Do you have long COVID, or suspect you do? It can affect anyone who had a COVID-19 infection, reinfection, or breakthrough infection. Women are more likely to get it than men, underscoring how important it is for women to prioritize their health. Knowledge is power! Learn about the latest research, studies, and treatment options so you can be better prepared to get the help you need and deserve should long COVID become a part of your life.
What is long COVID?
Long COVID is typically defined as ongoing symptoms of COVID-19 that continue for more than 12 weeks and are not explained by an alternative diagnosis.
Like most things related to COVID-19, there is not 100% agreement, and some in the medical and scientific community use a 4-week timeframe while others make a long COVID diagnosis at 2 months post-infection.
There’s also no agreement on what it’s called. The Centers for Disease Control (CDC), World Health Organization (WHO), and National Institute of Health (NIH) refer to this condition differently. You may hear long COVID referred to as:
- long hauler syndrome (used by NIH)
- PASC – post-acute sequelae of SARS CoV-2 infection (used by NIH)
- post-COVID condition (used by CDC and WHO)
Those struggling with lingering COVID symptoms, tend to prefer the phrase, long COVID. No matter the term, it can be devastating.
10-30% of people who get COVID,
How many people have it?
The CDC estimates that in the U.S., 20% of those who had a COVID-19 infection are currently experiencing long COVID. The impact can be more or less, with averages between 10-30% of people infected who go on to develop long COVID.
That’s at least 25 – 30 million people and includes 7.5% of the overall adult population.
A Brookings Institute report in August 2022 estimated that 4 million adults were unable to work due to long COVID symptoms.
While many studies to date haven’t analyzed data according to sex, trends are emerging that show women are more likely to get long COVID than men. Why is this the case? It’s unclear, but trends are emerging in studies.
Researchers at Johnson & Johnson reviewed academic papers on individuals who had COVID from December 2019-August 2020 and studies on long COVID published between January 2020 and June 2020. They found women tended to mount a more robust immune response to COVID, which could result in an autoimmune pathway to long COVID.
Hormones may also be to blame, which you can learn more about in the section on why long COVID impacts more women and the section on how it also increases the chance of medical gaslighting for women.
Long COVID symptoms
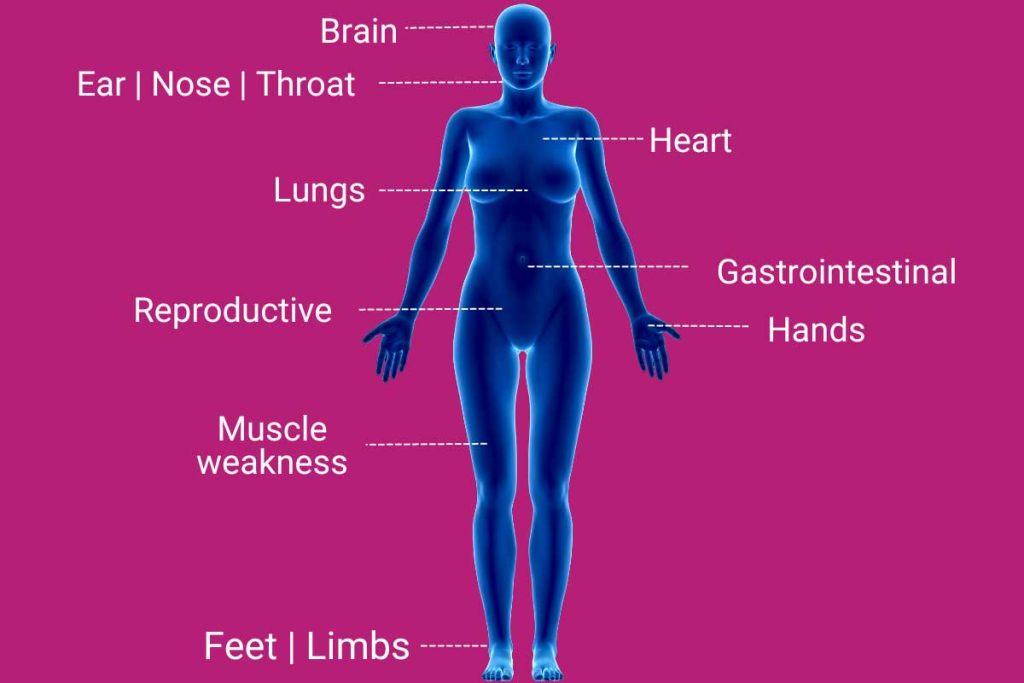
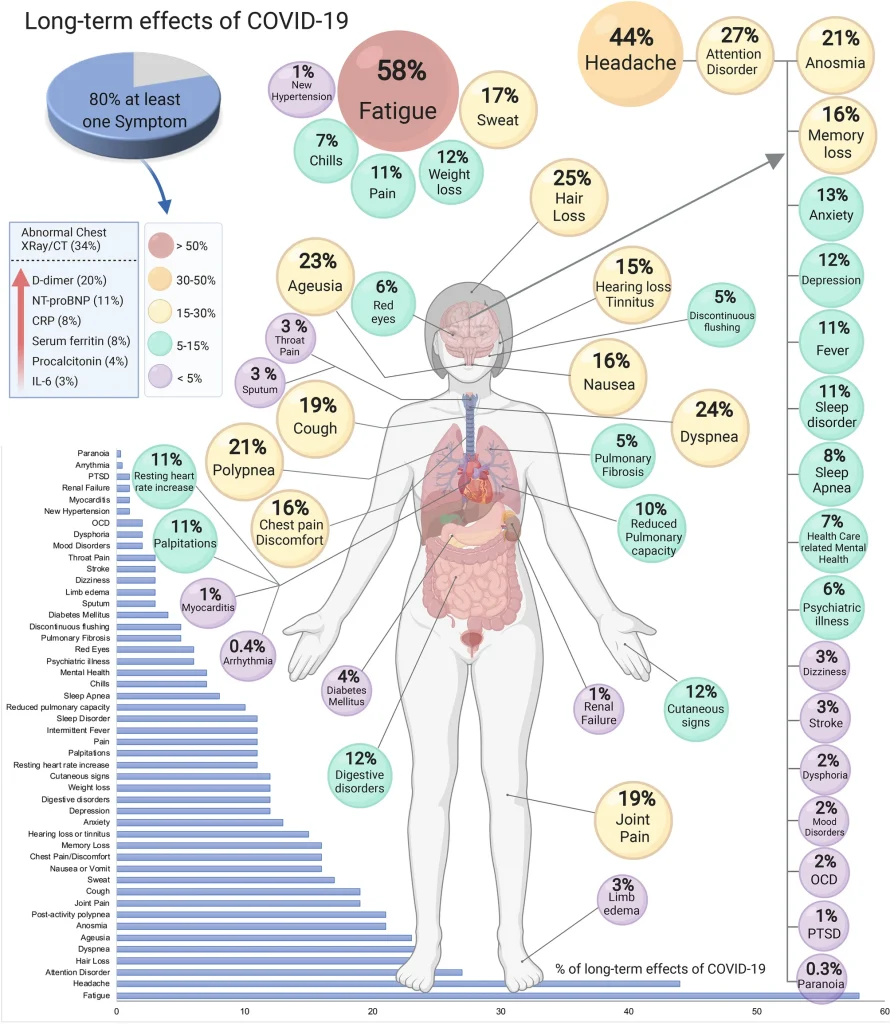
COVID-19 can impact the entire body and every organ system. Therefore, a wide range of symptoms has been reported.
You can experience symptoms from your head to your toes.
Some more commonly experienced symptoms are fatigue, headache, loss of smell and taste, sleeplessness, brain fog, joint pain, cough, shortness of breath, and hair loss. Some of these symptoms mirror menopause symptoms like brain fog, sleeplessness, joint pain, and hair loss which can exacerbate symptoms for women or lead to more confusion.
Long COVID symptoms may include:
Brain
- Forgetfulness
- Headache
- Depression
- Anxiety
- Delirium
- PTSD | OCD
- Sleep disturbance
- Brain fog
Ears | Nose | Throat | Eyes
- Loss of taste and/or smell
- Parosmia (noxious smells)
- Vertigo | Balance issues
- Tinnitus
- Sore throat
- Hoarse voice
- Earache
- Nasal congestion
- Hearing loss
- Visual impairment
Lungs
- Shortness of breath
- Persistent cough
- Persistent need for oxygen
Heart
- Heart palpitations
- Arrhythmia
- Chest pain or pressure
- Increased heart rate
- Heart failure
- Myocarditis
- Pericarditis
Gastrointestinal
- Nausea or vomiting
- Diarrhea
- Abdominal pain
Sexual Reproductive
- Changes in your menstrual period
Hands | Feet | Limbs
- COVID toes
- Neuropathy (pins and needles)
Generalized
- Extreme fatigue
- Exercise intolerance
- Rashes
- Body aches
- Fever
- Poor appetite
- Weight loss
- Hair loss
- “Internal tremors” and vibrations
- Blood clots
- Joint pain
- Muscle weakness
Symptoms may vary depending on the severity of the infection and if hospitalization was required, and the variant involved.
For example, the Alpha variant has been associated with brain fog, muscle aches and pain, insomnia, loss of smell, impaired hearing, problems with swallowing, and anxiety/depression.
Also, the symptoms of long COVID may be different than or additional to those experienced at the time of symptomatic infection.
Symptom clusters
Sometimes, these symptoms appear in clusters, so if you have one symptom, you may be more likely to have others in that grouping.
In a pre-print study of 1459 patients published in medRxiv in July 2022, researchers at King’s College London reported the identification of 3 distinct symptom clusters that were seen in the population:
- Group 1 – chest pain and severe shortness of breath; seen in those with infection by the “original” version (aka the “wild type”) of COVID-19
- Group 2 – fatigue, brain fog, and headaches; seen in those with infections by Alpha and Delta variants
- Group 3 – a diverse range of physical symptoms, including heart palpitations, muscle aches and pain, changes to their skin and hair, and most severe and debilitating multi-organ system symptoms
Another study published in July 2022 in Nature mapped symptoms and risk factors in non-hospitalized patients. The study analyzed data from a UK database of close to 500,000 patients.
62 symptoms were highly correlated with long COVID, using a definition of symptoms occurring three months from the onset of acute COVID-19 symptoms, lasting for at least two months, and which could not be explained by an alternative diagnosis.
The Nature study also reported an observation of 3 symptom clusters (which differ from the clusters noted in the medRxiv study):
- Group 1 – pain, fatigue, and rash (more likely to be seen in Asian or other ethnic minority groups)
- Group 2 – shortness of breath, cough, and phlegm (more likely to be seen in white patients)
- Group 3 – depression, anxiety, insomnia, and brain fog (more likely to be seen in white and younger patients)
Regardless of the group, patients were more likely to be female and have a low socioeconomic status.
It’s important to note how this study observed differences in white individuals, Asians, and other ethnic minority groups.
We also see this with menopause, where experiences vary for women of color and women around the world.
Long COVID and exercise
Long COVID symptoms can make daily activities difficult, especially healthy lifestyle habits like exercise.
Post-Exertional Symptom Exacerbation (PESE) is a condition seen in long COVID patients, characterized by disabling fatigue and exhaustion out of proportion to the effort expended.
It is most commonly triggered by physical activity or exercise but can also be seen after cognitive exertion.
Symptoms include:
- cognitive dysfunction/brain fog
- shortness of breath
- exercise intolerance
- sleep disturbance
- palpitations
- fever
They typically worsen 12 to 48 hours after activity and can last for days to months.
According to researchers, fatigue is one of the most frequent symptoms, followed by headaches.
Long COVID and cortisol
An August pre-print study found that long COVID patients had a cortisol level close to 50% below normal. Cortisol is the body’s main stress hormone secreted by the adrenal glands. It helps the body control inflammation, regulate blood pressure and blood glucose levels, sleep cycles, and the processing of protein/fat/carbohydrates. It also aids in boosting energy levels when under stress.
Long COVID and POTS
Knowing that more women tend to get long COVID, it’s not surprising that some symptoms of long COVID also have striking similarities to conditions like Postural Orthostatic Tachycardia Syndrome (POTS), which affects more women than men. It’s a disorder of the autonomic nervous system in which patients experience certain symptoms when standing upright, accompanied by a significant increase in heart rate.
The autonomic nervous system is a component of the peripheral nervous system that regulates involuntary physiologic processes, including heart rate, blood pressure, respiration, digestion, and sexual arousal.
85% of the those with the condition are female, but it can also affect men and children. Up to 3 million people in the U.S. have POTS.
Common symptoms include lightheadedness, fainting, “brain fog,” palpitations, severe fatigue, nausea and vomiting, exercise intolerance, and headache. Many of these symptoms are experienced by those with long COVID.
The cause of POTS is unclear, but its onset is often preceded by a viral infection.
Diagnosis typically involves blood tests and either a 10-minute standing test or tilt table test. Treatment may include dietary modifications, medications, and physical therapy.
Long COVID and ME/CFS
There are also symptom similarities to ME/CFS, which can impact up to 4 times more women than men. It’s typically seen in young to middle-aged adults.
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) is a condition of unknown cause in which patients experience extreme fatigue after physical or mental exercise that is unexplained by an underlying condition, has lasted at least 6 months, does not improve with rest, and is accompanied by at least 4 of the following additional symptoms:
- impaired short-term memory and concentration
- odynophagia (pain with swallowing)
- tender lymph nodes in the neck or underarms
- muscle pain
- joint pain with no signs of inflammation
- headache
- sleep that does not refresh
- exhaustion lasting more than 24h after exercise
- dizziness that worsens when moving from a lying position to sitting or moving from sitting to standing
Treatment may include dietary supplements, medications, herbal preparations, and low-intensity aerobic exercise.

Who gets long COVID?
Both children and adults can get long COVID.
At this point, most studies have shown women to be more likely to develop long COVID than men (up to two times in some studies).
Of particular note, long COVID can develop in individuals with no symptoms at the time of infection (and may never have even known they were infected). It can also be seen in previously healthy people with no underlying conditions.
Long COVID risk factors
There is variability from study to study as to the factors which increase the risk of developing long COVID.
Risk-factor profiles have also evolved, with new additions as more information becomes available. For example, the increased risk factor for women emerged in 2021.
2020
- Severe symptoms at the time of infection
- Infection severe enough to require hospitalization
- Preexisting medical conditions
2021
- Female sex
- Shortness of breath and chest pain at the time of infection
- Older age
- Preexisting mental health disorder
- Persistent elevated inflammatory markers on blood tests
2022
- Need for high-flow oxygen
- Presence of certain autoantibodies (antibodies against your body’s own cells)
- High viral load early in the course of infection
- Type 2 diabetes
- Reactivation of Ebstein-Barr virus (the virus that causes mononucleosis)
- Infection severe enough to require immunosuppressant medication
- Infection severe enough to require ICU admission
- Obesity
- Communities of color
- Low socioeconomic status
- Smoking/former smoking status
- Younger age
- People who experience multisystem inflammatory syndrome (MIS) during or after COVID-19 illness
- Being unvaccinated
In June 2022, the CDC reported the following additional patterns in those currently suffering from long COVID:
- Older adults were less likely than those who are younger to suffer from long COVID. For example, almost three times as many adults age 50 – 59 currently have long COVID than those aged 80 and older.
- Race/ethnicity may potentially play a yet-to-be-identified role. Long COVID was seen more often in Hispanic adults than non-Hispanic white adults. It was found more frequently in non-Hispanic adults than Black adults. And was seen the least in Asian adults.
- Gender identity and sexual orientation may also play a yet-to-be-identified role. Bisexual and transgender adults were more likely to have current long COVID symptoms than adults of other sexual orientations and gender identities.
- Geography also impacted prevalence, with the highest percentage of adults with long COVID symptoms in Kentucky, Alabama, Tennessee, and South Dakota. The states with the lowest percentage of long COVID cases include Hawaii, Maryland, and Virginia.
Reviewing these risk factors, several are present more commonly in women than men – lower socioeconomic status, obesity, mental health conditions, and preexisting chronic conditions.
Long COVID variant risk – Delta and Omicron
Thus far, long COVID is seen more commonly in those infected with the Delta variant and appears less common in those who have experienced an infection with Omicron. The Delta variant was first seen in the U.S. during the summer of 2021, and the Omicron variant first surfaced in November 2021.
The risk varied in triple-vaccinated individuals depending on the subvariant of the Omicron variant in a July 2022 study of UK National Health Service (NHS) data of patients who self-reported symptoms of long COVID from May 2021 through May 2022.
Those with BA.2 were more likely than those infected with BA.1.
Vaccines and long COVID
You can still get long COVID even if you’re vaccinated.
However, vaccination has been noted to reduce the risk of developing long COVID up to 50%.
A mixed picture has been observed regarding the impact of COVID-19 vaccination in those who already suffer from long COVID – one-third of patients experience a reduction in symptoms, one-third no change in symptoms, and one-third a worsening of symptoms.
For those who see improvement, there are several theories regarding how vaccination and boosting may help:
- helps the immune system fight off the lingering virus and clear its residual
- aborts a harmful immune response
- resets the immune system
An Italian study published in JAMA in July 2022 of 2560 healthcare workers who had had a COVID-19 infection but did not require hospitalization indicated that those vaccinated were less likely than the unvaccinated to develop long COVID. And those who had 3 doses of vaccine were less likely than those with 2 doses, who were less likely than those with a single dose.
Women and long COVID
Multiple studies have indicated that women are more likely to develop long COVID than men.
Having a COVID-19 infection is a requirement for the development of long COVID, and women are more likely to be infected by COVID-19.
An Italian study published in the Journal of Women’s Health in March 2022 of a mixed group of 223 outpatient and hospitalized patients found:
- Women were more likely to have intense symptoms than men during the acute phase of infection and more likely to report palpitations, muscle aches, diarrhea, loss of taste and smell, chest pain, asthenia (abnormal physical weakness or lack of energy), palpitations, sleep issues, and myalgia.
A UK study of 2320 patients who had not been hospitalized due to a COVID-19 infection was published in The Lancet in April 2022. Only 28.9% of study participants reported a full recovery at one year.
Persistent symptoms at one year included fatigue, symptoms consistent with “brain fog,” shortness of breath, poor sleep, joint and muscle pain, joint swelling, and limb weakness.
Women were 33% less likely to make a full recovery after infection. Plus, it can affect a woman’s health including her menstrual cycle, thyroid, and menopause experience.
Researchers at Johnson & Johnson pointed out in a review of academic papers published in Current Medical Research and Opinion (June 2022) that most studies to date often do not provide an analysis that includes a sex breakout.
Even still, in their review of academic papers on COVID from December 2019 and August 2020 and studies on long COVID published between January 2020 and June 2021, the differences in COVID for women were highlighted in the Johnson & Johnson findings.
Their findings include:
- Women’s symptoms tended to be more pronounced.
- Women tended to mount a more robust immune response to infection (which could then result in an autoimmune pathway to long COVID).
- Women were more likely to have fatigue, ear, nose, and throat problems, mood disorders, GI symptoms, neurological and rheumatologic symptoms, and skin issues. (Men were significantly more likely to experience disorders such as diabetes and kidney disease.)
Researchers at the Institute for Health Metrics and Evaluation (IHME) at the University of Washington’s School of Medicine also found 63% of long COVID patients worldwide during the first two years of the pandemic were women. Additionally, almost 10% of women older than 20 who had a symptomatic COVID infection, but did not require hospitalization, developed persistent symptoms vs. 5% of men.
Why are women at greater risk of long COVID?
Several potential factors under active investigation could explain the greater prevalence in women. Among them is a hormonal imbalance.
A COVID-19 infection can impact the ovaries and significantly reduce estrogen (and, to a lesser extent, testosterone) levels. The virus can enter the ovaries by binding to certain receptors known as angiotensin-converting enzyme 2 (ACE2) receptors. (A receptor is “molecule (such as a protein) on the cell surface or in the cell interior that has an affinity for a specific chemical group, molecule, or virus.”)
This hormonal disruption can impact the body’s inflammatory response.
Long COVID has also been found to impact menstruation as well as the menopause journey.
- In women with long COVID, changes in their periods (flow, frequency, duration) have been noted.
- In perimenopausal women, a worsening of long COVID symptoms has been observed in the days prior to the start of a period.
- For women on the menopause journey, those with long COVID have been found to suffer more severe symptoms and potentially a more acute onset of perimenopausal symptoms and the onset of menopause.
Interestingly, similarities have been seen between some long COVID symptoms and several of those experienced during the menopause journey symptoms, e.g., brain fog, sleep issues, fatigue, and emotional distress, which can make an assessment of each potential scenario more complicated and challenging. And it can sometimes make it difficult to identify the root cause of the symptoms, i.e., is it long COVID or menopause-related or both?
HT (hormone therapy) may potentially help mitigate the impact of long COVID in women taking it for perimenopausal symptoms. Its use is still being studied in this context.
Potential causes of long COVID
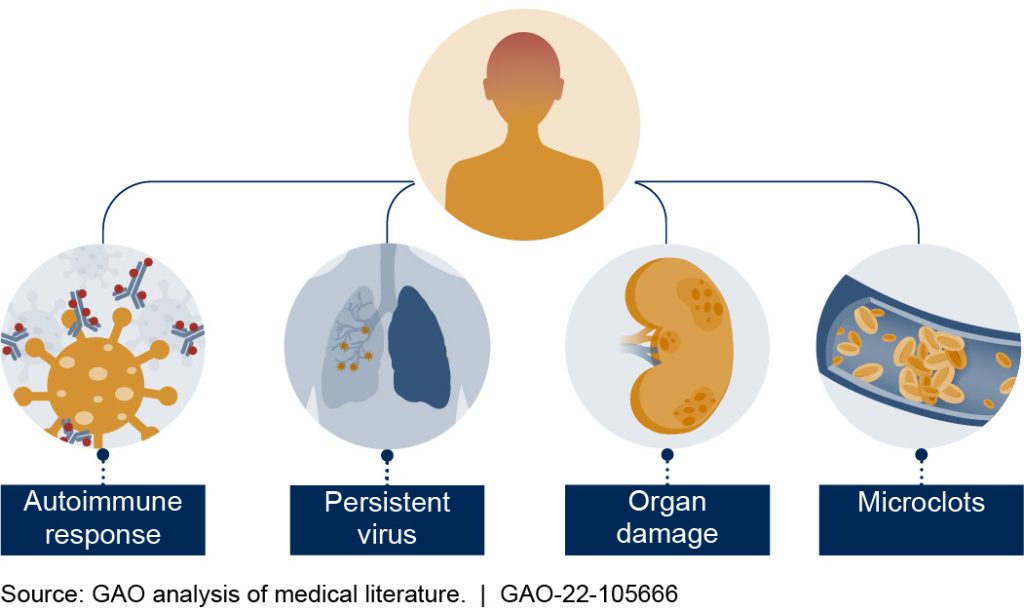
There are currently five different theories regarding the cause of long COVID, as reported by a GAO (Government Accountability Office) analysis of the medical literature. It may be the case that each is correct and applicable, depending on factors yet to be identified, with different causes manifest in different people and some people potentially suffering from more than one cause.
It’s thought in some patients the body produces an antibody that mimics COVID, so your body creates an autoimmune response. As a result, the immune system attacks its own cells.
For others, the virus may linger. You may wonder if you’re still contagious.
Although the virus may still be present in the body, current indications are that the period of being able to transmit this long-lingering virus (vs. a new infection) to someone else is well past by the time a diagnosis of long COVID would come into consideration.
Organ damage may also be to blame for why symptoms continue long after infection.
Also, microclots may form in blood vessels. They disrupt regular blood flow and cause tissue damage.
Finally, and not represented in the graphic, there are also reports that COVID-19 may reactivate the Epstein-Barr virus (the virus that causes mononucleosis).
How long is long?
The reported duration of symptoms varies from study to study and symptom to symptom.
For example, those who experienced a loss of taste or smell often have symptom resolution within a year, and close to 90% have returned to baseline by Year 2.
Other symptoms may resolve in a few months.
On the other hand, if there has been severe organ damage, e.g., scarring of heart or lungs, the duration could potentially extend a lifetime.
Differences have also been noted depending on geographic locale and symptom severity, or lack thereof, at the time of infection. Duration typically follows this pattern: severe > moderate > mild > no symptoms.
However, in others, illness severity has not appeared to impact how long someone has long COVID.
A mixed picture has also been seen regarding sex in yet other studies.
Symptom severity
In a presentation in March 2022 by Theo Vos during a NAM Workshop, “Long-Term Effects Stemming from COVID-19 and Implications for the Social Security Administration,” the probability of ongoing symptoms were mapped by three factors – sex, children (defined as age < 20) vs. adults, and time period since the end of the acute episode – 3, 6, and 12 months.
The findings indicated:
- The probability of ongoing symptoms fell over time and at 12 months ranged from 0.26% in a community setting to 25.37% in ICU patients. The probability was greatest for those who had been admitted to the ICU, followed by those who were hospitalized but did not require ICU care, followed by those whose care was provided in an outpatient setting.
- The probability was less for children than adults.
- The probability was greater for female patients than those who were male.
Impact of hospitalization
A study conducted in China was published in May 2022 in The Lancet Respiratory Medicine of 1192 patients who had been hospitalized due to COVID-19 infection. Approximately 50% had long COVID symptoms 2 years later.
Fatigue was the most frequently reported symptom, but patients also commonly experienced trouble with sleep and muscle weakness throughout the 2-year follow-up, regardless of disease severity. Pain/discomfort, anxiety, depression, and problems with mobility were the most common symptoms at Year 2. Those who had been critically ill were more likely to have lung impairment.
Patients experienced continued improvement over the 2-year period relative to mental health and exercise capacity, independent of the degree of disease severity at the time of initial infection.
89% of patients who had been working before COVID-19 had returned to work by 2 years out.
Taste and smell
A study of 168 patients with mild COVID-19 infection conducted in Italy and the UK and published in August 2022 in JAMA Otolaryngology–Head & Neck Surgery looked at the duration of the symptom of dysfunction of taste and/or smell. Approximately 64% experienced such symptoms at the time of infection at a point in time prior to the arrival of the Omicron variant.
Two years later, 88.2% reported complete resolution of smell/taste dysfunction, and only 2.5% indicated the symptom being either the same or worse than at the time of initial onset.
The most common symptoms unrelated to taste or smell that persisted at 2 years were fatigue and shortness of breath.
Review of COVID cases from Jan. 2020-April 2022
Another study of the health records of almost 1.3 million people (mainly in the U.S.) who had a diagnosis of COVID-19 in the timeframe between January 2020 and April 2022 was published in The Lancet in August 2022 by researchers at the University of London and found:
- increased risk of brain fog, dementia, psychotic disorders, and epilepsy (seizure disorder) at 2 years in adults who had had COVID
- increased risk of depression and anxiety within the first 6 months post-infection
- Children had an increased risk of cognitive deficit, insomnia, stroke due to a brain bleed or blood clot, epilepsy, nerve/nerve root/nerve plexus disorders, and psychotic disorders at 6 months.
- The risk of any new-onset neurologic or psychiatric diagnosis was higher among people ≥ age 65 (and many experienced a higher mortality rate, particularly if they suffered from epilepsy or dementia).
Long COVID treatment
With no cause(s) yet definitively determined, no long COVID-specific treatment is yet available. However, there are established protocols and guidelines, and at least one medication is being studied that appears to be promising.
At this time, the major focus is on symptom relief, as researchers look for answers and some patients experience improvement with the tincture of time.
However, there are treatment guidelines and regimens, which have grown in number as more has been learned about the condition.
Below are some of the current long COVID treatment protocols and guidelines:
- American College of Cardiology (ACC) March 15, 2022: ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19: Myocarditis, Post-Acute Sequelae of SARS-CoV-2 Infection (PASC) and Return to Play Journal of the American College of Cardiology
- Physical Medicine and Rehabilitation (AAPM&R)
- NIH
- NICE: COVID-19 rapid guideline: managing the long-term effects of COVID-19
- Summary of Joint (NICE, SIGN, Royal College of General Practitioners) Guideline on the Management of Long COVID
- Post COVID-19 Condition: Guidance for Primary Care (in Canada)
- ESCMID rapid guidelines for assessment and management of long COVID
- APA: Treating Patients with Long COVID
- OHSU: Clinical Guidelines – Long COVID-19
- Key learning points: updated NICE guidance on managing long COVID
- COVID-19 rapid guideline: managing COVID-19
- LONG COVID PHYSIO
Several protocols are being tested for effectiveness and the sustainability of symptom relief. Some of the approaches taken may replicate the type of treatment that is helpful in those who suffer from other conditions but do not cure long COVID. Some of these approaches include:
- Medication – antidepressants (depression and anxiety, sleep issues, and headaches), anti-seizure medication (pain, numbness, muscle aches), drugs to treat low blood pressure (POTS-like symptoms)
- Melatonin supplement – sleep issues
- Pulmonary rehabilitation – to improve shortness of breath and exercise tolerance
- Cognitive rehabilitation – to help symptoms of brain fog
- Autonomic conditioning – to help improve symptoms like dizziness and palpitations
- Olfactory (smell) training – to help with loss of smell and taste
There is also research underway to determine if pre-existing medications for other conditions might work for patients with long COVID. Naltrexone, a medication FDA-approved for use to address alcohol and opioid addiction, is showing a positive impact in long COVID patients in a study reported in October 2022. The drug has been used in low doses (50 mg) with some success to treat symptoms of conditions like myalic encephalomyelitis/chronic fatigue syndrome (ME/CFS), MS, and fibromyalgia. Some long COVID patients have gotten relief from symptoms like brain fog, fatigue, pain, and sleep issues.
In addition to the naltrexone studies, there are a number of collaborations and clinical trials underway
- The VA has launched a Long COVID Clinic Practice Based Research Network to gather uniform data on their long COVID patients and to fund studies.
- The Department of Health and Human Services (HHS) has established a National Research Action Plan on Long COVID.
- The National Institutes of Health (NIH) has provided $1 billion to the RECOVER Initiative, which is focused on identifying definitively the underlying causes of long COVID and treatments to address it.
- Longitudinal Study of COVID-19 Sequelae and Immunity (RECON_19)
- Observational Study of Neurologic Function After COVID-19 Infection
- The CORONA Project
- Innovative Support for Patients with SARS-CoV-2 Infections Registry (INSPIRE) study
- Patient-Led Research Collaborative
- The Long Covid Research Initiative
You can stay up-to-date regarding NIH clinical trials at clinicaltrials.gov.
Long COVID clinics
Most patients with long COVID start their treatment journey with their PCP. So, finding a doctor who cares for your mental, physical, gynecological, and emotional health is important.
However, multiple specialists may be needed to reach a diagnosis and develop an effective care plan. And in some instances, it may be necessary and beneficial to seek care at special long COVID clinics.
At their best, long COVID clinics provide a single location for in-person care, which houses a multidisciplinary group of clinicians using a team approach and also makes virtual care options available. They offer a range of specialists who spend a significant percentage of their time taking care of long COVID patients and coordinate care following a treatment plan on which there is an agreement between clinicians. Both physical and emotional health needs are addressed.
The patient should be given every opportunity to share in decision-making, and there should be collaboration and transparency. A patient’s health beliefs, life circumstances, and finances should be considered to deliver high-quality care in the most cost-effective and least disruptive way possible.
More patients currently want to receive care at long COVID clinics than the clinics can accommodate.
Some require evidence of a positive COVID test before they will consider accepting a patient. For this reason, as well as the documentation you may need to file a future disability claim, testing takes on greater significance when deciding whether or not to get tested if you suspect you may have COVID, either due to symptoms or exposure to someone with known or suspected COVID. (The CDC provides guidance regarding testing.)
As is always the case, the more engaged and educated you become regarding any health conditions you may have, the better position you will be to obtain the care you want and deserve. With long COVID, the benefit of investing time will be significant – learning as much as you can and staying up-to-date as more studies report their results. And because long COVID is a new condition, there is no world “expert” with all the answers.
Long COVID support groups
Long COVID is a unique situation in which a patient can also be a pioneer and contribute to the knowledge base and development of future solutions.
Don’t underestimate the power of people coming together to educate, provide support, understanding, empathy, and a “safe place” to voice fears and concerns, share knowledge, and advocate for funding and prioritization in research. Some of the long COVID groups currently available include:
- Body Politic
- LONG COVID SUPPORT
- Administration for Community Living (ACL)
- ENDOCORONAVIRUS.ORG
- COVID Survivors for Change
- Solve Long COVID Initiative
Here are several resources focused on long COVID:
- CDC – Post-COVID Conditions and Caring for People with Post-COVID Conditions
- Patient Tips: Healthcare Provider Appointments for Post-COVID Conditions
- What doctors wish patients knew about long COVID
- Department of Education
- Department of Labor: Job Accommodation Network (JAN)
Lastly, be vigilant about the possibility of long COVID scams. With no known treatments, long COVID is a condition that can be a prime target used by those who sell “wonder drugs” and “miracle solutions” to con patients desperate for help. As a result, patients may be vulnerable to such overtures and find themselves spending lots of money to no avail, or, even worse, find their symptoms made worse or even develop new medical problems in reaction to the treatment.

Long COVID and medical gaslighting
Despite the existence of long COVID clinics and research studies validating the condition, some patients find their doctor doesn’t take their symptoms seriously.
Medical gaslighting describes a situation in which a patient’s symptoms and concerns are trivialized, dismissed, or even completely ignored by a healthcare provider.
For women, a clinician often manifests symptoms to stress, “hormones,” or being “all in your head.” This can happen for any number of health concerns, including medical gaslighting for menopause symptoms.
As a result, a patient may experience delayed diagnosis and treatment, as well as the frustration of navigating a healthcare system and some providers who do not take them seriously (in addition to the cost of trying to find answers and appropriate treatment).
Some patients may also begin to doubt themselves and/or feel shame or low self-esteem.
Medical gaslighting can also unfold as a misinterpretation or misdiagnosis of symptoms due to a narrowly focused search for an answer that will fit a clinical “profile” rather than keeping an open mind, actively listening, and being willing to admit to not having all the answers.
One example is the difference between the symptoms reported by women vs. men when having a heart attack. Although chest pain is the most common symptom overall regardless of gender, women may experience different symptoms—including dizziness, nausea and vomiting, heartburn, or unusual and unexplained fatigue—as opposed to the stereotypical jaw pain, “elephant on the chest,” and shortness of breath with which providers are more familiar (and which are seen more frequently in men). Consequently, a woman may show up in the ER experiencing a heart attack and be discharged with a GI diagnosis and no evaluation of a potential problem with her heart.
While it is always important when navigating the healthcare system to be assertive, to ask questions, to keep track of your records, and to make sure everyone treating you is aware of what others are doing, it is even more essential with a condition like long COVID.
With its broad array of symptoms, greater prevalence in female patients, symptoms for which a work-up may reveal only normal findings, and so much still to be learned, medical gaslighting is a distinct possibility to guard against and for which you should be prepared to encounter.
Medical gaslighting can create undue stress, anxiety, and depression, and, in the case of a missed diagnosis, delayed diagnosis, or misdiagnosis, irrevocable harm to one’s health or even death. It may also result in an unnecessarily greater cost of care, which impacts out-of-pocket expenses for the patient. For those who are uninsured, underinsured, or have very high deductibles, the risk of financially devastating medical debt is very real.
Medical gaslighting disparities
Medical gaslighting is reported to be more common in women, communities of color, patients who are obese, those with mental health conditions or disability, those with conditions like chronic fatigue syndrome and POTS, and the LGBTQIA+ community.
There are many factors that contribute to the medical gaslighting women may experience:
- Bias, discrimination, sexism, racism
- insufficient research (and underfunding of research) in women’s health
- lack of diversity in the healthcare workforce (clinicians, researchers, scientists, leadership)
- lack of diversity in clinical trials, scientific and pharmaceutical data analysis that does not include a consideration of potential gender-based differences
- inadequate medical professional training (relative to women’s health, gender-specific conditions, and varying sex-based symptom presentation)
- unequal power dynamics in the patient-physician relationship
The result? Health disparities, disillusionment, mistrust of the healthcare system, and needless suffering.
Is long COVID a disability?
A Brookings Institute analysis estimated long COVID could account for up to 15% of the 11.5 million unfilled jobs in the U.S.
The percentage may be higher in certain populations (e.g., in some studies, seen in up to 80% of those with an infection severe enough to require hospitalization) and in different parts of the world.
Long COVID is a condition for which disability protection under the Americans with Disabilities Act (ADA) may exist IF a patient meets the applicable eligibility definition.
Current estimates are that 2 – 5 % of patients with long COVID will progress to a state of disability.

The future of long COVID
All current signals point to a future in which we will live with COVID-19 for quite some time.
There is MUCH to be learned about women’s health and long COVID.
Ironically, a “silver lining” to the present state of affairs could emerge. The arrival of the novel coronavirus provides an opportunity to make up for lost time and avoidable suffering when it comes to studying, training in, and funding research in women’s health.
Major progress could be made in setting a new standard – working for solutions that are inclusive and equitable by definition – if the medical and scientific communities continue to collaborate globally, take the time to learn from lost historical opportunities, and intentionally design an innovative and novel approach to finding answers and developing treatments for long COVID.
Be sure to check back frequently, as pausitive health will continue to provide updates and information regarding research results!
New data shows long COVID is keeping as many as 4 million people out of work | The Brookings Institution
Canas, Liane S., Molteni, Erika, Deng Jie, Sudre Carol H., Murray, Benjamin, Kerfoot, Eric, Antonelli, Michela, Chen, Liyuan, Rjoob, Khaled, Capdevila Pujol, Joan, Polidori, Lorenzo, May, Anna, Österdahl, Marc F. Whiston, Ronan, Cheetham, Nathan J., Boywer, Vicky, Spector, Tim D., Hammers, Alexander, Duncan, Emma L., Ourselin, Sebastien, Steves, Claire J., Modat, Marc. Profiling post-COVID syndrome across different variants of SARS-CoV-2 medRxiv 2022.07.28.22278159; doi: https://doi.org/10.1101/2022.07.28.22278159
Subramanian, A., Nirantharakumar, K., Hughes, S. et al. Symptoms and risk factors for long COVID in non-hospitalized adults. Nat Med 28, 1706–1714 (2022). https://doi.org/10.1038/s41591-022-01909-w
Tosto-Mancuso J, Dai Y, Perotti E, Akduman K, Tzeng T, Xu L, Yildirim I, Krumholz H, Shon J, Medzhitov R, Omer S., van Dijk D, Ring A, Putrino D, Iwasaki A. Distinguishing features of Long COVID identified through immune profiling. medRxiv 2022.08.09.22278592; doi: https://doi.org/10.1101/2022.08.09.22278592
Postural Orthostatic Tachycardia Syndrome (POTS) | Cleveland Clinic
Diagnosis | PoTS UK
Tilt Table Test | Mayo Clinic
Symptoms of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome | Centers for Disease Control and Prevention
European studies shed light on long COVID risk and recovery | University of Minnesota
Multisystem Inflammatory Syndrome (MIS) | Centers for Disease Control and Prevention
Nearly One in Five American Adults Who Have Had COVID-19 Still Have “Long COVID” | Centers for Disease Control and Prevention
Self-reported long COVID after infection with the Omicron variant in the UK: 18 July 2022 | Office for National Statistics
What doctors wish patients knew about long COVID | American Medical Association
Azzolini E, Levi R, Sarti R, et al. Association Between BNT162b2 Vaccination and Long COVID After Infections Not Requiring Hospitalization in Health Care Workers. JAMA. 2022;328(7):676–678. doi:10.1001/jama.2022.11691
The PHOSP-COVID Collaborative Group. Clinical characteristics with inflammation profiling of long COVID and association with 1-year recovery following hospitalisation in the UK: a prospective observational study. The Lancet Respiratory Medicine. 2022, April 23. https://doi.org/10.1016/S2213-2600(22)00127-8
Sylvester, Shirley V., Rusus, Rada, Chan Biankha, Bellows, Martha, O’Keefe, Carly, Nicholson, Susan (Johnson & Johnson). Sex differences in sequelae from COVID-19 infection and in long COVID syndrome: a review. Current Medical Research and Opinion. 2022/08/03 https://doi.org/10.1080/03007995.2022.2081454
JAMA study: women twice as likely as men to develop long COVID | Institute for Health Metrics and Evaluation (IHME)
Newson, Louise, Lewis, Rebecca, O’Hara, Margaret. Long COVID and menopause – the important role of hormones in Long COVID must be considered. Maturitas. 2021. https://doi.org/10.1016/j.maturitas.2021.08.026
Receptor | Merriam-Webster
National Academics of Sciences, Engineering, and Medicine. Long COVID: Examining Long-Term Health Effects of COVID-19 and Implications for the Social Security Administration: Proceedings of a Workshop | The National Academies Press. 2022. https://doi.org/10.17226/26619
Lixue Huang, MD, Xia Li, MD, Xiaoying Gu, PhD, Hui Zhang, MD, LiLi Ren, PhD, Li Guo, PhD, et al. Health Outcomes in people 2 years after surviving hospitalisation with COVID-19: a longitudinal cohort study. The Lancet Respiratory Medicine. 2022. 05/11. https://doi.org/10.1016/S2213-2600(22)00126-6
Boscolo-Rizzo P, Fabbris C, Polesel J, et al. Two-Year Prevalence and Recovery Rate of Altered Sense of Smell or Taste in Patients With Mildly Symptomatic COVID-19. JAMA Otolaryngol Head Neck Surg. 2022;148(9):889–891. doi:10.1001/jamaoto.2022.1983
Maxime Taquet, PhD, Rebecca Sillet, BA, Lena Zhu, BS, Jacob Mendel, Isabella Camplisson, Quentin Dercon, et al. Neurological and psychiatric risk trajectories after SARS-CoV-2 infection: an analysis of 2-year retrospective cohort studies including 1 284 437 patients. The Lancet Psychiatry. 2022, August 17. https://doi.org/10.1016/S2215-0366(22)00260-7
Ty J. Gluckman, Nicole M. Bhave, Larry A. Allen, Eugene H. Chung, Erica S. Spatz, Enrico Ammirati, Aaron L. Baggish, Biykem Bozkurt, William K. Cornwell, Kimberly G. Harmon, Jonathan H. Kim, Anuradha Lala, Benjamin D. Levine, Matthew W. Martinez, Oyere Onuma, Dermot Phelan, Valentina O. Puntmann, Saurabh Rajpal, Pam R. Taub, Amanda K. Verma. 2022 ACC Expert Consensus Decision Pathway on Cardiovascular Sequelae of COVID-19 in Adults: Myocarditis and Other Myocardial Involvement, Post-Acute Sequelae of SARS-CoV-2 Infection, and Return to Play: A Report of the American College of Cardiology Solution Set Oversight Committee. Journal of the American College of Cardiology, Volume 79, Issue 17, 2022, Pages 1717-1756, ISSN 0735-1097, https://doi.org/10.1016/j.jacc.2022.02.003.
Long COVID (PASC) Resources | American Academy of Physical Medicine and Rehabilitation
Coronavirus Disease 2019 (COVID-19) Traetment Guidelines | National Institutes of Health
COVID-19 rapid guideline: managing the long-term effects of COVID-19. London: National Institute for Health and Care Excellence (NICE); 2020 Dec 18. PMID: 33555768.
Post-COVID-19 Condition: Guidance for Primary Care | Ontario Health
Dana Yelin, Charalampos D. Moschopoulos, Ili Margalit, Effrossyni Gkrania-Klotsas, Francesco Landi, Jean-Paul Stahl, Dafna Yahav. ESCMID rapid guidelines for assessment and management of long COVID. Clinical Microbiology and Infection. Volume 28, Issue 7, 2022, Pages 955-972. ISSN 1198-743X, https://doi.org/10.1016/j.cmi.2022.02.018.
Treating patients with long COVID | American Psychological Association
Clinical Guidelines: Long COVID-19 | Oregon Health & Science University
Key Learning Points: Updated NICE Guidance on Managing Long COVID | Medscape UK
COVID-19 rapid guideline: managing COVID-19 | National Institute for Health and Care Excellence
NICE Long COVID Guidelines | Long COVID Physio
Drug Repurposing for COVID-19 with CORONOA Registry | Penn Medicine
Addiction Drug Shows Promise Lifting Long COVID Brain Fog, Fatigue | Reuters
Long-COVID treatments: why the world is still waiting | Nature
Navigating Your Healthcare Journey | Authors for Advocacy, LLC
VA Launching Long COVID Research Inititiatve | GovernmentCIO Magazine LCC
National Research Action Plan on Long COVID | Department of Health and Human Services
RECOVER: Researching COVID to Enhance Recovery | RECOVER
An Observational Study of Neurologic Function After COVID-19 Infection | National Institutes of Health Clinical Center (CC) and National Institute of Neurological Disorders and Stroke (NINDS)
CORONA Project | Castleman Disease Collaborative Network
Online COVID-19 Health Study | CDC INSPIRE Study
About the Patient-Led Research Collaborative | Patient-Led Research Collaborative
The Long COVID Research Initiative | Long COVID Research Initiative
Clinical Trials | U.S. National Library of Medicine
COVID-19 Testing: What You Need to Know | Centers for Disease Control and Prevention
How long COVID is accelerating a revolution in medical research | The Washington Post
COVID-19 Support Group | Body Politic
Long COVID Support | Long COVID Support
Resources for People with Long COVID | Administration for Community Living
Long COVID | New England Complex Systems Institute Inc.
COVID Surivors for Change | COVID Survivors for Change
How Long Until We Solve Long COVID? | Solve ME/CFS Initiative
Long COVID or Post-COVID Conditions| Centers for Disease Control and Prevention
Patient Tips: Healthcare Provider Appointments for Post-COVID Conditions | Centers for Disease Control and Prevention
Long COVID under Section 504 and the IDEA | Office for Civil Rights and Office of Special Education and Rehabilitative Services
Job Accommodation Network | Job Accommodation Network
Patient Tips: Healthcare Provider Appointments for Post-COVID Conditions | Centers for Disease Control and Prevention
CDC is asked to release race and gender data on long COVID | The Washington Post
Guidance on “Long COVID” as a Disability Under the ADA, Section 504, and Section 1557 | U.S. Department of Health and Human Services
You may also like…
5 Ways COVID-19 Can Impact A Woman’s Health
COVID-19 can impact a woman’s health. Learn how.

5 Ways Medical Gaslighting Can Make Your Menopause Journey More Difficult
Do you feel like your doctor dismisses your menopause symptoms? Medical gaslighting can leave you feeling crazy and make menopause harder.

Prepare for Menopause Like A Marathon: Your Body Will Thank You
Menopause is a marathon, not a sprint. You have the opportunity to enhance your health and well-being for the rest of your life. And, just like the 26-mile run, preparation for the “Menopause Marathon” is key to reaching the finish line. Focus on your body, mind, and spirit so you can feel your best during this natural stage of life.