Have your bowel habits changed? Feeling bloated? Having new problems with abdominal cramps, gas, or indigestion? It could be a sign that you’ve begun the menopause journey. The hormonal changes of menopause can affect your gut health, and your gut health can affect how you feel during the journey. We’re here to make your journey more “pausitive,” so let’s find out what’s causing your stomach pain, and ways to treat it.
Gastrointestinal (GI) pain during menopause
How does your gut feel? Menopause can throw off your gastrointestinal (GI) tract.
While menopause may be the cause, it could also be a sign of another health condition. It’s tricky. Many of the GI symptoms experienced during the menopause journey are common or can be related to other conditions. Always talk to your healthcare provider to determine if other causes need to be ruled out before assuming it’s menopause.
GI pain and upset could be a sign of menopause or:
- A change in bowel habits could be a sign of colon cancer.
- Constipation could be a symptom of hypothyroidism.
- Abdominal pain and bloating could signal ovarian cancer.
If you and your healthcare provider believe your stomach pain or bowel changes are related to menopause, some of the symptoms or signs you may be experiencing include the following:
- Abdominal or pelvic pain or cramps
- Bloating
- Flatulence (aka gas)
- Constipation
- Indigestion and GI reflux
- Nausea and vomiting
- Diarrhea
- Gallstones
- Pancreatitis
Are you having one of these symptoms? Go right to that section which details why you may be experiencing it during menopause and possible treatment options, by clicking on it above.
What causes GI symptoms during menopause?
Like almost every other menopause symptom, hormone changes top the list of culprits for why you’re having stomach troubles. It’s not just a drop in estrogen that’s to blame, though. Progesterone also decreases, and an increase in cortisol can also be contributory.
The midlife (or earlier if you have premature or early menopause) changes that affect your gastrointestinal tract include:
- Changes in the hormonal profile – estrogen, progesterone, and cortisol
- Increased sensitivity to hormone changes
- Hormone Therapy (HT)
- Extreme hot flashes
- Pelvic floor issues
- Gut microbiome
- Midlife stressors

Managing gut health
The management of GI symptoms during the menopause transition depends on the type of symptom and its cause.
But some basics can help optimize your GI health in general.
They include:
- a high-fiber diet (≥ 25 grams of fiber per day) with a low glycemic index
- the Mediterranean diet
- reducing your intake of sugar
- avoiding processed foods
- prebiotic and probiotic foods
- water intake sufficient enough to prevent dehydration
- sufficient physical activity levels
- coping skills that help address stress and anxiety
- Avoiding heavy alcohol intake. Alcohol in moderation is defined as no more than 1 drink per day in women+ (It’s important to note that The World Heart Federation has taken a stance that no amount of alcohol is safe to drink because of the impact it can have on the heart.)
| What is 1 drink? | |
|---|---|
| 5 fluid ounces | a glass of wine at an alcohol content of 12% |
| 12 fluid ounces | a standard bottle or can of regular beer at an alcohol content of about 5% |
| 1.5 fluid ounces | a shot glass of 80-proof distilled alcohol |
 Menopause bloating
Menopause bloating
Are you feeling bloated – as if you’ve gained weight, even though you haven’t changed your eating habits?
The bloating may make your midsection feel full, tight, or painful. The abdominal pain may be a result of bloating, gas, or constipation.
This happens because of changes to your hormonal profile.
During menopause, there is a significant drop in estrogen and progesterone levels, a change that can be quite volatile until they eventually settle out.
When estrogen and progesterone levels fall, the motility (movement) of the GI tract can slow down. As a result, more water can be reabsorbed as food and fluids move through the gastrointestinal system.
You may feel these changes long before menopause. Remember, menopause is the time when you have not had a period for 12 consecutive months. The time leading up to this moment is perimenopause and can last several years.
Can menopause cause constipation?
Yes. Constipation can strike at any time during the menopause transition. It tends to increase with age. Bloating may be one sign you’re constipated.
Constipation is when bowel movements change, becoming infrequent (less than three times a week) or uncomfortable.
Even when you go to the bathroom, you may also feel like you haven’t completely emptied your bowels.
Elevated cortisol levels (a stress hormone) seen during the menopause journey can cause constipation along with the overall slowdown of the GI tract.
Constipation due to pelvic floor issues
You may also experience constipation due to pelvic floor issues.
As women+ get older, their their pelvic floor muscles may weaken and become more lax.
This change is even more common in women who have had a vaginal delivery (particularly if they have had multiple deliveries), forceps were required, the baby was large, or if chronic constipation with straining has been a problem.
Some research suggests falling estrogen levels may also contribute.
As a result, a rectocele (prolapse of the back wall of your vagina) may form and lead to stool collecting in the pocket. That can create difficulty in emptying the rectum, which is then experienced as constipation and a sensation of incomplete evacuation of the rectum.
A referral to a urogynecologist may be beneficial to pursue the work-up necessary to identify any dysfunction and to determine the appropriate pelvic floor rehab.
Pelvic floor physical therapy may also be ordered. You may be instructed to do Kegel exercises in the interim (which are also helpful for those without an issue to help avoid one in the future with regard to both GI problems and urinary incontinence)
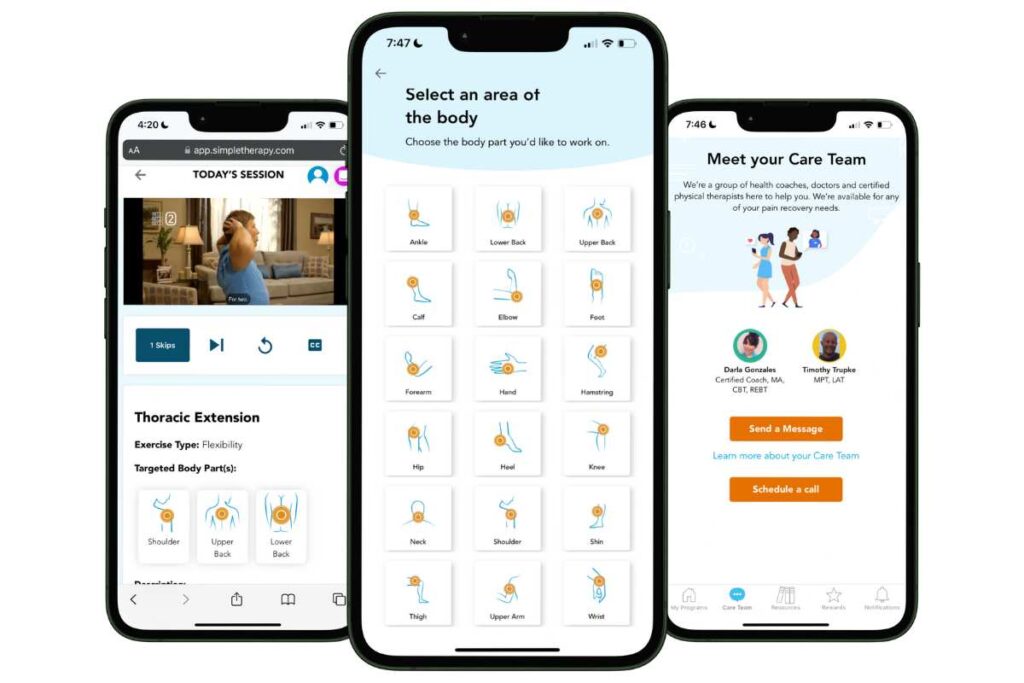
Free Physical Therapy
From the Comfort of Home
Only available for a limited time!
Become a member of the pausitive health pilot program and get physical therapist-led video exercises for the aches and pains (the musculoskeletal syndrome of menopause – MSM) that are common during the menopause journey. You can also access a program for pelvic floor issues like urinary leaking when you cough, sneeze, or laugh as well as problems with pelvic pain. The first 100 enrollees are also eligible for up to 2 live, virtual care physical therapy consultations.
You’ll also receive personalized text messages for your symptoms, a supportive community, and more!
Fiber-rich foods that help gas, bloating, and constipation
Simple changes to your eating habits, fluid intake, and physical activity levels can help get your GI tract moving again.
If you’re constipated, add fiber-rich foods to your diet, as well as those which help you to maintain a healthy gut microbiome. (link best foods). These include fruits and vegetables, whole grains, and nuts and seeds like:
- Artichokes
- Beans
- Banana
- Blackberries
- Bread, whole wheat
- Broccoli
- Brussel sprouts
- Carrots
- Cereal, high-fiber ready to eat
- Chia seeds
- Chickpeas
- Collard greens
- Dates
- Figs
- Flax seeds
- Oatmeal
- Orange
- Pear, skin included
- Peas
- Peanuts
- Pecans
- Pistachios
- Potato
- Popcorn
- Pumpkin seeds
- Prunes
- Quinoa
- Raspberries
- Rice, brown
- Spaghetti, whole wheat
- Spinach
- Yogurt
During menopause, it’s important to pay attention to the foods you’re consuming to ensure you get the nutrients you need during this stage of life.
Get the ultimate grocery list of foods for the menopause journey.
Make A Change For The Better!
This menopause grocery list contains a combination of foods specifically selected to help you feel better today and even better in the future.
"*" indicates required fields
If changes in your eating habits, fluid intake, and physical activity levels don’t do the trick, then HT might be considered, especially if you also suffer from other symptoms of menopause.
HT effectively addresses a range of menopause symptoms, including vaginal atrophy and vasomotor symptoms (VSMs) – hot flashes, night sweats, and palpitations. In that instance, some questions to be asked would be what dose and what form (e.g., oral, gel, suppository, patch) of HT will provide the best overall relief.
If you only have occasional, mild gas and bloating, then OTC simethicone and avoiding carbonated beverages and chewing gum might be suggested.

Heartburn and reflux
Heartburn refers to the burning sensation in your chest and esophagus. It can be caused by acid reflux, which is when you regurgitate stomach contents up into your esophagus, including the acid in your stomach, which helps to digest your food.
They’re symptoms of the upper GI tract.
Perimenopausal women are 2.9 times more likely to have upper GI symptoms than at any other stage of the menopause journey.
There are a number of factors for heartburn, including weight gain, obesity, spicy foods, alcohol, caffeine, fatty foods, acidic foods like orange juice and tomato sauce, eating before bed, and hormone therapy.
A 2023 study that reviewed five previous studies found a significant association between hormone therapy and the development of a common issue known as gastroesophageal reflux or GERD – which includes heartburn, chest pain, and difficulty swallowing.
Estrogen increases the production of stomach acid and a neurotransmitter that relaxes the esophagus’s lower portion. Progesterone also relaxes the esophageal muscles allowing stomach acid to flow freely.
More research is needed, but The Menopause Society said doctors should consider GERD risk factors when discussing menopause symptoms and treatment with patients.
Obesity is also a risk factor of GERD. So, once again, healthy eating and exercise can come to the rescue for menopause symptoms.

Can menopause cause nausea and vomiting?
I bet you thought nausea and vomiting were long gone now that pregnancy is out of the equation, but it’s back! Nausea is a menopause symptom for some women+. In some, vomiting may also occur.
Hormones are again at play, just like during pregnancy, for this awful feeling.
Elevated cortisol levels (a stress hormone) seen during the menopause journey can also play a role as it relates nausea, as it does with some of the GI symptoms.
If you’re feeling stressed, focus on stress management techniques to settle your mind and GI tract to help reverse the effects of elevated cortisol levels.
Nausea and hot flashes
Hot flashes can also cause nausea. It makes you think about the ways a hot flash affects you. It can cause your heart to beat fast, facial and neck flushing, sweat to pour down your face, and dizziness. So, add nausea to the list of ways hot flashes affect women.
Although it’s rare, blood pressure changes and palpitations during a hot flash can cause nausea in some women.
A digital diary-based study of 152 women in midlife published in the medical journal Menopause in 2016 found 5% of participants reported experiencing nausea with their hot flashes.
If this is the case for you, HT is likely the most effective relief route.
HT and nausea
A word of caution, though.
Hormone therapy, which many women take to address a wide range of symptoms, including hot flashes, can sometimes actually cause nausea. It’s uncommon, but it happens.
If you cannot use hormones or they contribute to your GI distress, then wearing clothes in layers, using cooling tubes, ice packs, fans, or wearables, avoiding alcohol, limiting spicy food, and quitting smoking can help.
And of course, talk to your doctor about your options.
If your PCP or GYN does not have the necessary training and expertise to provide the guidance you need, then see if you can find a clinician with the requisite knowledge base.

Menopause and diarrhea
Do you feel like you’re running to the bathroom more?
Diarrhea can be a symptom of menopause.
Elevated cortisol levels (a stress hormone) seen during the menopause journey can also cause diarrhea, nausea, vomiting, and constipation.
How to improve nausea, vomiting, and diarrhea
Take action to help manage cortisol levels by controlling the stress in your life. Techniques like mindfulness meditation, a gratitude practice, guided imagery, and listening to music can make a big difference (and provide the additional benefit of improving overall health and well-being over time).
Menopause is a perfect opportunity to focus on self-care and “me time.”
Additionally, for nausea and vomiting, additional steps that may help include:
- avoiding alcohol and hot caffeinated beverages
- ginger or peppermint tea or candy
- ginger ale
- cola syrup
- saltines
Irritable bowel syndrome (IBS) during menopause
Diarrhea is often associated with irritable bowel syndrome (IBS), along with abdominal pain and constipation.
IBS is a GI condition that may be diagnosed if the following (Rome) criteria are met:
- recurrent abdominal pain averaging at least 1 day/week within the last 3 months, associated with two or more of the following criteria:
- defecation
- change in the frequency of bowel movements
- change in the form (appearance, consistency) of the stool
Some patients with IBS experience primarily a problem with pain and constipation, while others may have diarrhea instead. And yet others may alternate between the two, in addition to the abdominal pain.
Individuals may also complain of bloating, a sense of incomplete evacuation, and mucus in the stool.
Women+ are more likely to have constipation compared to men, who are more likely to have diarrhea. As a result, women also tend to have more bloating and abdominal pain.
IBS affects 10 to 15% of the population in Western countries. Although twice as many women as men seek healthcare advice in the U.S. for this condition, it is not completely clear if the condition is actually more prevalent in women than men.
And, in some countries, the prevalence appears not to differ based on sex. However, the higher levels of estrogen and progesterone seen in those of the female sex can slow gut motility (movement), which would contribute to the greater prevalence of constipation rather than diarrhea in women than men with IBS.
Women are also more likely to experience depression, anxiety, and fatigue, which may be seen in those with IBS than men.
The rate of IBS diagnoses steadily declines as women age. If you are older than 50 and develop this pattern of symptoms, medical attention would typically be recommended by your provider. As one gets older, it is more likely that IBS will have already been diagnosed or that symptoms are not related to IBS.
The majority of people with the condition are diagnosed in their teens or early adulthood.
It’s not clear what role hormone fluctuations during the menopause transition may play when it comes to IBS. It should be noted that IBS symptoms often worsen around the time of one’s period when levels or estrogen and progesterone levels are lower than during the rest of the menstrual cycle.
And a major drop in estrogen and progesterone levels begins in perimenopause. That continues with volatility until leveling out during the post-menopause stage of the menopause journey.
There appears to be a greater sensitivity to visceral (felt in the internal organs of the body) pain in those with IBS. And some people with irritable bowel syndrome, as well as some with inflammatory bowel disease (Crohn’s disease and ulcerative colitis), have a greater sensitivity to hormonal changes, which in turn results in a greater likelihood of the perceived intensity of abdominal pain.
The impact of and role in treating IBS with HT is unclear, with some reports of improvement in symptoms while there are other accounts of it making things worse.
Although IBS can have a major negative impact on the quality of your life, it is important to remember it does not cause anemia or cancer, both of which can be seen in inflammatory bowel disease.
Gallstones during menopause
When estrogen and progesterone levels fall during the menopause transition, the motility (movement) of the GI tract can slow down.
The gallbladder may also empty more slowly the bile it contains (which is necessary for the digestion of food and absorption of fat and fat-soluble vitamins in the small intestine). As a consequence, the risk of developing gallstones increases.
For women+ using HT for menopause symptoms in a formulation which includes progestins, the risk of gallstones can also increase because of the negative impact it can have on gallbladder emptying. The likelihood of gallstones has been reported to be lower with HT gels or skin patches than with the use of oral HT.
Acute pancreatitis
The pancreas is an organ that secretes enzymes (amylase, lipase, protease) that aid digestion and produces hormones (insulin, glucagon, amylin, gastrin) that serve as messengers to other parts of the GI tract.
Some studies indicate that HT in post-menopausal women can increase the risk of acute pancreatitis, an inflammation of the pancreas. It is more likely to occur in those who take oral HT and who have been on HT for 10 years or more.
Theories of the connection between HT and acute pancreatitis include:
- increased risk of gallstones, a known cause of pancreatitis (e.g., the gallstone gets stuck in the pancreatic duct)
- increased level of triglycerides (a type of fat that circulates in the blood), known cause of acute pancreatitis if triglyceride levels are very high (due to a negative impact on blood flow in small blood vessels which results in a cut-off in blood flow to the pancreas)
There are non-hormonal options to help address menopause symptoms. If the risk of pancreatitis is a concern (or you experience an actual bout of pancreatitis), discuss alternatives to HT with your healthcare practitioner.
 Menopause and your gut microbiome
Menopause and your gut microbiome
In addition to the treatment options discussed, you may also want to focus on improving your gut microbiome.
Although a direct relationship has not been identified between the gut microbiome and GI symptoms during the menopause journey, researchers have found the menopause transition causes a change in the gut microbiome.
Thus far, the variety of organisms within the gut microbiome appears less during the menopause transition.
Why does this matter?
A of 2300 Hispanic/Latino individuals (of whom 293 were premenopausal women and 1027 were post-menopausal women) found menopause-related changes in the gut microbiome in post-menopausal women can negatively impact HDL (“good” cholesterol) levels, waist circumference, and the ability to achieve and maintain a healthy weight.
pausitve health’s Founder and Chief Medical Officer, Dr. Z. Colette Edwards, spoke with Under the Sisterhood about gut health and the microbiome.
How to improve your microbiome
Just as every person’s menopause journey is unique, the same is the case with regard to your gut microbiome. The number, type, and mix of microorganisms can be impacted by a wide range of factors, including what you eat and drink, antibiotics, GI surgery, whether you were delivered vaginally or via C-section, if you were breastfed or not, underlying medical conditions, medications, and your environment.
Prebiotics and probiotics can be ingested via certain foods and can help optimize your microbiome. Prebiotics are compounds in food that cause the growth and promote the activity of microorganisms that are beneficial. And the NIH defines probiotics as “live microorganisms that are intended to have health benefits when consumed or applied to the body.”
Prebiotic foods
Prebiotic foods include:
- asparagus
- garlic
- onions and leeks
- apples
- bananas
- oats
- barley
- jicama
- seaweed
Probiotic foods
Probiotic foods include:
- kim chi
- sauerkraut
- kefir
- kombucha
Research is ongoing to identify if, how, and under which circumstances oral probiotic supplements are beneficial.
High-fiber foods also impact both the type and number of microorganisms.
If you do not already have a high intake of prebiotic and/or high-fiber foods, it is helpful to increase your consumption and incorporate them gradually over time. Otherwise, a sudden increase can actually make symptoms like gas, bloating, and abdominal pain/cramping worse.

Race/ethnicity can impact GI symptoms
Women+ experience different frequencies and intensities of certain menopause symptoms, including GI symptoms, depending on their race/ethnicity and other factors.
The results of a study of 1051 women were reported in December 2021 by The Menopause Society. The analysis was based on two internet studies based on 12 questions related to health/menopausal and sociodemographic factors, of which nine questions addressed GI symptoms.
The Midlife Women’s Symptoms Index was used.
5% of women reported having GI symptoms.
The variability in GI symptoms included:
- Non-Hispanic white women had higher GI severity scores, especially with regard to diarrhea/constipation, nausea/vomiting, and loss of appetite.
- Non-Hispanic Black women had higher severity scores with regard to weight loss.
- Hispanic women/Latinas had higher GI severity scores related to bloating, constipation, and weight gain.
- Asian women were the least likely to have GI symptoms, and, when present, their symptoms were also less severe than for other groups.
Additionally, GI symptoms tended to increase throughout the menopause transition (except in Asian women), and both symptom severity and number of symptoms were greater in those women in the post-menopause stage of the journey.
Trust your gut
Trust your gut. The gut is often called the “second brain” because of the strong connection between gut health and how you feel. The health of your gut microbiome can even influence your mood, emotions, and certain mental health conditions.
So, the saying, “trust your gut,” is actually apropos!
A disruption to the gastrointestinal system is among the wide range of changes individuals can experience during the menopause journey. GI symptoms related to menopause are not among the most common.
However, for those who do experience GI shifts, there can be several potential causes. The good news is there are also many options to address them. So, don’t suffer in silence!
What is Cortisol? | EndocrineWeb
The Pelvic Floor As We Age | National Association for Continence
What is Pelvic Floor Therapy | WebMD
Kegel exercises – self care | MedlinePlus
Callan NGL, Mitchell ES, Heitkemper MM, Woods NF. Constipation and diarrhea during the menopause transition and early postmenopause: observations from the Seattle Midlife Women’s Health Study. Menopause. 2018 Jun;25(6):615-624. doi: 10.1097/GME.0000000000001057. PMID: 29381667; PMCID: PMC8080720.
Hormone Therapy May Cause Heartburn, Difficulty Swallowing, and Chest Pain | The Menopause Society
Fisher W, Thurston R. Measuring hot flash phenomenology using ambulatory prospective digital diaries. Menopause 23(11):p 1222-1227, November 2016. | DOI: 10.1097/GME.0000000000000685
Find a Menopause Practitioner | The Menopause Society
Heitkemper MM, Chang L. Do fluctuations in ovarian hormones affect gastrointestinal symptoms in women with irritable bowel syndrome? Gend Med. 2009;6 Suppl 2(Suppl 2):152-67. doi: 10.1016/j.genm.2009.03.004. PMID: 19406367; PMCID: PMC3322543.
Rome IV Criteria | Rome Foundation
Kim YS, Kim N. Sex-Gender Differences in Irritable Bowel Syndrome. J Neurogastroenterol Motil. 2018 Oct 1;24(4):544-558. doi: 10.5056/jnm18082. PMID: 30347934; PMCID: PMC6175559.
Oskarsson V, Orsini N, Sadr-Azodi O, Wolk A. Postmenopausal hormone replacement therapy and risk of acute pancreatitis: a prospective cohort study. CMAJ. 2014 Mar 18;186(5):338-44. doi: 10.1503/cmaj.131064. Epub 2014 Jan 27. PMID: 24468693; PMCID: PMC3956562.
High-Fiber Foods | HelpGuide.org
A good guide to good carbs: The glycemic index | The Presidents and Fellow of Harvard College
Arnone D, Chabot C, Heba A, Kökten T, Caron B, Hansmannel F, Dreumont N, Ananthakrishnan A, Quilliot D, Peyrin-Biroulet L. Sugars and Gastrointestinal Health.
Clinical Gastroenterology and Hepatology. 2022 Volume 20, Issue 9, Pages 1912-1924.e7. https://doi.org/10.1016/j.cgh.2021.12.011.
The Impact of Alcohol Consumption on Cardiovascular Health: Myths and Measures | World Heart Federation
No Amount of Alcohol Safe for the Heart, Federation Says | WebMD
Peters BA, Santoro N, Kaplan RC, Qi Q. Spotlight on the Gut Microbiome in Menopause: Current Insights. Int J Womens Health. 2022 Aug 10;14:1059-1072. doi: 10.2147/IJWH.S340491. PMID: 35983178; PMCID: PMC9379122.
Peters BA, Lin J, Qi Q, Usyk M, Isasi CR, Mossavar-Rahmani Y, Derby CA, Santoro N, Perreira KM, Daviglus ML, Kominiarek MA, Cai J, Knight R, Burk RD, Kaplan RC. Menopause Is Associated with an Altered Gut Microbiome and Estrobolome, with Implications for Adverse Cardiometabolic Risk in the Hispanic Community Health Study/Study of Latinos. mSystems. 2022 Jun 28;7(3):e0027322. doi: 10.1128/msystems.00273-22. Epub 2022 Apr 13. PMID: 35675542; PMCID: PMC9239235.
Probiotics: What You Need To Know | National Center for Complementary and Integrative Health
Im EO, Kim G, Choi M, Chee W. Gastrointestinal symptoms in four major racial/ethnic groups of midlife women: race/ethnicity and menopausal status. Menopause. 2021 Dec 6;29(2):156-163. doi: 10.1097/GME.0000000000001898. PMID: 34873105; PMCID: PMC8795485.
Kang Y, Han YR, Chang SJ, Chee W, Im EO. The Psychometric Properties of the Midlife Women’s Symptom Index. J Obstet Gynecol Neonatal Nurs. 2015 Sep-Oct;44(5):600-9. doi: 10.1111/1552-6909.12741. Epub 2015 Aug 18. PMID: 26285126; PMCID: PMC7646704.
Can a Healthier Gut Boost Your Mood? | EverdayHealth
You may also like…

Pelvic Floor Rehab: 10 Treatment Options During the Menopause Journey
Pelvic floor symptoms can be embarrasing, but don’t have to be. Learn about pelvic floor rehab options. Get treatment that’s right for you.

Menopause Matters: Understanding Pelvic Floor (Bladder and Bowel) Symptoms
Your pelvic floor is the “forgotten core” but your body may remind you of this area during the menopause journey, with bladder and bowel symptoms.

Foods For Menopause: 9 Best Foods To Help Menopause
Did you know you can manage your menopause symptoms with food? Learn the 10 best foods packed with the necessary nutrients to feel better.

