Caring for myself is not self-indulgence. It's self-preservation.
~ Audre Lorde
How would you describe your menopause journey so far? If you’re part of the LGBTQIA+ community, you may have noticed that menopause conversations are often centered around the experiences of cisgender women. But like many other aspects of being LGBTQIA+, menopause presents a complex and nuanced journey—including unique risk factors—for individuals who identify across the diverse spectrum of sexual orientations and gender identities.
At pausitive health, we believe that everyone deserves a healthy and empowered menopause experience. While systemic changes are needed to advance gender-affirming, informed, and inclusive healthcare, it’s also important you personally have a prescription for better health. Knowing about conditions for which your risk may be greater and the factors that make them more likely helps you optimize your health and be your own best advocate as you navigate the healthcare system.
A prescription for better LGBTQIA+ health
As you near or enter menopause, health is so much more than symptoms caused by changing hormones! Everything from loneliness to cancer risks can impact your health, so assessing the possibilities and taking positive action are important.
At pausitive health, inclusivity is foundational. It means seeing individuals as whole people, including their diverse backgrounds and lived experiences.
7.2% of the U.S. Population
identifies as lesbian, gay, bisexual, transgender, or something other than heterosexual.
Source: 2023 GALLUP Poll
Menopause can present a complex and nuanced journey.
For many measures of mental and physical health, lesbian, gay, bisexual, and transgender people tend to have greater risks and poorer health outcomes early on compared to their heterosexual counterparts. This trend continues throughout middle age as well.
Disparities for LGBTQIA+ individuals can be caused and/or exacerbated by systemic issues like socioeconomic status (a measure of an individual’s or group’s standing in the community determined by income/wealth, education level, occupation, and social class), insufficient access to quality care, and other intersecting factors like racism.
Termed by Black feminist lawyer Kimberlé Crenshaw, this framework is often referred to as intersectionality and can help patients and practitioners understand how different social and political identities can result in different combinations of discrimination.
The minority stress model further explains these contributory factors. It refers to the stresses affecting individuals from stigmatized groups as a result of their minority status in society.
These stressors are experienced in addition to the general stressors felt by all people—which means they can amount to disproportionate burdens with significant negative implications for health and well-being both now and in the years to come!
For some people, they can also result in coping strategies that are not health-supporting, such as self-medicating with alcohol.
Health/care disparities and increased health risks
To use and benefit from a prescription for better health, it’s important to understand potential risks, disparities, and coping strategies that can impact your overall well-being during the menopause journey and beyond. They include:
- Several types of cancer
- Tobacco
- Drugs and alcohol
- Loneliness
- Depression and anxiety
- Weight issues
- STDs/Is
- Scars and infections from silicone
- Health insurance disparities
- Reluctance to seek healthcare due to past negative experiences

1. Cancer
In general, cancer risks are higher for lesbian and bisexual women. These include:
- cervical
- ovarian
- breast
But those are not the only cancers for which LGBTQIA+ people are at increased risk.
It is also higher for these cancers:
- endometrial (cancer of the uterus)
- anal
- colorectal
- prostate
- lung
Cancer is an area of health disparity for the LGBTQIA+ community because of a number of factors, but some of which include increased risk attributed to:
- tobacco use
- alcohol use
- not having biological children or having them later in life
- higher rates of obesity
- high-fat diets
- discrimination
- lack of access to health insurance
For each type of cancer, we’ve detailed some of the cancer risk factors and screening methods, so you have a prescription for health!
In general, talk to your doctor about these screenings:
- HPV (human papillomavirus)
- mammogram (females and transgender men who still have breasts)
- Pap smear
- colonoscopy
- prostate exam (transgender women)
Screenings help, but you also need to pay attention to your body and talk to your healthcare practitioner about any new or changing symptoms that may be early warning signs that merit evaluation.
2. Tobacco
Similar to drugs and alcohol, studies have found that LGBTQIA+ individuals use tobacco more than heterosexual people—15.3% compared to 11.4%.
In addition to the potential stressors discussed previously, this trend may be traced back to the LGBTQIA+ population being one of the first groups targeted by Big Tobacco campaigns.
The health risks of tobacco are many and include cardiovascular disease, lung cancer, and COPD (emphysema and chronic bronchitis).
For transgender individuals using estrogen therapy, smoking can be especially dangerous, as it increases the risk of blood clots.
3. Drugs and alcohol
Many people unwind with a glass of wine or cocktail at the end of the day or with dinner over the weekend. However, relying on substances to de-stress can lead to an unhealthy habit, especially given the ways alcohol can impact you during menopause and the overall risks to your health in general, e.g., cancer and cirrhosis in the case of alcohol.
In fact, many in the medical community now believe there is no safe level of alcohol consumption for anyone.
Even if drinking starts out with low to moderate consumption, unhealthy habits can progress to substance use disorder and addiction, particularly if there is a preexisting genetic predisposition.
Risk of alcohol use is nearly 2x higher for lesbian, gay, and bisexual adults
and up to 4x as high for transgender individuals.
Possibly due to their unique stressors, substance misuse in the LGBTQIA+ population, including use of alcohol and illicit drugs, often begins as a way to deal with painful emotions and to self-medicate.
4. Loneliness
As you are well aware, there are many ways to create a community filled with love and support. For some people, children provide purpose, company, and legacy. LGBTQIA+ people are less likely to have children, and they’re also more likely to live alone as they age.
Being alone and loneliness are not the same thing, nor does being alone automatically reflect or imply isolation. And having children does not guarantee you won’t be alone, lonely, or isolated.
However, experiencing chronic loneliness and social isolation does have significant negative impacts on health and well-being.
Loneliness can have the same effects as smoking 15 cigarettes a day,
having alcohol use disorder, or being physically inactive.
It's also twice as harmful to physical and mental health as obesity.
Loneliness and social isolation increase the risk of many health events and chronic conditions, including:
- Premature death (in some studies, it’s more predictive in those younger than age 65)
- Dementia (50% increased risk)
- Cardiovascular disease (heart disease – 29% and stroke – 32%)
- Anxiety, depression, and suicide
Unfortunately, loneliness and social isolation have been found to be more common in the LGBTQIA+ community. Some reasons include:
- Although some progress has been made, societal stigma, bias and discrimination, hate, and violence are still very much alive in many settings, geographic locations, and segments of the non-LGBTQIA+ community.
- Rejection by family, friends, and colleagues
- Living closeted or “double life”
Leading predictors of loneliness include the size and diversity of one’s social network and being physically isolated. A study of trans and gender-diverse people also found that education level and employment rate were contributory factors.
The COVID-19 pandemic has also accelerated rates of loneliness and social isolation, regardless of gender identity and sexual orientation, with their effects expected to continue globally for years to come. Accordingly, the Surgeon General has sounded the alarm and created an Advisory to address what he considers an epidemic of another type.
"When everything goes to hell, the people who stand by you without flinching–they are your family."
~ Jim Butcher
Here are some ways to cope:
- Remember there are all sorts of families, not all of them biological. Many a chosen family is happier and has healthier relationships than those into which one is born!
- Volunteering can be a great way to meet people and build friendships. It also comes with its own set of positive benefits for your health and well-being, like helping to combat stress, anxiety, depression, and anger. And it can provide an additional source of purpose in community with those with similar interests and a desire to give back.
- Reconnect with friends from the past. Life gets hectic, time passes, and the next thing you know 25 years have gone by. When you reach out, you may discover there’s still a bond to jumpstart a friendship.
- Take up a new hobby (or return to one you enjoyed in the past) for which you’ve been saying for years “one of these days, I’m going to xxx.”
- Get a pet! Depending on your responsibilities at home or at work, your budget, how often you need to travel, and your temperament, a pet can have a positive impact on loneliness and social isolation and may present opportunities to interact with other animal owners. However, having a pet comes with its own set of responsibilities, requires patience, and can be expensive, all of which can be stressful for some people.
- Beware of the possibility that social media may make you feel worse. Seeing pictures of what appears to be a perfect life filled with non-stop happiness (a life that does not exist!) lends itself to unhelpful comparisons and feelings of isolation. Plus, confusing social media personas and ‘likes’ with true human connection and having friends can further feelings of loneliness and isolation.
- Avoid equating being alone with being lonely. You can be in a crowd and feel lonelier than ever. Being alone can also be a time to decompress, relax, and appreciate yourself and all you bring to others. Many people find they enjoy their own company! And being alone can help you discover or unearth parts of yourself you’ve hidden for years in order to become a persona that society or work settings expect.
- Don’t hesitate to seek help. If you are facing an emotional crisis, dial 988 for free and confidential mental health support and care available 24 hours a day. And for non-emergency situations, explore resources and care from a medical professional.

5. Depression and anxiety
In line with the minority stress model, women who have sex with women may be at a higher risk of depression and anxiety than their heterosexual counterparts—twice as high for lesbian, gay, and bisexual adults and nearly four times as high for transgender individuals. These risks can be heightened for bisexual individuals.
Care and support are vital to our well-being, and at times, LGBTQIA+ people may not receive acceptance from their loved ones or society and experience microaggressions or even outright rejection.
For LGBTQIA+ adults, the risk of suicide is higher as well – twice as high for lesbian, gay, and bisexual people and nearly four times as high for transgender individuals.
LGBTQIA+ people may also experience violence or abuse just for being who they are. For example, rape and sexual assault are ten times more likely in the LGBTQIA+ community.
For individuals who haven’t shared their sexual orientation or gender identity with others, mental distress may be even more severe. For example, a study found that in sexual minority women, being closeted was associated with a greater likelihood of reporting depression than those who were recently out. Remember that your feelings are valid, and it’s essential to find trusted support.
Call 9-8-8
6. Weight issues
Obesity and being overweight can lead to many other health problems, such as heart disease and diabetes. While the reasons behind this trend are still being explored, lesbian and bisexual females are more likely to struggle with their weight and related conditions.
In turn, carrying extra weight, particularly when it settles around the waist, and the fat settles around internal organs, sets up a cascade of inflammation that can increase the risk of chronic conditions like cardiovascular disease, diabetes, and many cancers.
7. STDs/Is
Sexually transmitted diseases (STDs) are comprised of a variety of conditions that result from sexual contact. They can be spread during vaginal, oral, or anal sex, as well as sexual contact involving the penis, vagina, mouth, or anus.
STDs are caused by sexually transmitted infections (STIs). While STDs have accompanying symptoms, STIs don’t always cause symptoms. STIs can also occur as a result of a blood transfusion or shared needles (and can even spread to infants during pregnancy or childbirth.)
While many STDs and STIs can go undetected, possible signs and symptoms include:
- Abnormal vaginal bleeding or discharge with an unusual odor or consistency
- Pain or a burning sensation when urinating
- Pain during sex
- Fever
- Fatigue
- Rashes over the hands, feet, or trunk
- Sores, bumps, or irritation in the vaginal, oral, or rectal area
- Abdominal pain
- Swollen lymph nodes, especially in the groin area
Common STDs include HPV (the most common STD in the U.S.), chlamydia, gonorrhea, herpes, syphilis, trichomoniasis, and HIV. Hepatitis is also considered an STD.
According to the CDC, chlamydia, gonorrhea, and syphilis have been on the rise since 2014 in bisexual men (and by extension in heterosexual and bisexual women who have bisexual male sexual partners) and gay men. And there is a rising number of infections across the board in the U.S. regardless of sexual orientation or gender identity in post-menopausal women 55 years of age and older.
HIV is also more prevalent in LGBTQIA+ populations. As a 2021 Centers for Disease Control (CDC) survey found, 40% of transgender women reported having HIV, and people assigned female at birth accounted for 24% of new HIV infections.
Another contributing factor to high rates of STDs/Is for LGBTQIA+ people is bacterial vaginosis (BV), a condition caused by an overgrowth of normal vaginal flora. It is more commonly seen in bisexual and lesbian people and can often be seen in both women in a lesbian relationship. Unfortunately, if left untreated, BV increases the risk of chlamydia, gonorrhea, pelvic inflammatory disease, and HIV.
8. Scars and infections from silicone
People of any sex or gender identity may choose to inject silicone or fillers to change their body appearance. These are common practices in transgender individuals who choose to undergo gender-affirming medical procedures. However, because of financial limitations or lack of medical support or expertise, some transgender individuals may be more likely to receive silicone from non-medical persons, as well as substances that may be contaminated or inappropriate for human use, causing scars, infections, bleeding, or allergic reactions.
To avoid or remediate these complications, it’s important to seek treatment from board-certified dermatologists and plastic surgeons experienced in gender-affirming care.
9. Health insurance disparities
Despite strides being made in inclusive policies, some health insurance providers still don’t cover unmarried partners as dependents or cover gender-affirming care. Combined with biases and discrimination, this can make it more difficult for LGBTQIA+ individuals to get equal access to quality healthcare. As such, more LGBTQIA+ people are uninsured than their heterosexual counterparts, a component of which reflects a higher level of unemployment (and therefore lack of access to job-related coverage) and lower household income levels for some individuals.
10. Reluctance to seek healthcare
Even those in the LGBTQIA+ community who do have healthcare providers are still less likely to seek help. When it comes to care, a sense of psychological safety is essential!
During the menopause journey, many individuals already feel their experiences are discounted, and medical gaslighting can be more pronounced in the LGBTQIA+ population. For example, LGBTQIA+ people are more likely to report a provider:
- has not believed them
- dismissed them
- made assumptions
- has suggested they were to blame for their health problems.
It’s no surprise, then, that sexual and gender minorities are less likely to seek support. For example, according to a study from the American Association for Cancer Research, nearly 1 in 4 report avoiding healthcare out of fear of discrimination.
23% of transgender people did not seek necessary care
due to fear of mistreatment.
Transgender individuals can experience menopause, so gain an understanding of what that experience may be like and talk with an inclusive provider.

How to care for your unique health and well-being needs
Your prescription for health should include regular screenings and visits with your healthcare practitioner as well as healthy habits for life.
Get regular GYN care
Even though lesbian and bisexual women are more likely to develop certain gynecologic cancers, such as cervical and ovarian, they’re less likely to receive gynecological health care. Talk to your doctor to schedule both a pelvic exam, Pap smear and HPV testing on a regular basis based on the most current guidelines. These procedures can help detect conditions like cancer early, improving the chances of curative treatment.
Get screened for breast cancer
Even if your doctor doesn’t bring it up, it’s essential to discuss breast cancer screenings to determine the best approach for you based on factors like your personal and family history, potential genetic mutations, your hormone profile, age, and hormone therapy regimen (or lack thereof). Although cisgender women make up the largest demographic relative to developing breast cancer, trans men and women, and non-binary people (and cisgender men) can also get breast cancer.
There is ongoing controversy in the medical community around breast cancer guidelines, particularly with regard to age to start, frequency of mammography, and use of other imaging techniques in those with dense breasts.
Below are various medical societies and organizations that provide guidance. They are not always in exact agreement, so a discussion with your healthcare practitioner about your specific situation is important!
- American Cancer Society
- U.S. Preventive Service Task Force (USPSTF)
- American College of Radiology (ACR) (includes a recommendation for risk assessment of all women, especially those who are Black or Ashkenazi Jews, by age 25 to determine if screening earlier than age 40 is needed)
Safe sex and STD/I testing
Sex can be a joyful and fulfilling part of relationships. Besides the physical pleasure, it can strengthen the emotional bond with your partner and bring another level of intimacy and trust.
For those who engage in penetrative vaginal sex, more frequent sexual activity that brings blood flow to the genital area and stimulates lubrication can also lessen symptoms and complications of genitourinary syndrome of menopause (GSM), like less genital sensitivity (which can make reaching orgasm more difficult) or narrowing and shortening of the vagina.
But there are steps you can take to stay as safe as possible.
- During oral sex, use either a latex condom or a dental dam. If you use sex toys, either wash them between uses or cover them with a condom.
- STDs/Is can spread in many ways, so consider using a condom on your finger if it’s involved in vaginal or anal penetration.
- Remember that infections don’t always show symptoms, so getting tested is the only way to know for sure. With a new partner, get tested and make sure your partner has been tested, too! You can even schedule an appointment to get tested together to prioritize and normalize conversations around safe sex. And if you have engaged in high-risk sexual activity, have been exposed to someone who you learn or suspect has an infection, or wonder if you might be infected, get tested so treatment can begin as soon as possible if the result comes back positive.
- Consider the possible risks of having multiple sexual partners.
- If your partner has or is at risk for HIV, you may also benefit from taking PrEP, or pre-exposure prophylaxis, which can help reduce the risk of infection.
Limit/eliminate alcohol and don’t use drugs
Alcohol and drug use can lead to risky behaviors like engaging in unsafe sex. Alcohol use is also a risk factor for conditions like heart and liver disease and many cancers.
Recent research suggests there is no safe level of alcohol consumption.

Be open with your healthcare providers
Because of the increased health risks for many physical and mental health conditions experienced by individuals who are in the sexual orientation and gender minority, advocating for yourself and learning effective ways to navigate the healthcare system are essential measures to getting the most appropriate care for your particular situation.
It’s also important to have a healthcare practitioner with whom you feel you can be honest. Open communication will help them provide the most effective and compassionate care. You may encounter doctors who don’t help you feel comfortable. If that’s the case, try to find another provider if that option is available.
To help you get started, we’ve shared resources below regarding providers who are welcoming to the LGBTQIA+ community.
Remember the information in this article is based on statistics—and we’re all so much more than a number! While certain health trends are found in LGBTQIA+ populations, they may or may not apply to you as an individual. Being equipped with facts will help you make the best decisions for yourself and locate the type and quality of healthcare you need and deserve.
LGBTQIA+ trained providers and additional health support
- Folx Health provides virtual care for the LGBTQIA community in all 50 states.
- Point of Pride: Financial aid and health support for transgender individuals.
- GLMA Health Professionals Advancing LGBTQ+ Equality: A LGBTQ+ Healthcare Directory
- Trans Lifeline: The nation’s only crisis and peer-support hotline for trans people. Visit online or call (877) 565-8860.
- LGBTQ Psychotherapists of Color: A volunteer-led group that provides support and community building for LGBTQ individuals in Psychology, Social Work, and Counseling.
- The National LGBT Cancer Network: A directory for LBGT-friendly cancer treatment facilities.
- VHA LGBTQ+ Health Program: Healthcare services for LGBTQ+ veterans.
- Included Health Bisexual Health Checklist
- Included Health Gay Health Checklist
- Including Health LGBTQ+ affirming mental health resources
- Included Health Guide for LGBTQ+ patients
- American College Health Association: A coalition of programs, projects, and other resources for LGBTQ individuals.
- You can also check out pausitive health’s guide – “Menopause Pride: The LGBTQIA+ Experience and Where to Find Inclusive Doctors“
- LGBT National Help Center
Free Support
For A Limited Time!
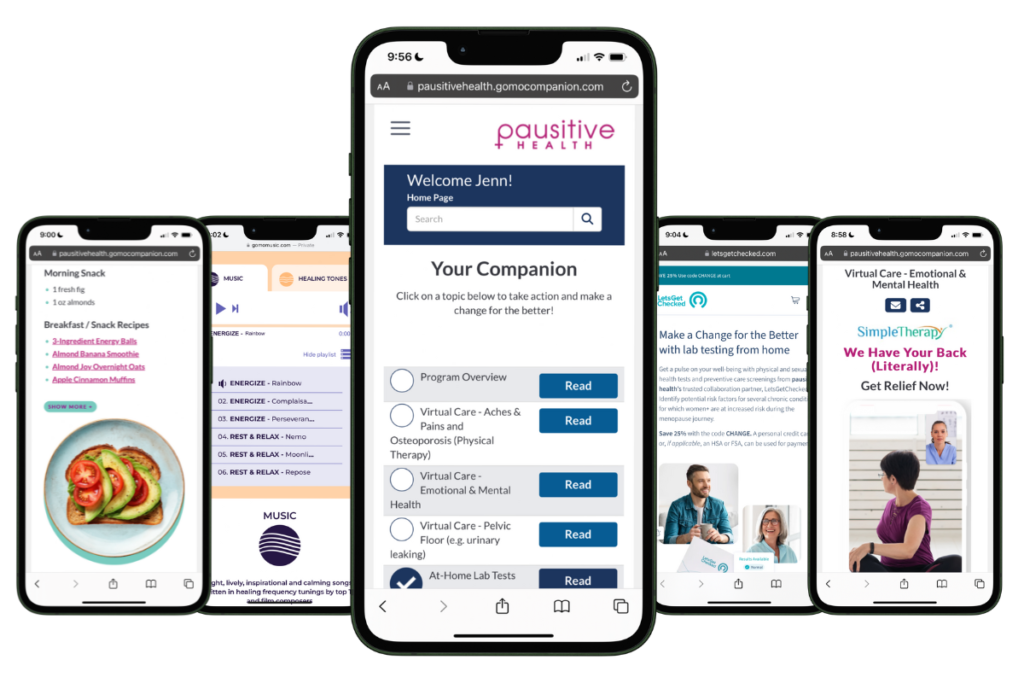
pausitive health offers personalized support for every stage of the menopause journey. Customize your experience with 14 evidence-based educational tracks, a diet assessment with recommendations and a food library, solutions for aches and pains, virtual care options, practical lifestyle supports, and a supportive community. All in one trusted place.
Join the pilot and be the first to know when our web-app is coming in 2026!
Lee A, Rajagopalan S, Ayresleigh R, Viloria R. Developing an Obstetrics and Gynecology Residency Curriculum for the Care of Gender-Diverse Patients. Obstetrics & Gynecology. 2023, Volume 141, Supplement 1, pages 90S-90S(1). DOI: https://doi.org/10.1097/01.AOG.0000931096.06293.f0
U.S. LGBT Identification Steady at 7.2% | Gallup
Medina-Martínez J, Saus-Ortega C, Sánchez-Lorente MM, Sosa-Palanca EM, García-Martínez P, Mármol-López MI. Health Inequities in LGBT People and Nursing Interventions to Reduce Them: A Systematic Review. Int J Environ Res Public Health. 2021 Nov 10;18(22):11801. doi: 10.3390/ijerph182211801. PMID: 34831556; PMCID: PMC8624572.
LGBT+ People’s Health Status and Access to Care | KFF
Not Up for Debate: LGBTQ People Need and Deserve Tailored Sexual and Reproductive Health Care | Guttmacher Institute
Crenshaw, K. Demarginalizing the Intersection of Race and Sex: A Black Feminist Critique of Antidiscrimination Doctrine, Feminist Theory and Antiracist Politics. 1989. University of Chicago Legal Forum: Vol. 1989, Article 8.
Alcohol and health: all, none, or somewhere in-between? The Lancet Rheumatology. 2023. Volume 5, Issue 4, E167. DOI:https://doi.org/10.1016/S2665-9913(23)00073-5
Day J, Fish J, Perez-Brumer, A. Transgender Youth Substance Use Disparities: Results From a Population-Based Sample. 2017. Journal of Adolescent Health. Volume 61, Issue 6, P 729-735. DOI:https://doi.org/10.1016/j.jadohealth.2017.06.024
New NIH Study Reveals Shared Genetic Markers Underlying Substance Use Disorders | National Institute on Drug Abuse
Why the Risk of Substance Use Disorders Is Higher for LGBTQ People | Healthline Media
Day J, Fish J, Perez-Brumer A, Hatzenbuehler M, Russell S. Transgender Youth Substance Use Disparities: Results From a Population-Based Sample. Journal of Adolescent Health. 2017. Volume 61, Issue 6, P729-735. https://doi.org/10.1016/j.jadohealth.2017.06.024
Kim HJ, Fredriksen-Goldsen KI. Living Arrangement and Loneliness Among Lesbian, Gay, and Bisexual Older Adults. Gerontologist. 2016 Jun;56(3):548-58. doi: 10.1093/geront/gnu083. Epub 2014 Sep 11. PMID: 25213482; PMCID: PMC4873763.
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., & Stephenson, D. (2015). Loneliness and Social Isolation as Risk Factors for Mortality: A Meta-Analytic Review. Perspectives on Psychological Science, 10(2), 227-237. https://doi.org/10.1177/1745691614568352
National Academies of Sciences, Engineering, and Medicine. 2020. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System. Washington, DC: The National Academies Press. https://doi.org/10.17226/25663.
LGBTQ+ Isolation Is a Public Health Problem | Psychology Today
Peterson N, Lee J, Svec J, Russell D. Diversity in Social Communication and Support: Implications for Loneliness Among LGB Adults. The Gerontologist, Volume 63, Issue 2, March 2023, Pages 361–72. https://doi.org/10.1093/geront/gnac101
New Surgeon General Advisory Raises Alarm about the Devastating Impact of the Epidemic of Loneliness and Isolation in the United States | U.S. Department of Health and Human Services
Our Epidemic of Loneliness and Isolation (2023) | Office of the Surgeon General
The Health Benefits of Volunteering | Corporation for National & Community Service
LGBTQ+ Mental Health Resource Center | Mental Health America
LGBTQ Mental Health Resources | The Mental Health Coalition
Adult Health | Mayo Clinic
LGBTQ Health Disparities: Finding Better Care, Safety, and Well-Being | BetterUp
Suicide Risk and Prevention for LGBTQ People | National LGBT Health Education Center
More Than 40% of Transgender Adults in the US Have Attempted Suicide |The Williams Institute
VAWA and LGBTQ People | The Williams Institute
Pachankis JE, Cochran SD, Mays VM. The mental health of sexual minority adults in and out of the closet: A population-based study. J Consult Clin Psychol. 2015 Oct;83(5):890-901. doi: 10.1037/ccp0000047. Epub 2015 Aug 17. PMID: 26280492; PMCID: PMC4573266.
Wolfgang, K.M., Takeshita, J., Fitzsimmons, R. et al. The association between sexual orientation, BMI, obesity diagnosis, and provider recommendation for weight management. BMC Women’s Health 22, 19 (2022). https://doi.org/10.1186/s12905-021-01585-x
Sexually Transmitted Diseases (STDs) | Mayo Clinic
Human Papillomavirus | Office on Women’s Health
U.S. STI Epidemic Showed No Signs of Slowing in 2021 – Cases Continued to Escalate | Centers for Disease Control and Prevention
Bacterial Vaginosis | National Library of Medicine
Yeung H. Complications of Silicone Injections: Persistence, Stigma, and Treatment. Dermatology World Insights and Inquiries. 2023, Volume 5, No. 3.
Yeung H, Kahn B, Ly BC, Tangpricha V. Dermatologic Conditions in Transgender Populations. Endocrinol Metab Clin North Am. 2019 Jun;48(2):429-440. doi: 10.1016/j.ecl.2019.01.005. PMID: 31027550; PMCID: PMC6497076.
Cervical Cancer Screening | National Cancer Institute
Cancer Facts for Lesbian and Bisexual Women | American Cancer Society
Health Insurance Coverage and Access to Care for LGBTQ+ Individuals: Current Trends and Key Challenges | U.S. Department of Health and Human Services
New Analysis Finds LGBTQ+ Households Trail in Income and Wealth | Federal Reserve Bank of St. Louis
It’s Sarah, Not Stephen! | Agency for Healthcare Research and Quality
Patient Safety Concerns and the LGBTQ+ Population | Agency for Healthcare Research and Quality
The State of Cancer Health Disparities In 2022 | American Association for Cancer Research
The 2015 U.S. Transgender Survey | National Center for Transgender Equality
Lesbian and Bisexual Women’s Health Issues | Johns Hopkins Medicine
American Cancer Society Guidelines for the Early Detection of Cancer | American Cancer Society
Breast Cancer: Screening | U.S. Preventive Services Task Force
New ACR Breast Cancer Screening Guidelines Call for Earlier and More-Intensive Screening for High-Risk Women | American College of Radiology
Preventing HIV with PrEP (Pre-Exposure Prophylaxis) | Centers for Disease Control and Prevention
Leigh BC, Stall R. Substance use and risky sexual behavior for exposure to HIV. Issues in methodology, interpretation, and prevention. Am Psychol. 1993 Oct;48(10):1035-45. doi: 10.1037//0003-066x.48.10.1035. PMID: 8256876; PMCID: PMC2585544.
Get The Healthcare You Deserve | Navigating Your Healthcare Journey
Life-Changing Access. Life-Saving Affirmation. | Point of Pride
Find a Provider | GLMA Health Professionals Advancing LGBTQ+ Equality
Radical Community Care | Trans Lifeline
Find An LGBTQ of Color Psychotherapist | LGBTQ Psychotherapists of Color (QTOC)
Screening Providers | National LGBT Cancer Network
VHA LGBTQ+ Health Programs | U.S. Department of Veteran Affairs
Bisexual Health Checklist | Included Health
Gay Health Checklist | Included Health
Mental Health Resources Guide | Included Health
Breaking Barriers to LGBTQ+ Health: A Guide for Patients | Included Health
LGBTQ+ Health Coalition | American College Health Association
Care Before Crisis | LGBT National Help Center
You may also like…

Menopause Pride: The LGBTQIA+ Experience And Where to Find Inclusive Doctors
Every menopause journey is unique. For LGBTQIA+ people there are positives and challenges, like health disparities. Learn how to have menopause pride by knowing what to expect.

7 Ways to Strengthen LGBTQIA+ Relationships During Menopause
There are unique challenges for LGBTQ+ women during menopause, and it can impact your relationship(s). Learn how to strengthen them.

How Being LGBTQIA+ Can Positively Impact Your Mindset During The Menopause Journey
Learn how being in the minority for gender identity and sexual orientation can positively impact your menopause mindset.

