988, the phone number for the National Suicide & Crisis Lifeline. If you are actively suicidal, call 911 and seek care immediately.
You are not alone in how you feel. Depression is common and is one of the most treatable mental health conditions, with 80-90% of people eventually responding well to treatment.
Don’t suffer in silence.
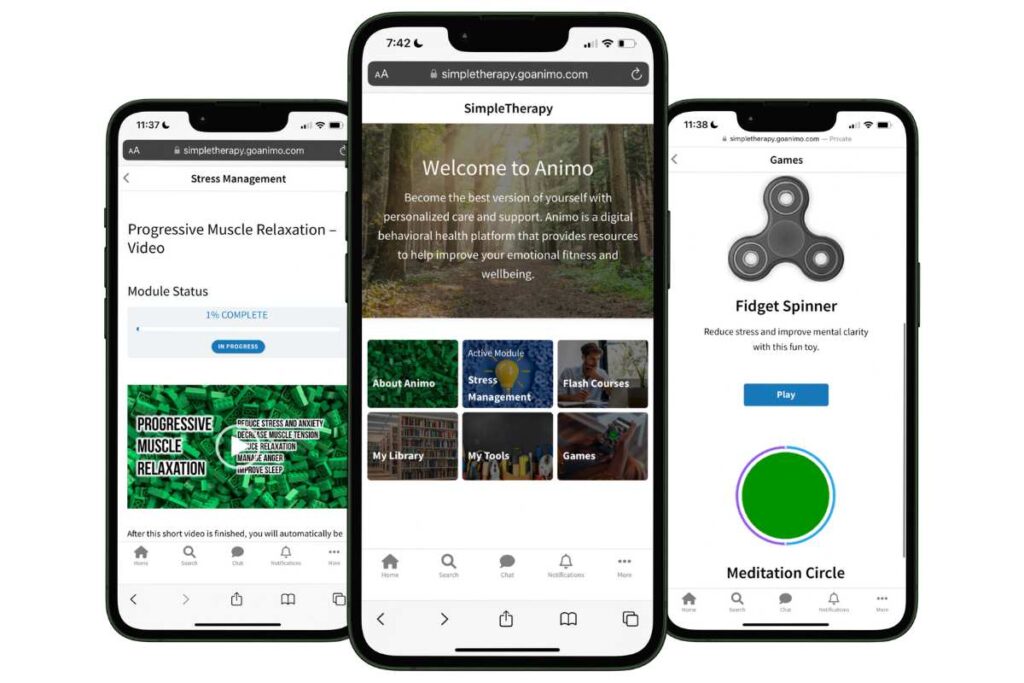
Free Digital CBT (d-CBT)
Only available for a limited time!
Become a member of the pausitive health pilot program and get access to complimentary digital cognitive behavioral therapy (d-CBT) from our collaboration partner, SimpleTherapy. These sessions can relieve anxiety, stress, and depressive symptoms.
As a member, you’ll also get access to personalized text messages that focus on topics you select, virtual care, a supportive community, and more!
Guidelines for the evaluation and treatment of perimenopausal depression: summary and recommendations | The Journal of The Menopause Society
Diagnosis and management of mood disorders during the menopausal transition | The American Journal of Medicine
Freeman EW, Sammel MD, Lin H, Nelson DB. Associations of Hormones and Menopausal Status With Depressed Mood in Women With No History of Depression. Arch Gen Psychiatry. 2006;63(4):375–382. doi:10.1001/archpsyc.63.4.375
Management of depressive symptoms in peri- and postmenopausal women: EMAS position statement | European Menopause and Andropause Society
Hadine Joffe, MD, on Depression in Perimenopause | MedPage Today
Georgakis MK, Thomopoulos TP, Diamantaras AA, Kalogirou EI, Skalkidou A, Daskalopoulou SS, Petridou ET. Association of Age at Menopause and Duration of Reproductive Period With Depression After Menopause: A Systematic Review and Meta-analysis. JAMA Psychiatry. 2016 Feb;73(2):139-49. doi: 10.1001/jamapsychiatry.2015.2653. PMID: 26747373.
Clayton AH, Ninan PT. Depression or menopause? Presentation and management of major depressive disorder in perimenopausal and postmenopausal women. Prim Care Companion J Clin Psychiatry. 2010;12(1):PCC.08r00747. doi: 10.4088/PCC.08r00747blu. PMID: 20582297; PMCID: PMC2882813.
Harlow BL, Wise LA, Otto MW, Soares CN, Cohen LS. Depression and its influence on reproductive endocrine and menstrual cycle markers associated with perimenopause: the Harvard Study of Moods and Cycles. Arch Gen Psychiatry. 2003 Jan;60(1):29-36. doi: 10.1001/archpsyc.60.1.29. PMID: 12511170.
Depression in Parents, Parenting, and Children: Opportunities to Improve Identification, Treatment and Prevention | National Academies Press
You may also like…

Yes! You Really Can Be Grateful During the Menopause Journey – Here’s How
Gratitude during menopause? It may seem counterintuitive, but being grateful can help your symptoms and improve your outlook.

Why Anger Problems Are Bad For Your Health
Anger is yet another menopause symptom, but anger problems are bad for your health, leading to depression and other health concerns.
Why Am I So Forgetful? Could It Be Dementia Or Is It Menopause?
Are you feeling forgetful or having trouble concentrating? Learn the difference between brain fog and dementia, and how to help prevent dementia.

