Did you know you have two cores? There’s your abdominal core that we associate with crunches and other exercises and your “forgotten core” or pelvic floor muscles that prevent urine and stool leakage, constipation, back pain, and pelvic pain. These symptoms may surface during the menopause journey, reminding you of your forgotten core. Understanding where these muscles are located, and whether yours are tight or weak, can help you understand the type of pelvic floor dysfunction you may experience during the menopause journey.
How does the menopause journey change your pelvic floor?
As you go through the menopause journey, your hormone levels shift. In particular, your estrogen levels decline. Estrogen is a vital hormone produced in your ovaries which, among many things, promotes muscle repair and growth.
When estrogen levels decrease, muscles can weaken, including those that make up the pelvic floor.
This change can result in various symptoms, including:
- urine leakage
- stool leakage
- constipation
- pelvic pain
- urinary tract infections
The pelvic floor is the forgotten core
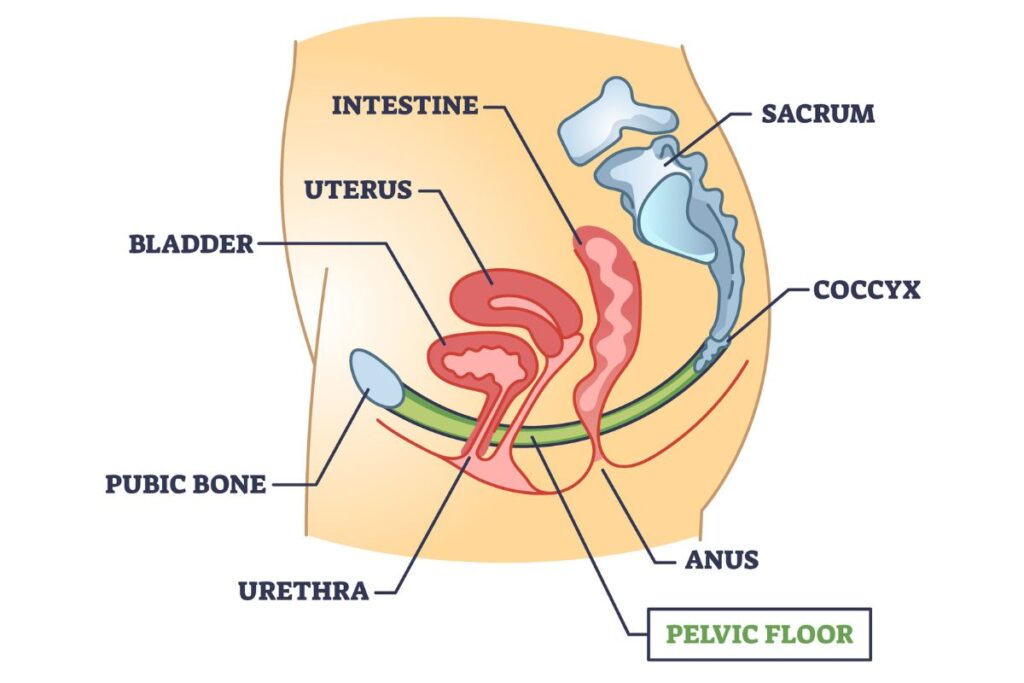
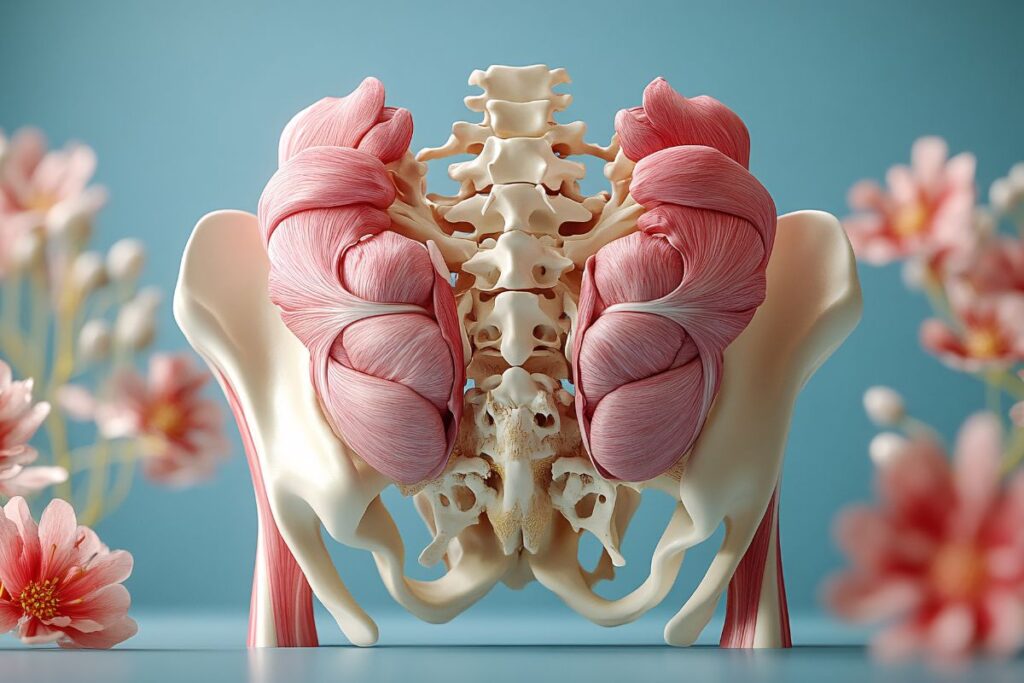
Most core exercises target your abdomen or midsection. But, the “forgotten core” or “other core” includes the muscles that run across the bottom of your pelvis or the lower part of your torso between your legs and abdomen.
You may not realize the importance of this area of your body during the menopause journey when you start to have symptoms.
Your pelvic floor works with your abdominal, back, and breathing muscles to help support your spine and manage the pressure within your abdomen. It also spans from front to back and helps support your bowels, uterus, and bladder.
These organs sit within your pelvis above your pelvic floor. But your anus, urethra (the tube that urine leaves), and vagina all pass through your pelvic floor.
So, when your pelvic floor tightens, it becomes more difficult for things to leave through these tubes. When it loosens, these passages open. This is why you have different symptoms depending on whether your pelvic floor muscles are weak or tight.
Keep in mind, the menopause journey can cause a variety of issues. Your pelvic floor may be just one piece of the puzzle. So, speak with your doctor about all your symptoms.
How to tell if your pelvic floor is tight or weak?
To function appropriately, your pelvic floor muscles need to be able to both loosen and tighten with adequate strength and coordination.
Your pelvic floor muscles can be both weak and/or tight. But each has some distinct symptoms you can look out for. And it’s important to distinguish which you have, or if you have both, as it will help determine the most effective treatment type.
Weak pelvic floor
If you have a weak pelvic floor, you may experience:
- Urinary or stool incontinence
- Pelvic organ prolapse
- Sexual dysfunction (pelvic floor pain after sex or trouble having an orgasm)
- Lower back or pelvic pain, especially lasting more than 6 months
Hypertonic pelvic floor symptoms (tightness)
Pelvic floor tightness is also known as a hypertonic pelvic floor. When a muscle is hypertonic, it has too much tone. So it is stiff and difficult to move.
Tight pelvic floor symptoms in females include:
- Difficulty passing urine or emptying your bladder.
- Constipation due to pelvic floor dyssynergia.
- Pain known as pelvic floor myalgia.
- Pelvic floor spasms.
What is pelvic floor dyssnergia?
Pelvic floor dyssynergia is a disturbance in muscular coordination. It can lead to abrupt and uncoordinated movements.
This occurs when your pelvic floor won’t relax. So, you may have difficulty having or evacuating a bowel movement, and end up feeling that you are not able to completely empty your rectum.
It can also lead to constipation.
What is pelvic floor myalgia?
That’s pain in a muscle group or group of muscles. You may feel this in any part of your pelvis, including your bladder, bowels, and vagina. It may be consistent or worsen with specific movements or activities.
What are pelvic floor spasms?
This is an involuntary tightening of your pelvic floor. Symptoms can vary greatly, so it can be difficult to diagnose. But it may feel like tightening, twitching, or fluttering in your uterus, vagina, or lower abdomen. You also may experience pain after certain activities, like intercourse. Spasms can also lead to urinary and bowel issues.

UTIs with weak and tight pelvic floors
Unfortunately, weak, and tight pelvic floors can cause other issues, like urinary tract infections (UTIs).
If you’re experiencing urine leakage or trouble emptying your bladder, you’re more likely to develop a UTI. If this happens, your UTI could worsen your pelvic floor symptoms. Many women experience urgency and leaking during a UTI. You may also experience painful urination.
Additionally, the menopause journey and UTIs are linked by more than your pelvic floor. The hormonal changes can cause your vaginal tissues to become thin and dry.
Plus, the microbiome (the collection of all microbes, such as bacteria, viruses, and fungi, that naturally live on our bodies and inside us) of your urinary tract may be altered as well.
Your urethra (the internal tube used to urinate) may also shorten. All of these factors can make you more prone to UTIs.
Types of pelvic floor disorders (PFDs) in women+
There are several types of pelvic floor disorders. Unfortunately, you can experience more than one.
About 1 in 3 women+ have at least 1 PFD. That number increases as women age, increasing to 50% of women+ 80 years and older.
There are three main types:
- urinary incontinence (UI)
- bowel dysfunction
- pelvic organ prolapse (POP)
1. Urinary incontinence (UI)
There are several types of urinary incontinence. But the two most common forms are stress incontinence and urge incontinence.
- People with stress incontinence experience urine leaks when they cough, sneeze, laugh, or exercise.
- People with urge incontinence experience a sudden urge to void or an involuntary leakage of urine.
In general, more than 10% of women suffer from urinary incontinence. But this number is more than 4 times higher for peri- and post-menopausal women+.
GSM and pelvic floor
If you experience urinary leaking, it may also be a symptom of genitourinary syndrome of menopause (GSM).
GSM is an umbrella term for a wide range of genital, sexual, and urinary symptoms. It can refer to symptoms like vaginal dryness, pain in your vagina, vulva, pelvis, or urinary tract. You might also have GSM if you have low libido or pain during sex.
So, it’s important to speak with your doctor about everything you are experiencing to get an accurate diagnosis and treatment plan. Some of the symptoms of GSM are best addressed with hormone therapy, but pelvic floor exercises like Kegels can help others.
2. Bowel dysfunction
Altered bowel function can range from constipation to gaseousness to stool incontinence.
- If your pelvic floor muscles are too tight, you may experience constipation. This includes having difficulty getting stool out or feeling like you haven’t fully emptied your bowels.
- If your pelvic floor muscles are weak, you may experience leakage of stool. Your symptoms could be as mild as minor leakage while passing gas.
But your bowel dysfunction could be as bad as experiencing a complete loss of bowel control.
Almost 2 out of 5 post-menopausal women+ experience altered bowel function.
3. Pelvic organ prolapse (POP)
Normally, your pelvic floor muscles hold your pelvic organs (bladder, uterus, and rectum) in place. But if they weaken, your pelvic organs can drop and press out of your vagina. This is known as pelvic organ prolapse.
If this happens, you may see or feel a bulge at or beyond the opening of your vagina. You may also experience:
- Pelvic pain or heaviness
- Problems inserting tampons during perimenopausal periods
- Lower back pain
- Pain during intercourse
- Urinary or bowel changes
- Urgency or not being able to completely empty bladder or bowels.
About 1 in 3 post-menopausal women+ develop a pelvic organ prolapse (POP) that causes symptoms. As you transition through your menopause journey, your symptoms and severity may increase.
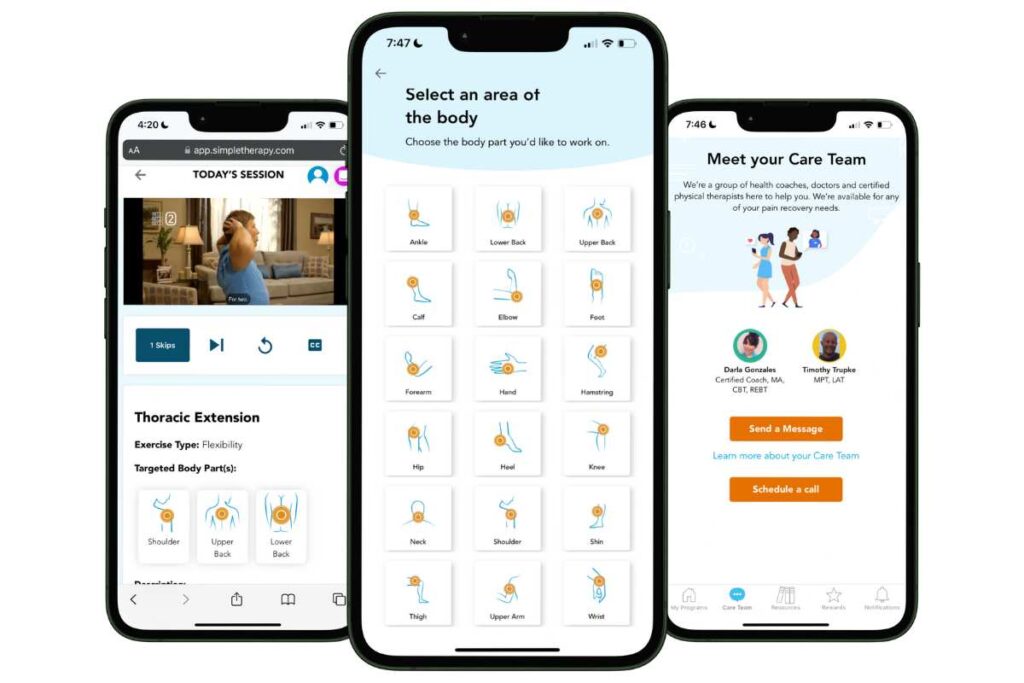
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!
Risk factors for pelvic floor dysfunction or disorder
Pelvic floor disorders are common, with about 30% (or potentially more depending on one’s medical history) of all women+ having at least 1 issue. About 17% suffer from two issues, and 8% suffer from 3 or more.
The most common symptoms are urinary or stool incontinence, pelvic pain, and symptoms of pelvic organ prolapse.
But besides menopause, what can put you at risk for having pelvic floor disorders? It can be:
- age
- weight
- pregnancy history
- long-term constipation or intestinal issues
1. Age
Like many muscles in your body, those in your pelvic floor can weaken or tighten as you age. As you grow older, the likelihood of developing urine or stool incontinence increases.
2. Weight
Weight can put pressure on your pelvic floor, leading to muscle stretching and weakness and bowel and bladder issues.
During the menopause journey, it’s common for women+ to experience weight gain. In fact, it’s the #1 symptom reported by pausitive health members.
As your weight increases, you’re also more likely to experience pelvic pain and pain during sex.
pausitive health can help you manage your weight, with our pilot program. Get access to recipes, a diet assessment, and information on managing your weight. Join today!
3. Pregnancy history
Pregnancy and delivery can cause trauma to your pelvic floor.
Having a history of vaginal delivery or multiple pregnancies increases your risk of having pelvic floor dysfunction. This includes pelvic organ prolapse, as well as urinary and bowel issues.
Unfortunately, women+ who’ve had a birth requiring forceps or vacuum suction are at a higher risk of developing stool incontinence.
4. Long-term constipation or intestinal issues
The strain of trying to go can cause damage to your pelvic floor muscles over time. This usually leads to experiencing additional or worsening bowel dysfunction symptoms.

Health disparities in pelvic floor dysfunction or disorder
The risk of developing pelvic floor disorders increases with age. And women+ are twice as likely as men to suffer from at least 1 pelvic floor disorder. But for women+, race is also a factor.
Compared to white women+, Asian women+ have a lower risk for all pelvic floor disorders.
Despite having more risk factors, like high rates of obesity and diabetes, for urinary incontinence, Black women+ actually have a lower risk for both urinary incontinence and pelvic organ prolapse. But they are more likely to have bowel dysfunction.
But the rate of pelvic floor dysfunction isn’t the only difference between races.
Actual care and types of treatment interventions are also factors. Hispanic/Latina women+ are more likely to suffer from pelvic organ prolapse than other races. But white women+ are more likely to have surgical intervention. And unfortunately, Black women+ who have surgery tend to have longer hospital stays.
One study showed that white women+ are far more likely to seek care for their urinary incontinence symptoms. Take a look at the differences between white women and women of color who seek care:
- 70% of white women+
- 16% of Latinas
- 6% of Black women+
- 5% of Asian women+
Having access to quality care, being taken seriously, and having a trusting relationship with a healthcare professional are just some of the factors that can impact whether or not someone seeks care.
General knowledge about pelvic floor dysfunction also varies between races. Compared to white women+, Black and other women+ of color are less likely to know about the benefits of pelvic floor muscle exercises and their impact on pelvic floor disorders.
So, knowing your risk of developing pelvic floor issues and seeking help for your symptoms could improve your quality of life and end needless suffering.
During the pausitive health podcast, Menopause the pausitive way, host Courtney Pesek spoke with the Peli Health co-founders about their holistic approach to pelvic health.
Get treatment
Recognizing that your pelvic floor may be causing your symptoms is only the first step. You also need to know if your pelvic floor is tight or weak to treat your symptoms appropriately.
A urogynecologist specializes in pelvic floor conditions. You may want to talk to your primary care doctor about a referral or seek out a specialist on your own.
There are many pelvic floor treatment options, from physical therapy to lifestyle and medication options.
You don’t have to suffer with menopausal symptoms. Make today the day you make a change for the better!
Collins B, Laakkonen E, Lowe D. Aging of the musculoskeletal system: How the loss of estrogen impacts muscle strength. Bone, Volume 123, 2019,
Pages 137-144. ISSN 8756-3282,
https://doi.org/10.1016/j.bone.2019.03.033.
Polackwich AS, Li J, Shoskes DA. Patients with Pelvic Floor Muscle Spasm Have a Superior Response to Pelvic Floor Physical Therapy at Specialized Centers. J Urol. 2015 Oct;194(4):1002-6. doi: 10.1016/j.juro.2015.03.130. Epub 2015 Apr 23. PMID: 25912491.
Kenne, K.A., Wendt, L. & Brooks Jackson, J. Prevalence of pelvic floor disorders in adult women being seen in a primary care setting and associated risk factors. Sci Rep 12, 9878 (2022). https://doi.org/10.1038/s41598-022-13501-w
Kołodyńska G, Zalewski M, Rożek-Piechura K. Urinary incontinence in postmenopausal women – causes, symptoms, treatment. Prz Menopauzalny. 2019 Apr;18(1):46-50. doi: 10.5114/pm.2019.84157. Epub 2019 Apr 9. PMID: 31114458; PMCID: PMC6528037.
Huang H, Ding G, Li M, Deng Y, Cheng Y, Jin H. Menopause and stress urinary incontinence: The risk factors of stress urinary incontinence in perimenopausal and postmenopausal women. The Journal of Obstetrics and Gynaecology Research. 2023. Volume 49, Issue 10, Pages 2509-2518. https://doi.org/10.1111/jog.15742
Grimes WR, Stratton M. Pelvic Floor Dysfunction. [Updated 2023 Jun 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Triadafilopoulos G, Finlayson M, Grellet C. Bowel dysfunction in postmenopausal women. Women Health. 1998;27(4):55-66. doi: 10.1300/J013v27n04_04. PMID: 9796084.
Aboseif C, Liu P. Pelvic Organ Prolapse. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-.
Sengupta N, Hillard T. Urogynecological Risk Assessment in Postmenopausal Women. Expert Rev of Obstet Gynecol. 2013;8(6):625-637.
Giannini A, Russo E, Cano A, Chedraui P, Goulis D, Lambrinoudaki I, Lopes P, Mishra G, Mucek A, Rees M, Senturk L, Stevenson J, Stute P, Tuomikoski P, Simoncini T. Current management of pelvic organ prolapse in aging women: EMAS clinical guide. Maturitas. 2018. Volume 110, pages 118-123. https://doi.org/10.1016/j.maturitas.2018.02.004
Peinado-Molina, R.A., Hernández-Martínez, A., Martínez-Vázquez, S. et al. Pelvic floor dysfunction: prevalence and associated factors. BMC Public Health 23, 2005 (2023). https://doi.org/10.1186/s12889-023-16901-3
Hartigan SM, Smith AL. Disparities in Female Pelvic Floor Disorders. Curr Urol Rep. 2018 Feb 23;19(2):16. doi: 10.1007/s11934-018-0766-3. PMID: 29476354.
You may also like…

Is Your Pelvic Floor in Perimenopause Too?
Give your pelvic health some love in perimenopause. It’s more than Kegels. Get solutions to improve vaginal and sexual health, your bladder, and pelvic floor.

Pelvic Floor Rehab: 10 Treatment Options During the Menopause Journey
Pelvic floor symptoms can be embarrasing, but don’t have to be. Learn about pelvic floor rehab options. Get treatment that’s right for you.

Menopause Bloating and Constipation? Don’t Suffer From GI Pain Any More
Does your stomach hurt or feel bloated? Menopause GI pain can cause several symptoms in your gastrointestinal tract. Learn how to manage them.

