The problem with heart disease is that the first symptom is often fatal.
~ Michael Phelps
Think you’re too young at this point to really worry about cardiovascular disease (e.g., hypertension, heart disease, and stroke)? Wake-up call: heart disease is the #1 cause of death in women+ in the U.S. For context, it’s more fatal than all forms of cancer combined! Yet, awareness of this is dropping among women+, and during the menopause journey your risk goes up as estrogen levels drop. In addition, there are at least 18 factors – like your medical history, weight, menopause symptoms, race and ethnicity, and even where you live – that can impact your cardiovascular risk. Understanding heart health risk factors can save your life.
Heart attack facts for women
A heart attack usually occurs when there’s a blockage or underlying cardiovascular condition like heart disease. In women+, a heart attack can show up differently than in the stereotypical pictures that are often portrayed in movies and come to mind when you imagine signs and symptoms.
While chest pain or discomfort are the most frequent symptoms of a heart attack in both men and women, a heart attack in women can present with symptoms like:
- pain or discomfort in your arms, back, jaw, neck or stomach
- shortness of breath
- a cold sweat
- nausea or vomiting
- lightheadedness or fainting
- extreme fatigue
Women+, and too often emergency room staff as well, sometimes attribute these symptoms to other conditions like acid reflux.
Cardiovascular disease (CVD): #1 Killer in women
Cardiovascular disease (CVD) includes conditions of the heart or blood vessels. CVD encompasses several conditions, including:
- heart disease
- hypertension (high blood pressure)
- stroke
- peripheral artery disesase (PAD)
Women typically develop cardiovascular conditions 7-10 years later than men, with the fastest growing rates of CVD among 45-64 year old women+. As you may have noticed, that timing aligns with a typical timeframe for perimenopause, menopause onset, and the post-menopause stage of the journey.
Women are exposed to more estrogen during their lifetime, particularly during the reproductive years, and estrogen offers a protective benefit with regard to CVD. However, once estrogen levels drop during the menopause journey, the risk of CVD goes up.
Despite CVD being a leading cause of death, the 2019 National American Heart Association Survey of Women’s Cardiovascular Disease Awareness found awareness of CVD as a leading cause of death had dropped in all races/ethnicities and ages, except in women 65 or older.
The greatest declines in awareness were seen among Hispanic women and non-Hispanic Black women.
By learning more about cardiovascular risk factors for women+, you can start taking charge of your heart health as soon as today. And it actually could mean the difference between life and death!
While our focus in this article is on CVD risks associated with menopause,
it’s important to note that other circumstances like a family history of CVD, certain medical conditions, and an unhealthy lifestyle also put you at increased risk.
Cardiovascular risk factors
Risk factors for CVD run the gamut from menopause symptoms to your medical history.
You have the power to take control of your heart health and your menopause journey!
Ready to learn about the menopause risk factors? You can follow the ones listed below in order or select the ones of most interest to you and jump right to them.
CVD Risk Factors Menopausal Women Should Consider
1. Metabolic syndrome
Have you heard of metabolic syndrome? It’s a group of medical conditions that increase the risk of heart disease, stroke, and type 2 diabetes.
Metabolic syndrome is diagnosed if a person has at least three of the following five conditions:
- excess internal body fat around your organs with a waist circumference ≥ 35 inches in women+ (≥ 31.5 inches if you are Asian)
- high blood sugar (glucose)
- high blood pressure
- a high blood triglyceride (a type of fat that can increase your LDL “bad” cholesterol) level
- low HDL cholesterol (“good” ) level
While each of the medical conditions individually increases risk, when they occur in combination, it can lead to a significantly increased risk of developing cardiovascular disease. So, even if you haven’t been diagnosed with metabolic syndrome, talk to your doctor about managing the conditions that can lead to a diagnosis, especially as the menopuase joureny can increase your risk of each of these conditions.
For example:
- The loss of estrogen during the menopause journey can impact your lipid levels like cholesterol. So, get regular lab work.
- Many women gain weight during the menopausal transition, and it’s common to have a greater distribution of weight in the waist area instead of the hips or thighs. That excess internal body fat around your organs is a risk factor. So, consider exercises designed for menopausal women+ and eat foods, rich with the nutrients you need.
- A recent study found that women+ who experience severe hot flashes are at a potentially greater risk of developing both hypertension and metabolic syndrome.

2. Obesity and visceral abdominal fat
In a pausitive health survey, weight gain was the top complaint from women+ on the menopause journey. So, what’s the impact on CVD?
- Being 20 pounds or more overweight can increase the risk of high blood pressure, which is an additional risk factor for heart disease and stroke.
- Excess visceral (internal around the organs rather than just under the skin) abdominal fat — the type most common during menopause — is particularly linked to increased (by 27%) CVD risk. It sets up an inflammatory process, which can also increase the risk of blood clots and diabetes.
So, why do women gain weight during the menopause journey?
- A drop in estrogen levels can cue your body to gain weight in the abdomen versus on the thighs or hips. In fact, in post-menopausal women, belly fat accounts for 15 to 20% of their total body weight, compared with 5 to 8% in premenopausal women.
- What’s more, the loss of muscle mass that tends to occur as we age can lead to a slower metabolism. And if the onset of menopause is early, a recent study of Korean women found an increased risk of muscle loss in the senior years, as measured by handgrip strength.
- Even if you haven’t noticed it, you may be less active than you once were.
- Symptoms like hot flashes, night sweats, aches and pains – the musculoskeletal syndrome of menopause, depression, and anxiety can lead to sleep issues, which in turn impact the levels of hormones like leptin and ghrelin, which can result in increased appetite and food cravings.
Because of its relationship to CVD, it’s critical to pay attention to your weight during the menopause journey. Focus on foods packed with nutrients a woman needs on the journey. Exercise can also help with weight loss/maintenance, with the added bonus of also helping to boost energy, maintain/build muscle mass, and reduce the risk of osteoporosis.

Yoga For Lifelong Strength: 5 Yoga Types To Power Through Daily Life
Yoga can provide lifelong strength. Learn about 5 yoga types and the benefits so you can power through daily life.

Discover Inner Balance: 8 Yoga Poses To Help Manage Menopause Symptoms
Yoga can improve your emotional and physical well-being during menopause, easing symptoms like hot flashes and sleeplessness. Try these yoga poses. for menopause.

28 At-Home Osteoporosis Exercise Videos To Help Prevent or Manage It
Try these at-home osteoporosis exercise videos from our collaborative partner. They can help prevent or manage osteoporosis and osteopenia.
3. Cholesterol and an abnormal lipid profile
When was the last time you had lab work done? In most cases, the only way to know if your cholesterol or other lipids are abnormal is to have them checked.
Importantly, menopause can contribute to abnormal lipid profiles. Lipids are fats that circulate in your blood.
One of these is cholesterol. It’s a waxy substance that’s made by your liver. There’s good (HDL) and bad (LDL) cholesterol.
Another type of lipid is triglycerides. They can build up to unhealthy levels from foods you eat and when you eat more calories than you burn.
If blood levels of some of these lipids are either too high or too low, it can lead to an increased risk of heart disease, stroke, or heart attack.
During the menopause journey, the dramatic drop in estrogen levels can cause good cholesterol (HDL) levels to drop and bad (LDL) cholesterol and triglyceride levels to rise.
When you have too much LDL (bad) cholesterol in your blood, it may be deposited in the lining of the arteries. These fatty deposits narrow your arteries, including those that carry blood to your heart, which can eventually lead to coronary artery disease.. On the other hand, having a low level of HDL (good) cholesterol has been associated with a higher risk of CVD.
An abnormal lipid profile is of concern for all women+, but especially so for Black women+, who are at higher risk of both cardiovascular disease and an abnormal lipid profile.
You can monitor cholesterol and triglycerides with lab work.
By taking action, like eating healthy foods (especially ones packed with nutrients needed for menopause), exercising regularly, and maintaining a healthy weight, you reduce the risk of developing an abnormal lipid profile and the likelihood of needing to take medication to do so.
4. Diabetes
Here’s what we know about diabetes and CVD:
- Individuals with type 1 or type 2 diabetes are twice as likely to have heart disease at a younger age than those without diabetes.
- The longer you have diabetes, the more likely you are to have heart disease. This occurs because high blood sugar can damage blood vessels and the nerves that control your heart.
Because being overweight raises your risk of type 2 diabetes, weight gain during menopause may be responsible for the association between diabetes and menopause. Additionally, if you experience premature (age younger than 40) or early (between age 40 and 45) menopause, you are also at a greater risk of type 2 diabetes.
You should have your doctor check your glucose levels at least every three years. These levels measure your blood sugar, which could help identify diabetes.
5, Polycystic ovary syndrome (PCOS)
There is also a connection between diabetes and polycystic ovary syndrome (PCOS), another risk factor for CVD.
PCOS is a condition affecting 5 – 10% of women in which the ovaries produce excess androgens (male hormones that women have in small amounts).
If you were diagnosed with PCOS during your reproductive years, you may be at an increased risk of a future cardiovascular event.
In fact, studies suggest that women with PCOS are twice as likely to have a heart attack or stroke.
While there is no single criterion for diagnosing PCOS, possible symptoms include missed or irregular periods, ovarian cysts, excess body hair, acne, weight gain, and infertility.
Many risk factors seen in people with cardiovascular disease, such as being overweight or having insulin-resistant diabetes, are also linked to PCOS. While the connection between diabetes and PCOS is not entirely understood, higher androgen levels are also a risk factor for diabetes.
Many women with PCOS are insulin resistant, which can make it difficult to maintain normal blood glucose levels. In fact, 35% of women with PCOS have prediabetes, and 10 percent go on to develop diabetes by age 40.
6. Hot flashes
Do you have hot flashes, night sweats, or heart palpitations? These are known as vasomotor symptoms.
There is some evidence hot flashes can be an indicator of heart health, but the connection is not clear. Like so many other things with menopause, research is ongoing, and we’re learning more each day.
Here’s what the research currently tells us:
Research indicating heart health and hot flashes may be connected:
- If hot flashes continue into the post-menopause stage and are severe, one study found women are more likely to develop metabolic syndrome and high blood pressure.
- Hot flashes are also closely linked to poor CVD health metrics. These metrics, identified by the American Heart Association, help someone establish good cardiovascular health. In relation to hot flashes, women+ had higher blood pressure and body mass index, as well as abnormal lipids. At normal levels, all three are better for your heart health.
Research showing there is not a link:
- Another study found women+ with two or more moderate to severe menopausal symptoms had an increased risk of CVD, but vasomotor symptoms were not one of those symptoms.
Remember, hot flashes are one potential risk factor for cardiovascular disease. Given the research is conflicting, there is even more reason to talk to your doctor about next best steps to manage VSMs and CVD risks.
Also, hot flashes can impact your quality of life, which is another risk factor you can also learn about in this article. You may also want to learn about ways to manage hot flashes, so in addition to possibly helping heart disease, they don’t also impact your quality of life as much.

Hormone-Free Hot Flash Relief: 12 Non-Hormonal Medications To Try
Want to beat the heat from hot flashes hormone-free? Try these non-hormonal hot flash medications that are FDA-approved or used off-label.

Black Women and Menopause: Why Symptoms Can Be Longer and More Severe
As a Black woman, menopause symptoms, including hot flashes, can be longer and more severe. Learn why and what you can do.

Conquer Menopausal Hot Flashes And Sleeplessness With CBT
Learn about cognitive behavioral therapy or CBT to help manage hot flashes, night sweats, and sleeplessness.

7. Insomnia
For women on the menopause journey, sleepless nights are common. Aches and pains, night sweats, and palpitations can lead to problems with falling asleep, staying asleep, and getting enough good quality sleep. And the result includes fatigue, problems with focus and concentration, weight gain, and an increased risk of cardiovascular disease.
If these issues occur 3 or more nights a week, last more than 3 months, and cannot be fully explained by another health problem, a diagnosis of chronic insomnia can be made.
Experienced by about 10 – 15% of people in the U.S., insomnia occurs when your day-to-day feelings and functioning are impacted by poor or insufficient sleep despite having an adequate opportunity to sleep.
Insomnia increases the risk of cardiovascular disease in several ways:
- increased inflammation and stress
- a causal connection to obesity, diabetes, and depression
- excessive daytime sleepiness
- negative impact on lifestyle habits, leading to behaviors like unhealthy eating, being sedentary, and self-medicating with alcohol
Besides heart disease, insomnia also impacts the likelihood of having a stroke. Compared to those who don’t have trouble sleeping, those with insomnia have close to a 51% higher risk of stroke, especially in people younger than 50.
Insomnia health disparities
As with many conditions, health disparities are observed with insomnia. Even before menopause, women report experiencing insomnia more often than men.
White adults are more likely to have trouble falling asleep than Hispanic, Black, and Asian adults.
Do you know what’s interrupting your sleep? Learn more about potential contributory factors besides dropping estrogen levels. And then get into a sleep routine as well as try techniques like binaural beats and cognitive behavioral therapy (CBT).

Why Women+ Are Prone To Restless Leg Syndrome (RLS) And How To Treat It
Do your legs move uncontrollably at night? Learn why Restless Leg Syndrome (RLS), is more common in women and how to treat it.

Having Leg Pain And Cramps? You May Be In Menopause
Do you have leg pain and cramps, during the day or at night? It’s a menopause symptom. Learn how to treat the leg pain.
Why Can’t I Sleep During The Menopause Transition? Understanding It Can Help You Sleep
Understanding why you can’t sleep during perimenopause and menopause can help you get more sleep.
8. Moderate-to-severe menopausal symptoms
How many menopause symptoms do you have? Now, how many are moderate-to-severe?
If you have two or more moderate-to-severe symptoms, researchers found your CVD risk goes up, including an increase in the risk of stroke.
In the trial, women+ who had these moderate-to-severe symptoms had a higher risk of CVD:
- dizziness
- heart racing
- restlessness
- feeling tired
- difficulty concentrating
- forgetfulness
- headaches or migraines
Remember, you have options. Talk to your healthcare practitioner about hormonal and non-hormonal medications and techniques to manage symptoms.
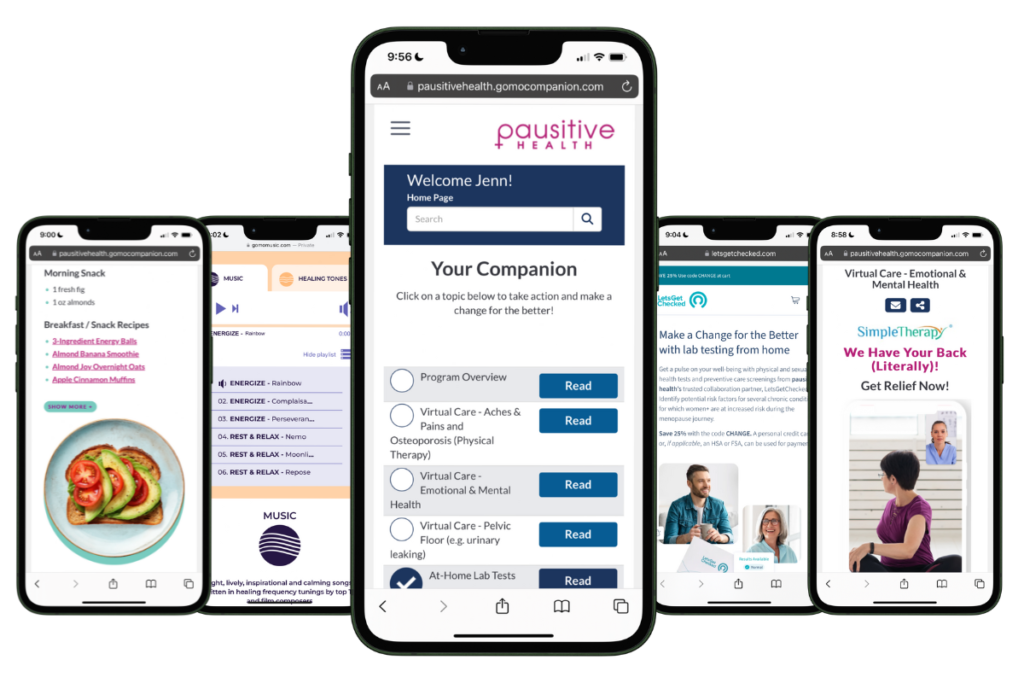
Free Support
For Your Menopause Journey!
Only available for a limited time!
Access a one-stop menopause journey digital destination that provides personalized text messages that focus on educational topics you select and offers many other features such as a diet assessment with recommendations, solutions from collaboration partners to address menopausal aches and pains (the musculoskeletal syndrome of menopause – MSM), pelvic floor issues, virtual care, lifestyle tools, and a supportive community.

VEOZAH: Medical Breakthrough Gives Women+ More Hot Flash Treatment Options
VEOZAH (fezolinetant) is a new breakthrough medication for hot flashes, that’s non-hormonal. It can reduce the frequency and severity.

How To Balance Hormones During Menopause: Is Hormone Therapy (HT) Safe?
Is hormone therapy safe? Learn about the potential pros and cons of HT for menopause.

Non-Hormonal 101
95% of women… would try hormone alternatives before HT. Source: Women’s Health Concern Non-Hormonal Options 101 How are you managing your menopause symptoms? You have
9. Quality of life during menopause
What’s your quality of life like during menopause?
Menopause symptoms can impact the quality of your life, even if symptoms are mild. Perhaps you have multiple mild symptoms or other life challenges that can make it difficult to manage everything.
In a Korean study about menopausal quality of life, researchers looked at 29 areas in four domains. Some of the symptoms on the questionnaire included:
1. Vasomotor
- hot flashes
- night sweats
- palpitations
2. Psychosocial
- dissatisfaction with life
- anxiety and depression
- impatience
- accomplishing less than usual
- poor memory
- a desire to be alone
3. Physical
- bloating, flatulence (gas)
- tiredness, difficulty sleeping
- drying skin
- stress incontinence
4. Sexual
- intimacy avoidance
- changes in sexual desire
- vaginal dryness during intercourse
How many of these quality-of-life boxes describe your menopause journey? The study found a higher prevalence of CVD when women+ had symptoms in all 4 areas.
Having your day-to-day quality of life negatively impacted is definitely another reason to reach out to your healthcare practitioner to discuss the many options available to help manage symptoms.

When Perimenopause Depression Steals Your Joy: How To Recognize It And Cope
Are you feeling down? Perimenopause depression is a common symptom. Learn about the symptoms and treatment options.

Reignite Passion: How To Manage Genitourinary Syndrome Of Menopause (GSM)
Are you experiencing vaginal dryness, no orgasm, or painful sex? If you wait or don’t have sex, it can get worse. Try these menopause treatments.

Menopause Bloating and Constipation? Don’t Suffer From GI Pain Any More
Does your stomach hurt or feel bloated? Menopause GI pain can cause several symptoms in your gastrointestinal tract. Learn how to manage them.
10. Stage of menopause
The risk for CVD goes up as you progress through the stages of menopause, and estrogen levels continue to fall to a new low baseline in post-menopause.
Post-menopausal women are at higher risk than perimenopausal women.
It can take up to 10 years to move through the stages of menopause, particularly if you are a Black woman+. Knowing where you are in the journey can help determine risk and any potential next steps. But developing healthy lifestyle habits is always a good place to start, both now and for your future health and well-being.
A new test, Clearblue, is now available which reportedly indicates your stage of menopause. Since global menopausal testing of all women+ is not recommended, it would be a good idea to speak with your doctor to determine if testing would be of value in your particular situation.
11. Premature and early menopause
When did you start menopause? Knowing if it’s “premature” or “early” is important because the timing can put you at higher risk for certain conditions for a longer time, including cardiovascular disease.
Early menopause (age 40-45) and premature menopause (age <40) means the drop in estrogen levels occurs sooner during a person’s lifespan, and the associated increased risk of several chronic conditions lasts for a longer period of time.
Both premature and early are linked to elevated risks of CVD, specifically heart failure and atrial fibrillation (a type of abnormal heart rhythm that increases the risk of stroke).
Here’s what the research shows:
- A study of more than 1.4 million women found the younger the age at menopause, the higher the risk of heart failure and atrial fibrillation.
- Premature menopause, which affects about 1% of women, is also linked to a 5x higher stroke risk.

Black Women and Menopause: Why Symptoms Can Be Longer and More Severe
As a Black woman, menopause symptoms, including hot flashes, can be longer and more severe. Learn why and what you can do.

15 Causes Of Premature Or Early Menopause: Could It Happen To You?
Premature is when menopause happens before age 40 and early menopause is after age 40 but before age 45. Learn about the causes of premature and early menopause and why it matters for your health.

When Menopause Happens “Overnight”: What Are Premature And Early Menopause?
Learn what premature and early menopause are and why your age matters for your health and symptom severity.

12. High blood pressure during pregnancy
When you hit menopause, you may think you’ve said goodbye to your reproductive years, but if you have been pregnant in the past, events during your pregnancy can also impact you during menopause.
Gestational hypertension — defined as high blood pressure that first occurs after 20 weeks of pregnancy — is linked to an increased risk of heart disease later in life.
High blood pressure disorders during pregnancy increase the likelihood of severe menopause symptoms like hot flashes and night sweats. In turn, those symptoms may impact your risk of CVD.
If you’ve been pregnant before, think back to your experiences during pregnancy to assess whether they might be affecting both your menopause symptoms and cardiovascular risks now and discuss with your healthcare practitioner.
13. Hysterectomy
After Cesarean section, hysterectomy is the most common surgery performed in women in the US.
A 2023 study found hysterectomy performed in women+ younger than age 50 were at increased risk of CVD. The incidence of stroke was also significantly higher.
Typically, the removal of the ovaries during a hysterectomy leads to the immediate onset of menopause and, therefore the loss of heart-protective estrogen levels. However, in the study, the increased risk of CVD was present even in those whose ovaries were preserved, suggesting something related to the uterus itself is also heart-protective.
14. Hormone therapy (HT)
Hormone therapy (HT) can help relieve symptoms, like hot flashes. But there are risks to using it. Many of the HT risks you’ve probably heard about are connected to breast cancer, but there are heart disease concerns too.
Even though HT usually includes estrogen, it doesn’t necessarily provide the same heart-protective benefits as estrogen that’s naturally found in the body.
If you take estrogen hormone pills to relieve symptoms, you may be more likely to develop high blood pressure than women+ using other forms of the medication, according to new research.
Why? Estrogen ingested orally must be processed first through the liver and is associated with factors that can raise blood pressure.
How can you minimize this risk?
Talk to your doctor about other forms of HT which pose fewer cardiovascular risks. For example, low-dose, non-oral estrogen, like estradiol in transdermal or vaginal forms, poses a lower risk of hypertension. If you have additional risk factors or a family history of CVD, exploring these alternative options becomes even more important.
Consider HT in the early stages of menopause. Research has found that starting menopausal hormone therapy early in the menopause journey in women+ with menopausal symptoms may have cardiovascular benefits—though not in the late stages, according to the 2020 AHA scientific statement. The latest position statement from The Menopause Society also indicates that CVD events happen less often in younger women taking HT.
It is important to note that taking HT solely as a preventive measure (rather than for symptoms) is not indicated.

15. Where you live
Did you know that where you live could impact your risk of CVD?
A Mayo Clinic study found the prevalence of coronary heart disease (CAD) and stroke to be highest in the southern U.S., and the best cardiovascular health index (CVHI) scores were seen in the West. (The CVHI considers 7 cardiovascular health parameters – blood pressure, blood glucose, cholesterol, body-mass index, physical activity, healthy diet, and smoking behavior.)
As you can see, the 7 factors are, thankfully, all health parameters and:
- are ones over which you have a significant degree of control.
- include many that a healthy lifestyle, which is helpful to pursue during the menopause journey to manage symptoms better, will help address.
- are ones for which taking action will reduce the risk of conditions like diabetes, cancer, and cardiovascular disease (all of which figure more prominently during the hormonal transition and the years beyond)
In the study, geographic locations where the population experiences higher degrees of insecurity – financial, housing, and food – had greater rates of heart disease.
16. Race | Ethnicity
Race is another risk factor for CVD. Women+ of color (WOC+) are more at risk for both CVD and their complications from heart disease than those who are white. In general, WOC+ are also at a greater risk of conditions which can contribute to the development of CVD, such as hypertension and diabetes. Some factors thought to be root causes of this disparity include exposure to racism/bias/discrimination and social determinants of health (SDOH), like socioeconomic status, environmental exposures, and degree of difficulty in living a healthy lifestyle.
Possible reasons include:
- higher blood sugar levels
- higher cholesterol levels
- greater likelihood of experiencing:
- lack of access to healthcare
- environment – limited green space, safe walking areas
- food deserts and less access to quality grocery stores
The last two factors can make maintaining a heart-healthy diet and regular physical activity much more difficult to accomplish.
And of course, the experience of racial discrimination in and of itself can also have detrimental health effects. For example, higher levels of perceived discrimination have been linked to elevated blood pressure.
Black women+
Black adults are diagnosed with more CVD risk factors such as hypertension and obesity than other racial groups.
They’re also dying at disproportionate rates, particularly at younger ages (35 – 64 years old). While white women+ are more likely to be diagnosed with CVD, they are less likely than those who are Black to die from it. This disparity points to the barriers to quality healthcare that women+ of color face more often.
African-American women in particular, have a higher prevalence of heart failure than any other intersection of race and sex in the country.
Hispanic women+/Latinas
Hispanic women+ of color also have a higher prevalence of heart failure than their white peers.
Native women+
Native women+ are 1.5 times more likely to be diagnosed with coronary artery disease (CAD).
Asian women+
While heart disease rates differ among Asian ethnicities, they are rising faster overall than rates among white adults. For example, Filipino Americans experienced the greatest increase in CVD, about twice as high as their white counterparts, during the study period from 2007-2018. The exception is among the Japanese, whose lower cardiovascular risks may be due to greater intake of traditional Japanese diets, which are more heart-healthy. Chinese people have been found to have the lowest prevalence of CVD.
For Hmong women+, an ethnic group primarily from mountainous areas in Laos, China, Vietnam, and Thailand, a first stroke tends to occur at a much younger age than their white counterparts, recent research has found. Additionally, intracerebral hemorrhage—a type of stroke that often causes fatal brain bleeding—was twice as common in Hmong adults compared to white patients.
Hawaiian and Pacific Islander women+
Non-Hawaiian Pacific Islanders have been found to have a greater rate of coronary artery disease than Native Hawaiians.

Black Women and Menopause: Why Symptoms Can Be Longer and More Severe
As a Black woman, menopause symptoms, including hot flashes, can be longer and more severe. Learn why and what you can do.

Embrace a Healthier You: A Native American/Alaska Native Woman’s Prescription for Health
Embrace a healthier you, with this prescription for health for Native/Alaska Native women. Know the health risks, disparities, and prevention steps to live healthier.

How To Live Healthier: A Latina/Hispanic Woman’s+ Prescription For Health
The menopause journey is the perfect time to make a change for the better. Learn about Latina/Hispanic woman’s health, and get a prescription for better health.
17. Risks for the LGBTQIA+ community
LGBTQIA+ individuals can also face unique risks for cardiovascular disease. According to a small study, sexual and gender minorities may have a higher risk for stroke at a younger age than their heterosexual counterparts – the average age for LGBTQIA+ patients was 55 compared to 69 for their heterosexual peers. Lesbian, gay, bisexual, transgender or non-binary individuals were also potentially more likely to have another stroke.
In addition to the elevated stress that comes with facing stigma and discrimination as risk factors, sexual and gender minority patients were also more likely to have HIV and a current or previous history of syphilis and hepatitis C as risk factors, contributing to inflammation and damage to blood vessels thereby increasing stroke risk.
Transgender-specific risks
In addition to the elevated stress that prejudice can cause, trans women undergoing gender-affirming hormone therapy have an increased risk for stroke, blood clots, and heart attacks.
The risks for stroke and blood clots were highest with estrogen pills, shots, or patches and lower in individuals who took medication such as spironolactone to reduce testosterone.
Additionally, chronic stress increases the risk of both hypertension, a risk factor for heart disease, and cardiovascular events. The stress of discrimination and transphobia has been linked to greater rates of heart disease in the transgender community.

Empowering LGBTQIA+ Health: Cancer Knowledge Is Power. Learn The Risks
We’re empowering LGBTQIA+ health with information on LGBTQIA+ cancer risks. There’s no better time to invest in your health than menopause.

Transgender Menopause: What to Expect
Transgender menopause can happen. Learn what to expect.

Menopause Pride: The LGBTQIA+ Experience And Where to Find Inclusive Doctors
Every menopause journey is unique. For LGBTQIA+ people there are positives and challenges, like health disparities. Learn how to have menopause pride by knowing what to expect.
18. Disabilities and heart health
In the U.S. approximately 42.5 million people are estimated to live with some form of disability (defined as persistent conditions of abnormal functioning that limit activities or restrict participation.) While not all disabilities are linked to an increased risk of cardiovascular conditions, physical disabilities are linked to the development of coronary heart disease.
In addition, disabilities caused by coronary heart disease are more likely to result in death than disabilities from other causes.
You can improve your heart health
Menopausal risks are just one part of CVD. Factors like your lifestyle and a family history of cardiovascular disease can also contribute to an increased risk.
These other factors include:
- smoking and second-hand smoke exposure
- sedentary lifestyle
- family history
- alcohol
- unhealthy eating – diet high in saturated fats, trans fat, and cholesterol
Talk to your doctor about your risk factors and consider a cardiovascular check-up. Watch the video below to learn more about the menopause journey and heart health.
Whatever risks factors you may have for heart disease, remember there are many ways to improve your cardiovascular health, reduce the risk of complications, and make a change for the better. Take action now.
The connection between menopause and cardiovascular disease risks | American Heart Association
Cushman M, Shay C, Howard V, Jiménez M, Lewey J, McSweeney J, Newby K, Poudel R, Reynolds H, Rexrode K, Sims M, Mosca L, and On behalf of the American Heart Association. Ten-Year Differences in Women’s Awareness Related to Coronary Heart Disease: Results of the 2019 American Heart Association National Survey: A Special Report From the American Heart Association. Circulation. 2021;143:e239–e248. doi/10.1161/CIR.0000000000000907
Symptoms of a Heart Attack in Women and Men | American Heart Association
Heart Attack Symptoms in Women | American Heart Association
The Connection Between Menopause and Cardiovascular Disease Risks | American Heart Association
Maas AH, Appelman YE. Gender differences in coronary heart disease. Neth Heart J. 2010 Dec;18(12):598-602. doi: 10.1007/s12471-010-0841-y. PMID: 21301622; PMCID: PMC3018605.
Armeni E, Augoulea A, Efstathiou A, Chatzivasileiou P, Kaparos G, Vlahos N, Eleftheriades M, Lambrinoudaki I. The severity of hot flashes is associated with the risk for incident metabolic syndrome and new-onset hypertension after the menopause. Endocrine Abstracts (2023) 90 OC4.6. DOI: 10.1530/endoabs.90.OC4.6
What to know about menopause and high blood pressure | Healthline Media
Kodoth V, Scaccia S, Aggarwal B. Adverse Changes in Body Composition During the Menopausal Transition and Relation to Cardiovascular Risk: A Contemporary Review. Womens Health Rep (New Rochelle). 2022 Jun 13;3(1):573-581. doi: 10.1089/whr.2021.0119. PMID: 35814604; PMCID: PMC9258798.
The Reality of Menopause Weight Gain | Mayo Clinic
Lee, Sae Rom MD; Cho, Young Hye MD; Park, Eun Ju MD; Lee, Youngin MD; In Choi, Jung MD; Kwon, Ryuk-Jun MD, PhD; Son, Soo Min MD; Lee, Sang Yeoup MD, PhD. The association between reproductive period and handgrip strength in postmenopausal women: a nationwide cross-sectional study. Menopause ():10.1097/GME.0000000000002283, November 28, 2023. | DOI: 10.1097/GME.0000000000002283
Abnormal Cholesterol (Dyslipidemia) | Stanford Medicine
What is Cholesterol? | American Heart Association
Mesalić L, Tupković E, Kendić S, Balić D. Correlation between hormonal and lipid status in women in menopause. Bosn J Basic Med Sci. 2008 May;8(2):188-92. doi: 10.17305/bjbms.2008.2980. PMID: 18498273; PMCID: PMC5698353.
Take control of rising cholesterol at menopause | The Presidents and Fellows of Harvard College
The reality of menopause weight gain | Mayo Clinic
Kodoth V, Scaccia S, Aggarwal B. Adverse Changes in Body Composition During the Menopausal Transition and Relation to Cardiovascular Risk: A Contemporary Review. Womens Health Rep (New Rochelle). 2022 Jun 13;3(1):573-581. doi: 10.1089/whr.2021.0119. PMID: 35814604; PMCID: PMC9258798.
Diabetes and Your Heart | Centers for Disease Control and Prevention
Extra Weight, Extra Risk | American Diabetes Association
Polycystic Ovary Syndrome (PCOS) | Johns Hopkins Medicine
Scicchitano P, Dentamaro I, Carbonara R, Bulzis G, Dachille A, Caputo P, Riccardi R, Locorotondo M, Mandurino C, Matteo Ciccone M. Cardiovascular Risk in Women With PCOS. Int J Endocrinol Metab. 2012 Fall;10(4):611-8. doi: 10.5812/ijem.4020. Epub 2012 Sep 30. PMID: 23843832; PMCID: PMC3693634.
Polycystic Ovarian Syndrome: How Your Ovaries Can Affect Your Heart | Johns Hopkins Medicine
Insomnia | Cleveland Clinic
Sleep Disorders and Heart Health | American Heart Association
Sleep Difficulties in Adults: United States, 2020 | Centers for Disease Control and Prevention
CVD, stroke risk increase with number of menopause symptoms | Healio
Premature menopause is associated with increased risk of heart problems | European Society of Cardiology
Women experiencing severe hot flashes after menopause more likely to develop metabolic syndrome | AZoNetwork
Choi, Hye Rin MPH, PhD; Chang, Yoosoo MD, PhD; Kim, Yejin MPH; Cho, Yoosun MD, PhD; Kwon, Min-Jung MD, PhD; Kang, Jeonggyu MD; Kwon, Ria MPH, PhD; Lim, Ga-Young PhD; Kim, Kye-Hyun MD, PhD; Kim, Hoon MD, PhD, NCMP; Hong, Yun Soo MD, PhD; Park, Jihwan MHS; Zhao, Di PhD; Cho, Juhee PhD; Guallar, Eliseo MD, DrPH; Park, Hyun-Young MD, PhD; Ryu, Seungho MD, PhD. Vasomotor and other menopause symptoms and the prevalence of ideal cardiovascular health metrics among premenopausal stage women. Menopause 30(7):p 750-757, July 2023. | DOI: 10.1097/GME.0000000000002203
Menopause before 40 tied to higher stroke risk | American Heart Association
A New Reason to Watch Your Blood Pressure During Pregnancy | HealthCentral
Hypertension: Everything You Need to Know | HealthCentral
Faubion SS, King A, Kattah AG, Kuhle CL, Sood R, Kling JM, Mara KC, Kapoor E. Hypertensive disorders of pregnancy and menopausal symptoms: a cross-sectional study from the data registry on experiences of aging, menopause, and sexuality. Menopause. 2020 Aug 17;28(1):25-31. doi: 10.1097/GME.0000000000001638. PMID: 32810078; PMCID: PMC7769885.
Hysterectomy | Cleveland Clinic
Yuk J, Kim BG, Lee BK, et al. Association of Early Hysterectomy With Risk of Cardiovascular Disease in Korean Women. JAMA Netw Open. 2023;6(6):e2317145. doi:10.1001/jamanetworkopen.2023.17145
Oral estrogen therapy for menopause may increase high blood pressure risk | American Heart Association
El Khoudary S, Aggarwal B, Beckie T, Hodis H, Johnson A, Langer R, Limacher M, Manson J, Stefanick M, Allison M and On behalf of the American Heart Association Prevention Science Committee of the Council on Epidemiology and Prevention; and Council on Cardiovascular and Stroke Nursing. Menopause Transition and Cardiovascular Disease Risk: Implications for Timing of Early Prevention: A Scientific Statement From the American Heart Association. Circulation. 2020;142:e506–e532 https://doi.org/10.1161/CIR.0000000000000912
Parcha V, Kalra R, Suri SS, Malla G, Wang TJ, Arora G, Arora P. Geographic Variation in Cardiovascular Health Among American Adults. Mayo Clin Proc. 2021 Jul;96(7):1770-1781. doi: 10.1016/j.mayocp.2020.12.034. Epub 2021 Mar 26. PMID: 33775420; PMCID: PMC8260439.
Cardiovascular disease and race: Causes | Healthline Media
Powell-Wiley T, Baumer Y, Osei Baah F, Baez A, Farmer N, Mahlobo C, Pita M, Potharaju K, Tamura K, Wallen G. Social Determinants of Cardiovascular Disease. Circulation Research. 2022;130:782–799 https://doi.org/10.1161/CIRCRESAHA.121.319811
Dolezsar CM, McGrath JJ, Herzig AJM, Miller SB. Perceived racial discrimination and hypertension: a comprehensive systematic review. Health Psychol. 2014 Jan;33(1):20-34. doi: 10.1037/a0033718. PMID: 24417692; PMCID: PMC5756074.
Javed Z, Haisum Maqsood M, Yahya T, Amin Z, Acquah I, Valero-Elizondo J, Andrieni J, Dubey P, Jackson R, Daffin M, Cainzos-Achirica M, Hyder A, and Nasir K. Race, Racism, and Cardiovascular Health: Applying a Social Determinants of Health Framework to Racial/Ethnic Disparities in Cardiovascular Disease. Circulation: Cardiovascular Quality and Outcomes. 2022;15 https://doi.org/10.1161/CIRCOUTCOMES.121.007917
Breathett K. Latest Evidence on Racial Inequities and Biases in Advanced Heart Failure. 2020. American College of Cardiology.
Study of heart disease trends reflects diversity among Asian Americans | American Heart Association
Waitzfelder B, Palaniappan L, Varga A. et al. Prevalence of cardiovascular disease among Asian, Pacific Islander and multi-race populations in Hawai’i and California. BMC Public Health 23, 885 (2023). https://doi.org/10.1186/s12889-023-15795-5
Hussein H, Kashyap B, O’Keefe L, Droegemueller C, Othman S, Kau Yang M, Hanson L. Stroke Characteristics in a Cohort of Hmong American Patients. Journal of the American Heart Association. 2023;12:e026763 https://doi.org/10.1161/JAHA.122.026763
Diaz M A, Rosendale N. Exploring Stroke Risk Factors and Outcomes in Sexual and Gender Minority People. Neurol Clin Pract Feb 2023, 13 (1) e200106; DOI: 10.1212/CPJ.0000000000200106
Women’s unique risk factors | Heart & Stroke Foundation of Canada
You may also like…

How Menopause Impacts Heart Health: 7 Action Steps That Help
Heart health lifestyle habits can help you manage menopause symptoms and help reduce the risk of cardiovascular disease.

Women Are Skipping Preventive Care Even Though It Helps Healthy Aging
Are you up to date on your mammogram and other preventive care screenings and exams? Don’t skip them, as they can help with healthy aging.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

