Have you started noticing pimples on your face and torso in your 40s and 50s? Have you had sudden breakouts of acne for what feels like no good reason? You might be experiencing menopausal acne, sometimes referred to as hormonal acne. It’s yet another menopause symptom! Let’s dive into how to clear your skin of these unwanted blemishes.
Menopause acne
You’re in midlife, but do you feel like you’re back in high school again worrying about acne? While you probably thought acne was limited to the teenage years, the truth is, you can experience a breakout at any stage of life, including during the menopause journey.
That’s why the menopause journey often feels like going through a second adolescence along with mood swings, embarrassment, and body changes.
Don’t worry – it’s not quite puberty all over again! Hormonal acne tends to be less severe, and the prevalence goes down as you age.
Does estrogen cause acne?
When acne appears during the menopause journey, it’s likely caused by the imbalance and volatility of hormone levels including estrogen which most women+ most closely associate with the journey.
But, it’s not the only hormone responsible. These hormones play a role:
- estrogen
- progesterone
- testosterone
Estrogen and progesterone drop significantly and eventually fall to a new baseline during the post-menopause stage of the journey. This hormonal fluctuation can have a notable impact on the skin, leading to the development of acne as well as issues with dry, itchy skin.
In other words, your skin is sensitive to your hormones. But why can that cause acne?
Research shows that when hormone fluctuations happen during menopause, it impacts sebum production. That’s an oily substance that protects your skin from drying out.
As estrogen levels decrease, there’s also a relative increase in testosterone. That can lead to more sebum (oily substance). The excess oil and shedding of skin cells can lead to clogged pores and acne.
Here’s a visual to explain this process.
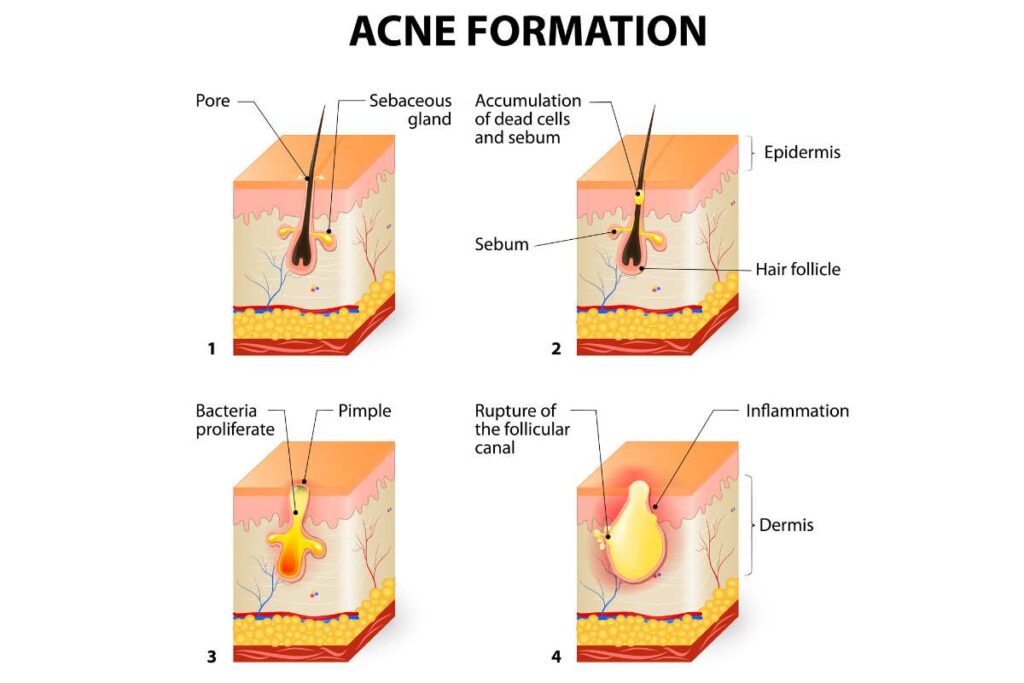
The delicate balance between estrogen, progesterone, and androgen hormones like testosterone, is disrupted during menopause, allowing hormonal acne to emerge. These hormonal fluctuations can lead to increased sebum production, clogged pores, and the growth of acne-causing bacteria.
Acne triggers
It’s not just hormones playing tricks on you. Women+ should consider their lifestyle during the menopause journey. That can trigger blemishes too along with other factors.
These triggers include:
- diet
- obesity
- smoking
- cosmetics
- sleep deprivation
- stress
- exposure to the sun’s UV rays
- genetics
- health conditions*
- medications*
*Health conditions can hijack your skin as well as medications, especially those which increase androgen levels in your bloodstream. For example, in a sleep study, acne was triggered by an insomnia medication that contained an androgen.
Some of these acne triggers like sleep deprivation and stress can be co-existing menopause symptoms.
So, while hormones are the main culprit, you should also look at your health and well-being holistically. You may not be able to control your hormones, but you can control what you eat, your weight, stress levels, and your skincare routine.
That’s why some of the adult acne treatment options are lifestyle-related.
Where does menopausal acne show up?
Menopausal acne can pop up in different areas of the body, but there are certain places where it tends to show up more often.
During menopause, you may notice acne appearing on your:
- Face
- Forehead
- Cheeks
- Chin
- Around your mouth
- Neck
- Chest
- Back
These are the usual suspects when it comes to adult acne. But, it can also appear on other parts of the body as well.
Sometimes the acne is itchy or in the form of a menopausal acne cyst. The cyst is a deeper, more painful acne lesion that requires special attention and treatment.
Perimenopause acne
Some women+ start getting acne during perimenopause, which is the phase leading up to menopause. If you experience premature (age < 40) or early (40 or older but younger than 45) menopause, it can kick in even earlier.
It can happen at any time during the menopause journey, though. Usually, women+ report that acne appears between the ages of 45 and 55.
How long does menopause acne last?
Even after menopause (12 consecutive months without a period) is over and your periods have stopped completely, menopausal acne can still stick around.
In one study, postmenopausal women+ who were taking hormonal treatment with testosterone were more likely to develop acne. Testosterone is sometimes used to address low libido is women+ (in addition to the role it may play in transgender transitions).
However, the risk goes down as you age with it prevalent in about 26% of women in their 40s and 15% of women 50 years old or older.
If you do experience acne during the post-menopause stage, it’s a good idea to consult your healthcare provider as this can sometimes be a symptom of other conditions, such as polycystic ovary syndrome (PCOS) or a thyroid condition.
Every woman+’s experience with menopausal acne is different. It’s a good idea to talk to your healthcare practitioner for advice on the best way to manage and treat it in your particular situation.

Acne in women of color
Menopausal acne can affect women+ of all skin tones. However, in women+ with darker skin, acne can cause:
- scarring
- dark marks
- hyperpigmentation
- keloid scars (scar tissue that grows)
This happens because the skin produces extra melanin. That’s what typically adds pigment to your skin and protects you from harmful UV rays. But, when acne inflames your skin, more melanin is released, which can lead to dark spots. It’s more common in women+ with darker skin.
This skin damage can last longer than the pimples and cysts.
Find a dermatologist who specializes. in darker skin tones.
Besides acne, women of color – WOC – need to be aware of other skin conditions that are more prevalent, which may present differently or need to be treated differently than in white populations.
It’s not just acne that may be different. Learn about other menopause symptoms and how they can impact your journey as a woman of color.
Acne for transgender and gender diverse individuals
Acne can also be problematic for transgender and gender diverse individuals.
A large study of 46,507 patients concluded there is an increased likelihood of acne in those who are taking masculinizing gender-affirming hormone therapy, which contains the androgen testosterone.
In contrast, the study also found that people taking female gender-affirming hormone therapy may be at a decreased risk of acne, confirming the role testosterone and other androgens play in triggering acne breakouts.
Acne can be especially detrimental to the mental health and well-being for this community, who may already experience discrimination, bias, health disparities, medical gaslighting, and difficulty finding welcoming healthcare practitioners with the expertise and experience to address unique needs that may be present.

Menopause acne treatments to clear it up
There are many treatment options for acne.
Talk to your healthcare practitioner about the best treatment for your individual needs. They may even refer you to a dermatologist if needed.
The treatment regimen selected depends on factors like:
- severity of the condition
- your medical history
- age
- other medications you may be taking
- whether or not hyperpigmentation and/or scarring complicates the picture
Here are some of the most common treatments available.
1. Topical treatments
These tend to be the first-line approach for many and have the added benefit of also improving the signs of aging and photoaging (premature aging of the skin due to sun exposure). They include:
- retinoids like adapalene, which help unclog pores and encourage cell turnover,
- benzoyl peroxide, which has antimicrobial properties and reduces inflammation salicylic acid, which helps skin cells to shed, decreases pimple formation and speeds healing
- topical antibiotics, like clindamycin and erythromycin
A combination of topical treatments may also be used for mild to moderate acne.
2. Systemic therapy
This includes:
- antibiotics
- hormonal antiandrogens (e.g., spironolactone a diuretic that is also used for the treatment of hypertension and heart failure)
- oral isotretinoin
- hormonal therapy like spironolactone
Systemic treatment becomes a consideration for more severe forms of acne, e.g., papulopustular and nodulocystic acne.
3. Procedural therapy
This is used when other treatments have failed or scarring has developed including techniques like:
- steroid injections
- chemical peels
- laser therapy
4. Lifestyle changes
As with other aspects of health and well-being and many medical conditions, lifestyle factors can make a difference in the management of acne.
Diet
The type of food you eat can have an impact on your skin.
A study in France found that people who ate a Western style diet, i.e., lots of meat and fatty, sugary foods) were much more likely to develop adult acne.
These foods are associated with the development of inflammation in the body, which can increase the risk of acne.
And some studies suggest that following a low-glycemic diet may help prevent or improve acne. These are foods like green vegetables or carrots that have a low impact on your blood sugar level.
The gut microbiome
Emerging research suggests a potential link between gut health and acne, highlighting the role of the gut microbiome in skin health.
The gut microbiome is made of trillions of microorganisms that live in the digestive tract and play a vital role in lots of bodily functions. Studies have shown that an imbalance in the gut microbiome, known as dysbiosis, may contribute to the development of acne.
By encouraging inflammation and weakening the skin’s natural barrier, dysbiosis can make acne symptoms worse.
Improving gut health through changes to your diet, like eating more fiber-rich foods, probiotics, and prebiotics, may help restore and maintain a healthy microbiome balance and help resolve your acne symptoms.
Also, adopting a balanced and nutritious diet, drinking enough water, managing your stress levels, and getting regular exercise can also help your overall gut health.
Sleep
Some research indicates a relationship between sleep and acne. Poor sleep quality and fatigue on waking have been associated with more severe acne.
During the menopause journey sleep issues are a common complaint. Hot flashes and night sweats contribute to problems staying asleep and getting enough good-quality thereby potentially increasing the severity of acne during this stage of life.
Stress
A direct causative relationship between stress and acne has not been found. However, being stressed increases the level of the stress hormone, cortisol (which may already be elevated due to the dropping estrogen and progesterone levels that occur during the menopause journey). In turn, elevated cortisol levels can lead to inflammation and increased production of oil in sebaceous glands. So indirectly, stress can trigger or exacerbate an acne outbreak.

Menopause skin care
Taking good care of your skin is important at any stage in life. The hormonal transition may require doing a few things differently and adjusting your skincare routine.
For example:
- Be on the lookout for signs of dry skin like flaking and itching. And some over-the-counter acne skin care products may dehydrate skin, actually making acne worse. If you find that to be the case, contact your healthcare practitioner for guidance.
- Sun protection remains essential to reduce the risk of skin cancer and to help avoid photoaging. However, an oil-free sunscreen may be a better selection if you are experiencing acne during the menopause journey.
- If you use cosmetics, make sure you are using fresh products and eliminating any that are old and could potentially expose your skin to bacterial contamination from your makeup. Using cosmetics that do not contribute to clogging pores (noncomedogenic) may also be helpful.
Learn more about general care of your skin during the menopause journey from pausitive health’s skincare guide. And of course, always contact your PCP or dermatologist for guidance and to address any concerns as well as for recommendations regarding overall body skin checks for early detection of skin cancer.

Soothe Dry Itchy Skin
Shop a safe, gentle, clinically-proven line of skincare designed specifically for the unique needs of people with the most compromised skin. While originally designed to help cancer patients, Lindi Skin products can also help with aging and menopausal skin that’s dry, itchy, and sensitive. A portion of each sale helps those fighting cancer. Use code “pausitive“ for at least 10% off.
This is an affiliate link. We may earn a small commission if you access these services. The companies we work with are carefully vetted. However, we do not guarantee their products and services.

Finding help with your skin
The bottom line? Help is available. Not only do you not have to suffer in silence, but there are actions under your control that you can take right now to make a change for the better!
Resources:
Free Support
For A Limited Time!
pausitive health offers personalized support for every stage of the menopause journey. Customize your experience with 14 evidence-based educational tracks, a diet assessment with recommendations and a food library, solutions for aches and pains, virtual care options, practical lifestyle supports, and a supportive community. All in one trusted place.
Join the pilot and be the first to know when our web-app is coming in 2026!
Sebaceous Glands | Cleveland Clinic
The hormonal causes of adult acne | Women’s Health Network
Khunger N, Mehrotra K. Menopausal Acne – Challenges And Solutions. Int J Womens Health. 2019 Oct 29;11:555-567. doi: 10.2147/IJWH.S174292. PMID: 31754313; PMCID: PMC6825478.
Menopause and Acne | Acne.org
Kamp E, Ashraf M, Musbahi E, DeGiovanni C. Menopause, skin and common dermatoses. Part 2: skin disorders, Clinical and Experimental Dermatology, Volume 47, Issue 12, 1 December 2022, Pages 2117–2122, https://doi.org/10.1111/ced.15308
Braunstein GD. Safety of testosterone treatment in postmenopausal women. Fertil Steril. 2007 Jul;88(1):1-17. doi: 10.1016/j.fertnstert.2007.01.118. Epub 2007 May 10. PMID: 17493618.
The Menopause Society (formerly North American Menopause Society). The role of testosterone therapy in postmenopausal women: position statement of The North American Menopause Society. Menopause. 2005 Sep-Oct;12(5):496-511; quiz 649. doi: 10.1097/01.gme.0000177709.65944.b0. Epub 2005 Sep 1. PMID: 16145303.
Collier CN, Harper JC, Cafardi JA, Cantrell WC, Wang W, Foster KW, Elewski BE. The prevalence of acne in adults 20 years and older. J Am Acad Dermatol. 2008 Jan;58(1):56-9. doi: 10.1016/j.jaad.2007.06.045. Epub 2007 Oct 22. Erratum in: J Am Acad Dermatol. 2008 May;58(5):874. Cafardi, Jennifer A [added]. PMID: 17945383.
Acne: Considerations for darker skin | Harvard Health Publishing
8 Tips for Skin of Color, Straight from Dermatologists | Byrdie
Gao J, King D, Modest A, Dommasch E. Acne risk in transgender and gender diverse populations: A retrospective, comparative cohort study. Journal of the American Academy of Dermatology. Volume 87, Issue 5, 2022, Pages 1198-1200,
ISSN 0190-9622, https://doi.org/10.1016/j.jaad.2022.03.013.
Penso L, Touvier M, Deschasaux M, et al. Association Between Adult Acne and Dietary Behaviors: Findings From the NutriNet-Santé Prospective Cohort Study. JAMA Dermatol. 2020;156(8):854–862. doi:10.1001/jamadermatol.2020.1602
Low-glycemic index diet: What’s behind the claims? | Mayo Clinic
Sánchez-Pellicer P, Navarro-Moratalla L, Núñez-Delegido E, Ruzafa-Costas B, Agüera-Santos J, Navarro-López V. Acne, Microbiome, and Probiotics: The Gut–Skin Axis. Microorganisms. 2022; 10(7):1303. https://doi.org/10.3390/microorganisms10071303
How To Select a Dermatologist, Find a Dermatologist, Find a Free Skin Cancer Screening, Find Skin Cancer: How to Perform a Skin Self Exam | American Academy of Dermatology
Skin of Color | American Society for Dermatologic Surgery
Home | Skin of Color Society
You may also like…

8 Solutions To Get Relief When Dry, Itchy Skin Happens During Menopause
Does your skin feel dry and itchy? It’s a menopause symptom. Learn 7 solutions to get relief from the itch.

Menopause Is Just Like Being A Teenager Again, Except You’re Wiser For It
Menopuase is like a second adolescence, bringing back memories of acne, moodiness, and other teenage concerns. Learn how to navigate it!

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

