How often do you feel those sudden waves of intense heat wash over your face, neck, and chest, leaving you flushed, sweating, and reaching for the nearest fan? Hot flashes are one of the most common and disruptive symptoms of the menopause journey, affecting up to 80% of women during this transition. While they can feel isolating and even embarrassing, understanding what’s happening in your body and knowing your options can make all the difference.
Hot flash 101
Women describe hot flashes as a burning or overheated sensation, most commonly felt in the head, neck, chest, and upper back. Some women+ experience "cold flashes" as well, which may follow a hot flash as your body overcorrects. These episodes can last anywhere from a few seconds to several minutes and can occur multiple times throughout the day and night.
You may hear hot flashes interchangeably called vasomotor symptoms or VMS. That's because the medical term "vasomotor" refers to the expansion and constriction of blood vessels, essentially, your body's thermostat changing in response to hormonal changes impacting the brain.
VMS refers to several related symptoms, including:
- hot flashes
- night sweats
- heart palpitations
They may occur independently or together.
And in the aftermath of a hot flash, some women actually experience cold flashes.
During the menopause transition, your ovaries gradually produce less estrogen and progesterone. This isn't a smooth decline. Instead, hormone levels fluctuate wildly, creating volatility that throws off the delicate balance your body has maintained for years.
Your brain's temperature control center, which relies on stable estrogen levels to function properly, gets confused by these rapid changes. The result? Your body thinks it's overheating when it's not, triggering the cascade of symptoms you experience as hot flashes, night sweats, and/or palpitations.
There are hormone-free breakthrough medical treatments available for women+ who want a non-hormonal way to manage hot flashes or vasomotor symptoms.
There are three FDA-approved medications, hormone therapy, herbal remedies, and lifestyle changes. Women have more options than ever before to manage hot flashes.
Don't suffer through them. Studies show women+ who have severe or frequent hot flashes face increased health risks. Take control of menopause, and make this a time you make a change for the better.

The Real impact: more than just discomfort
While hot flashes might seem like a temporary inconvenience, their effects ripple through every aspect of daily life.
Daytime hot flashes can interrupt work meetings, exercise routines, social gatherings, and intimate moments with your partner.
Night sweats disrupt sleep, leading to chronic fatigue, difficulty concentrating, and mood changes.
Health risks
Beyond quality-of-life concerns, research shows that women+ who experience severe or frequent hot flashes, or those whose symptoms persist for many years, face increased health risks.
These health risks include:
- higher rates of heart disease
- lower bone density that can lead to osteoporosis and fractures
- potentially an elevated risk of cognitive decline and dementia.
This is why addressing hot flashes isn’t just about comfort; it’s about protecting your long-term health.
Health Inequities: who’s most affected?
The burden of hot flashes doesn’t fall equally on all women. Research consistently shows significant disparities based on race and ethnicity.
Black and Hispanic/Latina women are more likely to experience hot flashes during the menopause journey, and their symptoms tend to last longer and be more severe than those experienced by white women.
Native women report more hot flashes during perimenopause than any other racial or ethnic group and are also more likely to report them when they are premenopause as well.
Other risk factors that can intensify hot flashes include smoking, obesity, and genetic predisposition.
Understanding your personal risk factors can help you and your healthcare practitioner develop a more targeted approach to managing your symptoms and a comprehensive review of your options.
Lifestyle changes that help
The good news is you have more control over hot flashes than you might think. While you can’t stop the hormonal changes of menopause, you can significantly reduce the frequency and severity of hot flashes through targeted lifestyle adjustments.
Dress strategically
Start your day with layers. When a hot flash hits, you can peel off a cardigan or jacket instead of being stuck in a sweater that feels suffocating. Natural, breathable fabrics like cotton and linen work better than synthetic materials. Some women+ also find cooling scarves or moisture-wicking fabrics helpful for managing sudden temperature spikes.
Identify and avoid your triggers
Certain foods and beverages are notorious hot flash triggers. The most common culprits include:
Spicy foods
That rush of heat you feel after eating spicy dishes can trigger or intensify hot flashes.
Caffeine
Found in coffee, tea, and some sodas, caffeine can bring on vasomotor symptoms.
Alcohol
Even one drink can cause facial flushing and trigger hot flashes. Research also shows a concerning link between alcohol consumption and breast cancer risk (with some studies indicating that any alcohol consumption is bad for health and well-being).
Hot beverages and soups
The heat itself can trigger your body’s cooling response.
Processed and fast food
These can contribute to inflammation and weight gain, both of which may worsen symptoms. To make matters worse, there appears to be a potential association between ultraprocessed foods and the type of polyps that can turn into cancer. Additionally, the impact seems to be greater at younger ages.
Foods high in saturated fats
These foods have been associated with more frequent hot flashes, which are also more severe.
Pay attention to your body’s signals. If you notice certain foods consistently trigger hot flashes, it’s worth cutting back or eliminating them. Keep a symptom diary to track potential triggers. You might be surprised by the patterns you discover.
Maintain a healthy weight
Research shows that women+ who are overweight or obese tend to experience more frequent and severe hot flashes. Regular physical activity not only helps with weight management but also improves sleep quality, boosts mood, and supports cardiovascular health.
You don’t need to run marathons. Moderate exercise like brisk walking, swimming, or cycling for 30 minutes most days of the week can make a meaningful difference. And strength training is essential to help prevent osteoporosis and muscle mass. Muscle also positively impacts metabolism.
Breakthrough medical treatments: more options than ever
The landscape of hot flash treatment has transformed dramatically in recent years, offering women more choices than ever before. Whether you prefer hormonal or non-hormonal approaches, there are evidence-based options that can provide significant relief.
Major update: FDA removes black box warnings from hormone therapy
In a groundbreaking development, the FDA recently removed black box warnings from hormone therapy labels, recognizing that previous warnings didn’t reflect the nuanced science around timing and individual risk factors. This change represents a significant shift in how we understand hormone therapy and how it’s prescribed.
Research now clearly shows that hormone therapy initiated within 10 years of menopause onset—or before age 60—has been associated with numerous health benefits without significantly affecting cardiovascular disease risk in younger postmenopausal women. The benefits include:
- a dramatic reduction in hot flashes and night sweats
- a reduction in fatal cardiovascular events (the leading cause of death in women+)
- a reduction in bone fractures
- a potential reduction in cognitive decline and risk of Alzheimer’s disease (conflicting studies so more research needed)
The key is timing. When hormone therapy is started during this “window of opportunity,” it can be one of the most effective ways to improve long-term health outcomes for women+ on a population level. The old “one-size-fits-all” approach has been replaced with personalized recommendations based on your age, time since menopause, and individual health profile.
Hormone therapy now comes in many different formulations—pills, patches, gels, and creams—each with its own benefit-risk profile.
The recommendation to use “the lowest effective dose for the shortest duration” has also been removed, acknowledging that treatment decisions should be individualized based on your particular situation and ongoing discussion with your healthcare provider.
Non-hormonal prescription medications: three FDA-approved options
If hormone therapy isn’t right for you—or if you simply prefer a non-hormonal approach—there are currently have three FDA-approved medications specifically designed to treat moderate to severe hot flashes:
Paroxetine (Brisdelle®)
This low-dose SSRI antidepressant was the first non-hormonal medication approved for hot flashes. It works by affecting brain chemistry to reduce the frequency and severity of vasomotor symptoms.
Fezolinetant (Veozah®)
Approved in 2023, this breakthrough medication represents a completely new class of drugs called neurokinin 3 (NK3) receptor antagonists. It targets the brain area responsible for temperature regulation, addressing hot flashes at their source.
In clinical trials, women taking Veozah experienced a 60% reduction in hot flashes after 12 weeks (compared to 45% with placebo). The medication requires baseline bloodwork and regular monitoring during the first several months due to a rare but serious risk of liver injury. However, for many women+, this monitoring is a worthwhile trade-off for the significant symptom relief Veozah can provide.
Elinzanetant (Lynkuet®)
The newest addition to the hot flash treatment arsenal, Lynkuet, is also a hormone-free prescription option.
In clinical trials involving 796 menopausal women experiencing moderate to severe hot flashes, participants saw impressive results. At week 12, women taking Lynkuet had 8.7 to 9.7 fewer hot flashes per day compared to 5.4 to 6.5 fewer with placebo. Some women even noticed improvement as early as one week.
Further investigation is underway to determine if it also independently improves sleep.
Off-label medications
Other medications are sometimes prescribed off-label for hot flashes, including:
- certain antidepressants (SSRIs and SNRIs),
- anti-seizure medications like gabapentin
- blood pressure medication clonidine
- other antidepressants (SSRIs and SNRIs – citalopram (Celexa), Sertraline (Zoloft), escitalopram (Lexapro), fluoxetine (Prozac), paroxetine (Paxil), duloxetine (Cymbalta), venlafaxine HCI (EFFEXOR XR®), and desvenlafaxine (Pristiq)

Herbal remedies and alternative approaches
Many women explore herbal remedies as alternatives or complements to conventional treatments. While research on these approaches is mixed, some show promise:
Black cohosh
One of the most commonly used botanicals for the menopause journey, black cohosh has shown benefits in some studies, though results are inconsistent. Some research suggests it may help with hot flashes, vaginal dryness, and sleep disturbances. The typical dose is 40 mg/day. Note that rare cases of liver damage have been reported, so, as always, discuss this option with your healthcare provider.
Red clover
Contains isoflavones that are structurally similar to estrogen. Some studies show improvements in hot flash frequency and intensity, as well as benefits for bone density, though evidence remains mixed.
Sage
One clinical trial found that women taking a daily sage tablet experienced a 64% decrease in hot flashes after eight weeks, with the most dramatic improvements seen in severe and very severe hot flashes.
Hops
Beyond its use in beer, hops extract may help with hot flashes and sleep quality. Research suggests it could be an effective alternative for women+ seeking relief from vasomotor symptoms.
Other options
St. John’s Wort (particularly when combined with black cohosh), valerian root for sleep and hot flashes, and ginseng for sexual function and overall menopausal symptoms have all shown benefits in various studies.
Important caveat
Herbal remedies are not without risks. They can interact with prescription medications, cause side effects, and may not be safe depending on your health conditions. Always consult with your healthcare provider or a certified herbalist before starting any herbal supplement. The Australian Menopause Society and other international organizations provide helpful guidance on the safety and efficacy of various herbal approaches.
Cognitive Behavioral Therapy: training your brain
Cognitive behavioral therapy (CBT) is an evidence-based psychological approach that can help you manage not just the physical symptoms of hot flashes, but also your emotional response to them. Research shows that CBT can reduce the distress and disruption caused by hot flashes and night sweats, helping you sleep better and feel more in control. This mind-body technique focuses on changing thought patterns and behaviors that may amplify your symptoms.
Acupuncture and Other complementary approaches
Some women find relief through acupuncture, mindfulness meditation, yoga, or other mind-body practices. While research on these approaches is still evolving, many women report meaningful improvements in their symptoms and overall well-being. The menopause journey can be an ideal time to explore wellness practices you may not have considered before.
Innovative wearables
Technology has entered the hot flash arena with wearable devices that sense temperature changes and provide cooling or heating sensations to help regulate your body temperature. Options like the ThermaBand and Embr Wave offer on-demand relief that you can control discreetly throughout your day.
Taking action: your next steps
Hot flashes and night sweats may be common, but you don’t have to simply endure them. Here’s how to take charge:
1. Track your symptoms.
Keep a detailed log of when hot flashes occur, their intensity, potential triggers, and how they affect your daily life. This information is invaluable when discussing treatment options with your healthcare provider.
2. Talk to your healthcare practitioner.
Don’t minimize your symptoms or assume “this is just how menopause is.” Be specific about how hot flashes are affecting your quality of life. Ask about ALL available treatment options, including the most recent Menopause Society hormone therapy guidelines, non-hormonal prescription medications, and alternative approaches.
3. Find a menopause-trained specialist.
If your current healthcare provider isn’t meeting your needs or doesn’t seem knowledgeable about the latest treatment options, consider finding a practitioner certified by The Menopause Society. These specialists stay current on the latest research and treatment approaches. pausitive health collaborates with Pandia Health, Stella, and MyMenopauseRx.
4. Don’t underestimate the potential impact of lifestyle modifications.
Layer your clothing, identify your food triggers, maintain a healthy weight, and optimize your sleep environment. These changes alone can significantly reduce symptom severity.
5. Download helpful resources.
Get started with pausitive health’s menopause-friendly grocery shopping list that includes foods specifically selected to help you feel better today and support your long-term health.
6. Don’t go it alone.
Connect with other women+ on the menopause journey. Sharing experiences and strategies can be empowering and reassuring.
Don’t let hot flashes control your life
Hot flashes and vasomotor symptoms are a common part of the menopause journey, but they don’t have to control your life. With recent advances in our understanding of hormone therapy safety, new non-hormonal prescription options, and a growing toolkit of lifestyle modifications and alternative approaches, you have more choices than ever before.
The key is being proactive. Don’t wait until symptoms become unbearable—start making healthy adjustments now. Whether you choose hormone therapy, non-hormonal medications, lifestyle changes, herbal remedies, or a combination of approaches, the goal is finding what works best for your body and your life.
Remember, you deserve to feel comfortable in your own skin. Hot flashes are treatable, and with the right approach, you can minimize their impact and protect your long-term health. Take that first step today—your future self will thank you.
Free Support
For A Limited Time!
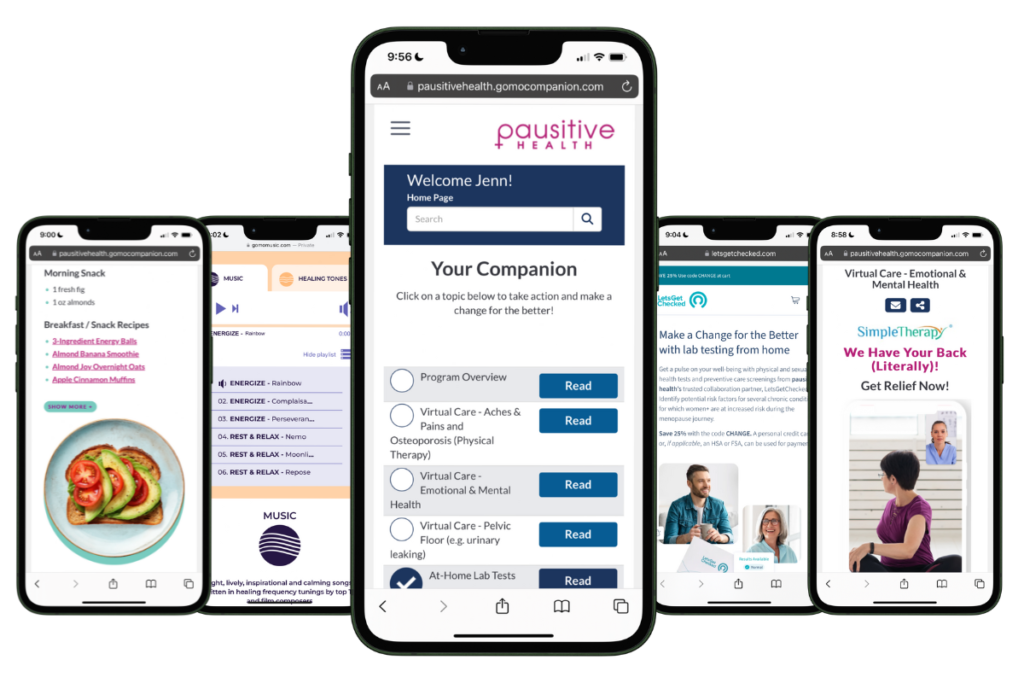
pausitive health offers personalized support for every stage of the menopause journey. Customize your experience with 14 evidence-based educational tracks, a diet assessment with recommendations and a food library, solutions for aches and pains, virtual care options, practical lifestyle supports, and a supportive community. All in one trusted place.
Join the pilot and be the first to know when our web-app is coming in 2026!

