The Native community is diverse, and the unique cultures and health beliefs among the 574 federally recognized Indigenous Nations can shape the menopause journey for women+. It’s not just menopause symptoms that can impact a woman’s experience; the menopause journey can also impact a woman’s risk for chronic conditions. As a Native woman+, different risks and health disparities can affect your menopause journey. Knowledge is power. Learn about a “prescription for health” for Native American/Alaska Native women+.

Prescription for health for Native American/Alaska Native women+
The hormonal changes that occur during menopause, a natural stage of life, generally increase the risk of both physical and mental chronic conditions (regardless of race/ethnicity) and may make them more difficult to manage if you already have a diagnosis.
In the case of Native women+, hypertension, heart disease (including heart failure and an abnormal heart rhythm), and osteoporosis are more likely to be underlying conditions, the risk for which is further increased during the menopause journey.
Native women+ also have a greater likelihood of an earlier age of menopause onset, which not only further exacerbates the risk but means it exists for a longer period throughout a lifetime.
General health disparities
Those are the conditions associated with menopause, but there are also general health conditions for which there are health disparities for Native American/Alaska women+.
When it comes to cancer, the Native American community in the U.S. is not spared. The Office of Women’s Health reports Native women have a higher rate of kidney cancer.
Additionally, the Native community has the highest rate of liver and bile duct cancer, as well as higher death rates from kidney cancer than any other racial group, according to the National Cancer Institute (NCI).
And globally, Alaska Natives have the highest rate of colorectal cancer.
Lastly, life expectancy declined significantly in the U.S. across all racial groups due to the COVID-19 pandemic. However, pre-pandemic, the Native community had the lowest life expectancy (71.8 years), and it experienced the greatest decline (6.6 years) during the pandemic.
Now, let’s jump right in to review several specific conditions, so you can make a change for the better!
Cardiovascular Disease (CVD)
Cardiovascular disease includes hypertension, heart disease, and stroke, among other conditions. Heart disease is the number one cause of death in women+ across most racial groups.
However, if you are a Native woman, it falls to the number two position. While that’s good news, Native women+ still need to be on alert.
Native people have a 50% greater risk of developing CVD prematurely (age 60 or younger) compared to their white counterparts. And they are more likely to have coronary artery disease (blockage of the vessels in the heart), which can lead to heart attack.
Risk factors for CVD
When thinking about your risk, consider some of the risk factors. Do you have them?
When studying Native people located in Indian Health Service (IHS) regions, the CDC found that risk factors for CVD, like obesity, physical activity, and smoking, were found at higher rates compared to the white population, although there was variability depending on an individual’s IHS geographic region.
The American Heart Association reported disproportionate rates for several CVD risk factors for Native American/Alaska Native women.
- Diabetes was found in up to 72% of women
- Obesity affects almost 50% of Native American/Alaska Native women+.
- About one-third of Native American/Alaska women smoke, more than twice the amount who smoke in the U.S.
Symptoms of CVD
Like men, the most common symptoms of heart attack in women include:
- chest pain
- radiation of pain down the left arm/to the jaw
- shortness of breath
However, women may have other symptoms that are sometimes interpreted as being unrelated to a heart problem, including:
- nausea
- vomiting
- extreme fatigue
- lightheadedness
- shoulder or back pain
Be proactive and learn more about 18 risk factors for CVD to determine how many may apply to your particular situation.
Diabetes
Diabetes is a concern because it’s a CVD risk factor and because of the other ways it impacts your body.
Across racial groups, the rate of diabetes is greatest in the Native community, and Native people are more likely to experience gestational diabetes (during pregnancy), which increases the likelihood of developing diabetes at some point later in life.
There are two types of diabetes – type 1, when your body cannot make insulin, and type 2 – when your body does not use insulin effectively.
Insulin helps convert sugar (glucose) into energy for your body to use. So, sugar builds up in your blood and organs when insulin is not made or used well.
Symptoms
The most common symptoms are:
- increased thirst
- urination (pee)
But other symptoms include:
- tiredness
- numbness or tingling in your hands or feet
- slow wound healing
Diabetes that is not properly managed can lead to additional problems like heart and kidney issues, vision loss, and amputations.
Diagnosis
Diabetes is most commonly diagnosed with blood tests, usually with an A1C. This measures your average blood sugar levels over the past 3 months. If your A1C is 6.5% or higher, your doctor may diagnose you with diabetes.
Management of diabetes
Taking care of yourself is critically important when you have diabetes. Having regular visits with your healthcare practitioner can help keep you up to date on diabetes guidelines.
Preventive care to catch things early and help avoid complications includes monitoring sugar levels and your kidney function with blood tests, regular exams of your feet and eyes, and also paying attention to your emotional health.
Stress and depression are common in people with a chronic condition and can negatively impact your motivation to eat in a healthy fashion and be physically active, as well as make it harder to get enough good-quality sleep.
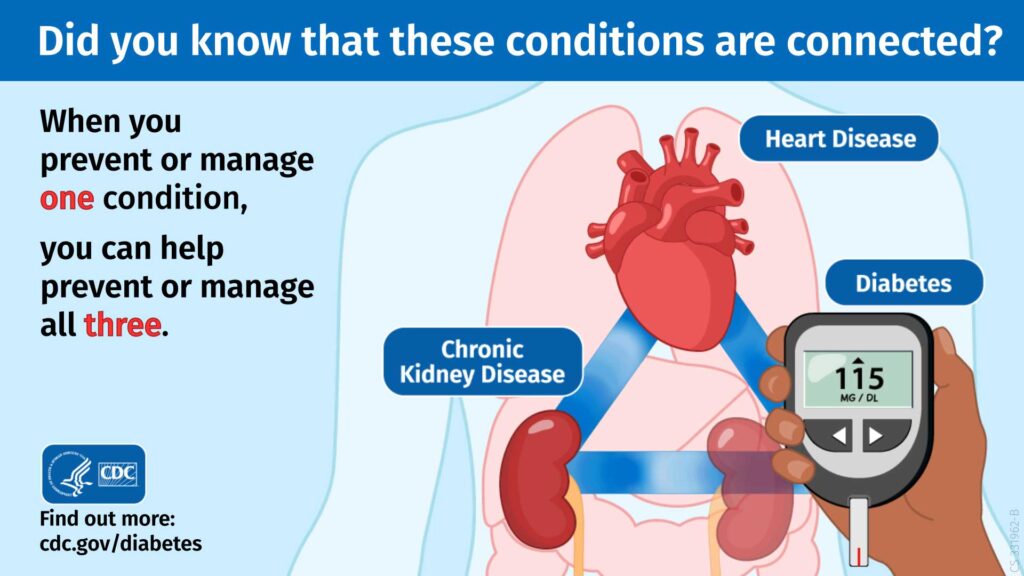
We talked about the connection between heart disease and diabetes, but there’s also a connection to chronic kidney disease.
The rate of end-stage renal (kidney) disease, i.e., ESRD, is 3.5 times higher in the Native population than in the white community.
Although they have survival rates following kidney transplantation comparable to white individuals, Native people have less access and wait longer for an organ.
That’s why it’s critical you take prevention seriously. Managing and preventing one condition can help you manage and prevent three conditions.
Native Americans and Alaska Natives are 50% more likely to be obese
than individuals in the white population.
Source: Office of Minority Health
Obesity
Obesity is a major health crisis in the U.S., with 42% of people falling into that weight category.
And there is a cascade of other chronic conditions which result or are made worse:
- diabetes
- cancer
- sleep apnea
- GI reflux
- hypertension
- high cholesterol
- stroke
- gallbladder disease
- osteoarthritis
- body pain
- mental health issues, including depression
In a study of close to 30,000 Native American and Alaska Natives age 50 or older of whom 30% received care from the Indian Health Service, some of the observations that made obesity more likely were:
- living 30 miles or more from a primary care facility
- having lower levels of education and income
- having transportation issues
- living in a county with a lower proportion of the population that was Native American/Alaska Native
And a CDC study found obesity was more prevalent in the Southern Plains region of the Indian Health Service.
Obesity prevention
Obesity is a chronic condition in which lifestyle factors can be leveraged to help reach and maintain a healthy weight:
- healthy eating
- regular physical activity
- getting adequate (7 – 9 hours) good-quality sleep
- managing stress
During the menopause journey, it can be harder to manage these lifestyle factors. You may find the hormone fluctuations disrupt your sleep, make you more stressed, or make you crave unhealthy foods.
Focusing on these lifestyle factors can help with chronic conditions like obesity and diabetes and your menopause symptoms.
You can use the Be Less Stressed Toolkit to help manage stress.
Be Less Stressed
Feeling stressed or overwhelmed? Learn life hacks to reduce stress with the Be Less Stressed toolkit.
"*" indicates required fields
It’s also important to connect with your primary care practitioner to make sure you don’t have another condition like thyroid disease that could be the cause of an unhealthy weight as well discuss your potential treatment options, including GLP-1 agonist medications, which are drugs originally developed for the treatment of diabetes but which also help with weight loss.
Cancer is the leading cause of death
for Native women.+
Cancer
Unlike in many populations where heart disease is the leading cause of death in women+, for Native women+ cancer is the top risk.
The risk factors for certain cancers may differ from other racial groups, and the prevalence of cancer may vary depending on the part of the country in which a person lives.
For example, a study of Native women in North Dakota found the major risk factors for breast cancer were starting one’s period at age 12 or 13 and never having delivered a live baby.
The Prevent Cancer Foundation has also reported geographic location can play a role. For example, the rates of different types of cancer in the Northeast region of the Indian Health Service (IHS) varied dramatically compared to the Southwest – lung cancer as the most common cancer in five of the six Indian Health Service (IHS) regions vs. in the Southwest, where it was only the fourth most common cancer.
Kidney cancer
Kidney cancer rates are rising in the Native community even though they’re on the decline as a whole in the U.S.
- develop kidney cancer at a younger age
- are diagnosed at a more advanced stage
- are more likely to die from it than those who are white
Renal cell carcinoma (RCC) is the most common type of kidney cancer and is seen in 90% of those with kidney cancer.
Risk factors include:
- family history of the disease
- genetic syndromes (e.g., von Hippel-Lindau disease, Cowden syndrome)
- smoking
- obesity
- chronic kidney disease, especially if severe enough to require dialysis
- high blood pressure
- toxin exposure (e.g., cadmium, trichloroethylene)
- long-term dialysis with the development of kidney cysts
- sickle cell trait/disease
- certain medications (e.g., acetaminophen)
Most people with kidney cancer don’t have symptoms on the early stages of the disease; but when they do, they can include some of the following:
- Blood in the urine (hematuria)
- Low back pain on one side (not caused by injury)
- A mass (lump) on the side or lower back
- Fever that is not caused by an infection and that doesn’t go away
- Anemia (low red blood cell counts)
Blood in the urine (hematuria)
It’s important to identify the reason for hematuria because this symptom can occur for many reasons, especially for women+ on the menopause journey.
UTIs can cause this symptom, and during the menopause journey, you may experience UTIs related to the genitourinary syndrome of menopause (GSM).
GSM refers to a wide range of symptoms, but generally refers to pain in your vagina, vulva, pelvis, or urinary tract and lower libido or pain during sex. The urinary symptoms often present as blood in the urine.
Given the increased risk for kidney cancer, if you see urine in your blood, don’t ignore it or assume it’s from a UTI.
Connect with your healthcare practitioner to determine the cause of the hematuria so you can get the appropriate treatment quickly.
For example, if it is related to GSM, in addition to antibiotics for the UTI, you may also be a candidate for hormone therapy to address the underlying issue, which might also include thin, dry vaginal tissue that can bleed easily and show up as blood in your urine.
If the cause is kidney cancer, your primary care practitioner will help you make arrangements for a consultation and further care from specialists like an oncologist (cancer doctor) and/or a surgeon.
Screening for kidney cancer
General screening is not recommended for those at average risk. For those at high risk, urine testing for blood and various imaging studies like ultrasound, CT, and MRI, may be ordered.
For individuals in which kidney cancer is diagnosed in Stage 1, the 5-year survival rate can be as high as 93%, according to the American Cancer Society.
So, talk to your doctor at the first sign of symptoms.
Colorectal cancer (CRC)
In the U.S., people younger than age 55 are the fastest-growing group to develop CRC.
In this age group, most of the cancers are located in the rectum or left side of the colon, increasing the likelihood of being found on screening.
There are several risk factors for CRC. Those seen more frequently in the Native community are in italics:
- Overweight/obesity
- Diabetes
- Alcohol consumption
- Cigarette smoking
- Physical inactivity
- Unhealthy eating – low-fiber, high-fat diet, red and processed meats
- Personal or family history of CRC
- Vitamin D deficiency
- Inflammatory bowel disease (IBD – Crohn’s disease and ulcerative colitis)
- Hereditary CRC syndromes (e.g., Lynch syndrome)
- Abdominopelvic radiation
- Having cystic fibrosis
Role of the microbiome
Most cancers begin in a polyp of a certain type (adenomatous). Studies show changes in the microbiome of Native people have been associated with that type of polyp. The changes have also been associated with progression of the cancer.
The health of your gut microbiome (the collection of bacteria, fungi, and viruses, and other microorganisms in your GI tract) is key to a well-functioning immune system. It can also help you manage your weight and cholesterol levels, protect brain and heart health, and maintain the ability to regulate sugar levels.
If your microbiome becomes unhealthy, (e.g., problem with number or diversity of organisms, presence of unhealthy bacteria) it can increase the risk of chronic conditions and cancer, including colon cancer.
A person’s dietary eating pattern has a major impact on the health of the gut microbiome. The Native community has long known and lived “food as medicine.”
The plant-based eating habits of Native peoples prior to their conquest by European settlers were ones that would have been protective against conditions like diabetes and colon cancer.
During the menopause journey, food as medicine, is vitally important. So, focus on the foods that can improve overall menopause symptoms and reduce risks for conditions like CRC.
Symptoms of CRC
Signs and symptoms of CRC include:
- blood in the stool
- rectal bleeding
- change in bowel habits
- change in size/shape of stool
- anemia
- abdominal pain
Screenings
Screening makes a difference!
The 5-year survival rate for colon cancer in those who were diagnosed in Stage 1 is 91%, as reported by the American Cancer Society.
Current guidelines for those at average risk recommend screening start at age 45.
There are several options for CRC screening, but colonoscopy remains the “gold standard.”
It’s important to seek guidance from your healthcare practitioner for your situation, as age, frequency, and best screening approach may differ in your particular case.
The mortality rate is 65% higher for Native American (and Black) women+
than for people who are white.
Source: American Cancer Society
Infection-Related Cancers
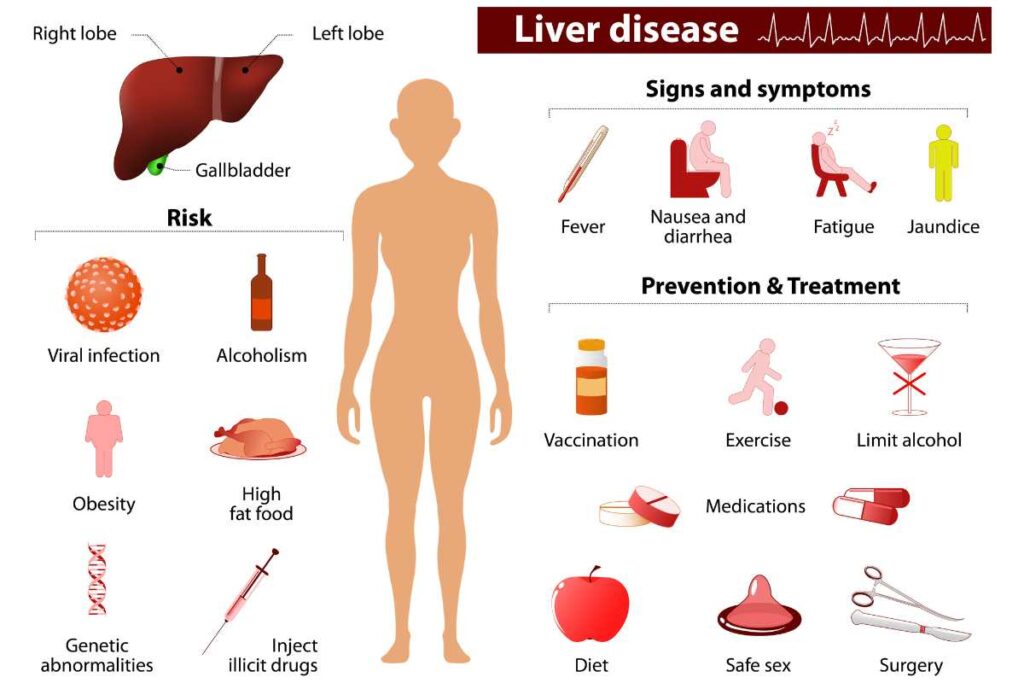
According to the CDC, Native women have higher rates of cancers which can be related to certain types of infection – cervical (HPV), stomach (Helicobacter pylori), liver, and bile duct (hepatitis B and C).
1. Cervical
The incidence of cervical cancer in the U.S. has been on the rise in women+ in ages 30 – 44.
The human papillomavirus (HPV) is the primary cause of cervical cancer, and infection with the virus is common in the general population.
Thankfully, there are opportunities to help prevent (HPV vaccine up to age 45) and catch the condition early (Pap smear and HPV testing).
So, taking action and staying up to date on preventive care guidelines for immunization and cancer screening is key to reducing your risk!
Although most types of cervical cancer are most commonly diagnosed between the ages of 35 and 44, 20% of people who develop it are actually 65 or older.
Symptoms you might experience are:
- abnormal vaginal bleeding (e.g., between your periods, after sex, after menopause)
- unusual vaginal discharge
- pain during sexual intercourse
- pelvic pain
Risk factors for cervical cancer include:
- Family history of cervical cancer
- Becoming sexually active at a young age (especially younger than 18 years old)
- Having many sexual partners or a high-risk partner (e.g., has many sexual partners, has an HPV infection)
- Having HIV
- Smoking
- History of having a chlamydia infection
- History of full-term pregnancy prior to age 20 or history of 3 or more full-term pregnancies
- Long-term use of birth control pills
- DES exposure
- Diet low in fruit and vegetables
Check out the CDC’s National Breast and Cervical Cancer Early Detection Program to see if you are eligible.
And consult with your OB-GYN regarding screening based on your personal situation. The age, frequency, and screening type may differ in your particular case.
2. Gastric (stomach)
Gastric cancer tends to grow slowly for years and is usually asymptomatic in the early stages. Therefore, unless certain actions are taken, it is usually diagnosed at an advanced stage.
Native women+ are at high risk for this type of cancer and should be on alert for symptoms and also should proactively talk with their healthcare practitioner about screening.
If caught during stage 1, the 5-year survival is 70%, vs. 7% for those diagnosed in stage 4.
Symptoms include:
- Feeling full quickly when eating
- Poor appetite
- Nausea, vomiting, indigestion
- Pain or discomfort in the upper part of the abdomen
- Unintentional weight loss
The more commonly seen risk factors in the Native community are in italics, and the others are generalized risk factors for stomach cancer:
- H. pylori infection
- Obesity
- Diabetes
- Diet high in fried food, processed meat and smoked fish, and red meat, plus low consumption of fruit and vegetables, milk, and vitamin A
- Alcohol consumption
- Smoking
- Exposure to environmental toxins
- Family history of gastric cancer
- Consumption of salt and salt-preserved food
- Ebstein-Barr virus infection (EBV)
- Gastric surgery
- Atrophic gastritis
- Consumption of nitrates
- Prior radiation of the abdomen related to treatment of other types of cancer
- CDH1, BRCA1, and BRCA2 gene mutations
- Hereditary cancer syndromes (e.g., Lynch syndrome, Peutz-Jeghers syndrome)
- Blood type A
- Gastric polyps
- Gastric ulcer
- Pernicious anemia
- Immigration from a country where gastric cancer rates are high (e.g., Korea, Japan, China, Vietnam, and Mongolia)
In countries where gastric cancer is common, certain actions are taken to reduce the likelihood of developing gastric cancer or to catch it early if someone already has it. They include:
- Proactive testing for H. pylori and treatment if found positive
- Upper endoscopy with biopsy
- Radiologic imaging
- Biomarker testing
In the U.S. screening of those at average risk is not routinely performed, as the overall prevalence in the general population is low.
However, if you are at high risk (e.g., first-degree relative with gastric cancer history, personal history of gastric surgery, being an immigrant from a country with a high incidence, being a Latina/Hispanic or Native woman+), speak with your healthcare practitioner about being screened.
Native women are 2x+ likely to have chronic liver disease and almost 5x more likely to die
from it, compared to women+ who are white.
Source: Office of Minority Health
3. Chronic Liver Disease (CLD), Cirrhosis, and Liver Cancer
There is a relationship between CLD, cirrhosis, and liver cancer. CLD can progress to cirrhosis, which in turn can lead to liver cancer.
And 80 – 90% of those who develop hepatocellular carcinoma (HCC – the most common type of liver cancer) have cirrhosis.
Some of the major causes of CLD-deaths in the U.S. include:
- Hepatitis C virus
- Alcohol
- Metabolic dysfunction-associated steatotic liver disease (MASLD) – previously known as non-alcoholic fatty liver (risk factors: obesity, diabetes, high blood pressure, high cholesterol; increases the risk of cardiovascular disease)
- Hepatitis B virus
The highest incidence (new infections) of hepatitis C in the U.S. is in the Native community, according to the CDC.
Additional risk factors for liver cancer include primary biliary cirrhosis, aflatoxins (a type of fungus that can contaminate peanuts, ground nuts, wheat, soybeans, corn, and rice), hemochromatosis, and anabolic steroids.
Thankfully, several of the risk factors are ones over which you have some degree of control.
Screening
There are tests available to detect both hepatitis B and C.
If you are found to be negative for the virus, there is a vaccine series you can take to prevent hepatitis B (80 – 100% effective), and if you are found to be positive, there is a medication regimen which has a high cure rate (98%) for hepatitis C!
Anabolic steroids (used by athletes to build muscle mass) and alcohol can be avoided altogether.
As is frequently the case with regard to many conditions and several cancers, living a healthy lifestyle can help reduce the risk of CLD/cirrhosis/liver cancer by addressing conditions like obesity, diabetes, and fatty liver.
You’ll even get a bonus for your efforts! A healthy lifestyle can also help:
- reduce the severity and frequency of menopausal symptoms
- reduce the chance of developing many of the physical and mental health conditions for which the risk increases due to the hormonal changes that occur during this stage of life.
Native American/Alaska Native communities have the highest rate of suicide
of all racial groups in the U.S.
Source: National Indian Council on Aging
Mental Health
In addition to physical health disparities, the Native community also has a greater burden of several mental health conditions. For example:
- The CDC reports Native people are “60% more likely to experience the feeling that everything is an effort.”
- The Native community also has the highest rate of substance use disorder, according to a survey by SAMHSA.
- For those who are also members of the LGBTQIA+ community, the rate of depression has been reported to be 43% by the Williams Institute of the UCLA School of Law.
- The prevalence of PTSD is higher in the Native community and can lead to self-medicating with alcohol.
Rates of depression, anxiety, alcohol and substance use disorder all rose during the COVID-19 pandemic, and the Native community was disproportionately impacted by the virus. Additionally, the virus itself can result in mental health issues.
Call 9-8-8

What’s behind these health disparities?
The many health disparities discussed above are examples of the impact of colonialism, seizure of Indigenous land, government policies that created and sustain systemic inequity, and bias/discrimination/racism on health, well-being, and longevity. The result has been a variety of social determinants of health (SDOH) experienced by many Indigenous people which lead to an increased risk of many lifestyle-related chronic conditions and cancers, including stomach cancer.
Some SDOH examples are insufficient access to healthy and affordable food/food insecurity and clean water/water insecurity, exposure to uranium and associated radiation, insufficient access to high-quality healthcare made worse by inadequate funding of the Indian Health Service, transportation challenges (54% of Native people live in rural or small town locations.), insufficient income to sustain a healthy lifestyle/higher rates of poverty, and inadequate access to broadband infrastructure.
Environmental Toxins
Environmental toxin exposure is a longstanding problem in the Native American community and may also be a contributory factor to chronic conditions and negative health outcomes.
In addition to the “forever chemicals” (PFAS) which plague us all, regardless of race/ethnicity, a meta-analysis of multiple Indigenous Nations in the U.S. that participate in the Strong Heart Study found exposure to persistent organic pollutants (POPs), open dumpsites, and heavy metals. Researchers report associations between these toxin exposures and not only cardiovascular disease but also diabetes, cancer, autoimmune disorders, and negative impacts on reproductive health and the nervous system.
EcoWatch provides tips to help limit your exposure to toxins, including ditching Teflon cookware, buying or growing organic produce, getting your home tested for radon and more.

The more you know, the more you will trust and the less you will fear.
~ Ojibwe saying
Time to take charge
As with other communities of color, there are many potential health disparities which may put you at a disadvantage when it comes to your health, well-being, and longevity. The hormonal changes that occur during this stage of life increase the risk of developing many of the conditions for which you may already be at baseline risk.
There is no better time than now to take charge and make a change for the better! pausitive health is here to help.
Resources
You may also like…
Osteoporosis 101: Know What To Look For and Foods That Can Help Prevent It
Osteoporosis is often undiagnosed and untreated in post-menopausal women+. It’s not curable, so prevent it with these foods and other lifestyle changes.

How Menopause Impacts Heart Health: 7 Action Steps That Help
Heart health lifestyle habits can help you manage menopause symptoms and help reduce the risk of cardiovascular disease.

Best Foods To Eat To Manage Restless Leg Syndrome (RLS)
Food as medicine. Get a list of the best foods to eat to manage restless leg syndrome (RLS) and avoid triggering it.
Disparities and the Leading Causes of Death in Women – National Women’s Health Week 2023 | Office on Women’s Health
Cancer Disparities | National Cancer Institute
Nash SH, Britton C, Redwood D. Characteristics of colorectal cancers among Alaska Native people before and after implementing programs to promote screening. J Cancer Policy. 2021 Sep;29:100293. doi: 10.1016/j.jcpo.2021.100293. Epub 2021 Jul 12. PMID: 35559952; PMCID: PMC8357310.
Fleck A. Native Americans Still Face Significant Life Expectancy Gap. Statista. Oct 9, 2023.
Heart health is sub-optimal among American Indian/Alaska Native women, supports needed | American Heart Association
Eberly LA, Shultz K, Merino M, et al. Cardiovascular Disease Burden and Outcomes Among American Indian and Alaska Native Medicare Beneficiaries. JAMA Netw Open. 2023;6(9):e2334923. doi:10.1001/jamanetworkopen.2023.34923
Zhao G, Hsia J, Vigo-Valentín A, Garvin WS, Town M. Health-Related Behavioral Risk Factors and Obesity Among American Indians and Alaska Natives of the United States: Assessing Variations by Indian Health Service Region. Prev Chronic Dis 2022;19:210298. DOI: http://dx.doi.org/10.5888/pcd19.210298
Latif W, Lambrinos KJ, Rodriguez R. Compare and Contrast the Glucagon-Like Peptide-1 Receptor Agonists (GLP1RAs) [Updated 2023 Mar 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK572151/
Menopause and Heart Health Infographic | American Heart Association
Heart health is sub-optimal among American Indian/Alaska Native women, supports needed | American Heart Association
Bkin BV, Rowe S, Sanni O, et.al. Prevalence of diabetes in pregnancy among Indigenous women in Australia, Canada, New Zealand, and the USA: a systematic review and meta-analysis. Volume 8, Issue 5, E681-E698, May 2020, doi::https://doi.org/10.1016/S2214-109X(20)30046-2
Diagnosis and Classification of Diabetes: Standards of Care in Diabetes—2024. American Diabetes Association Professional Practice Committee. Crossmark: Check for Updates. Diabetes Care 2024;47(Supplement_1):S20–S42. https://doi.org/10.2337/dc24-S002
Diabetes Symptoms | Centers for Disease Control and Prevention
Testing for Diabetes | Centers for Disease Control and Prevention
Did you know that these conditions are connected? Infographic | Centers for Disease Control and Prevention
Narva AS. Kidney disease in Native Americans. J Natl Med Assoc. 2002 Aug;94(8):738-42. PMID: 12152933; PMCID: PMC2594281.
Obesity and American Indians/Alaska Natives | Office of Minority Health
State of Obesity 2023: Better Policies for a Healthier America | Trust for America’s Health
Goins RT, Conway C, Reid M, Jiang L, Chang J, Huyser KR, Brega AG, Steiner JF, Fyfe-Johnson AL, Johnson-Jennings M, Hiratsuka V, Manson SM, O’Connell J. Social determinants of obesity in American Indian and Alaska Native peoples aged ≥ 50 years. Public Health Nutr. 2022 Apr 22;25(8):1-30. doi: 10.1017/S1368980022000945. Epub ahead of print. PMID: 35451356; PMCID: PMC9991752.
Luppino FS, de Wit LM, Bouvy PF, Stijnen T, Cuijpers P, Penninx BW, Zitman FG. Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010 Mar;67(3):220-9. doi: 10.1001/archgenpsychiatry.2010.2. PMID: 20194822.
Nadeau M, Best LG, Klug MG, Wise K. Exploring Clinical Risk Factors for Breast Cancer Among American Indian Women. Front Public Health. 2022 Jun 17;10:840280. doi: 10.3389/fpubh.2022.840280. PMID: 35784224; PMCID: PMC9247609.
Three things you might not know about how cancer affects Indigenous peoples | Prevent Cancer
Gonzalez V, Suflita M, Janitz A, Campbell J, McIntosh AG, Stratton K, Cookson MS, Parker DC. Kidney Cancer Incidence and Mortality Disparities Involving American Indians/Alaska Natives: An Analysis of the Oklahoma Central Cancer Registry (OCCR). J Cancer Epidemiol. 2022 Jun 19;2022:2689386. doi: 10.1155/2022/2689386. PMID: 35769890; PMCID: PMC9234047.
Batai K, Harb-De la Rosa A, Lwin A, Chaus F, Gachupin FC, Price E, Lee BR. Racial and Ethnic Disparities in Renal Cell Carcinoma: An Analysis of Clinical Characteristics. Clin Genitourin Cancer. 2019 Feb;17(1):e195-e202. doi: 10.1016/j.clgc.2018.10.012. Epub 2018 Oct 27. PMID: 30459061; PMCID: PMC6348034.
What Is Kidney Cancer? | American Cancer Society
Kidney Cancer: Risk Factors and Prevention | Cancer.Net
Survival Rates for Kidney Cancer | American Cancer Society
Haverkamp D, Redwood D, Roik E, Vindigni S, Thomas T. Elevated colorectal cancer incidence among American Indian/Alaska Native persons in Alaska compared to other populations worldwide. Int J Circumpolar Health. 2023 Dec;82(1):2184749. doi: 10.1080/22423982.2023.2184749. PMID: 36867106; PMCID: PMC9987760.
American Indian and Alaska Native People Experience a Health Burden from Commercial Tobacco | Centers for Disease Control and Prevention
Frost P. Vitamin D deficiency among northern Native Peoples: a real or apparent problem? Int J Circumpolar Health. 2012 Mar 19;71:18001. doi: 10.3402/IJCH.v71i0.18001. PMID: 22456053; PMCID: PMC3417586.
Malhotra R, Turner K, Sonnenberg A, Genta RM. High prevalence of inflammatory bowel disease in United States residents of Indian ancestry. Clin Gastroenterol Hepatol. 2015 Apr;13(4):683-9. doi: 10.1016/j.cgh.2014.06.035. Epub 2014 Jul 30. PMID: 25083563.
About Colorectal Cancer | Cystic Fibrosis Foundation
Ocvirk S, Wilson AS, Posma JM, Li JV, Koller KR, Day GM, Flanagan CA, Otto JE, Sacco PE, Sacco FD, Sapp FR, Wilson AS, Newton K, Brouard F, DeLany JP, Behnning M, Appolonia CN, Soni D, Bhatti F, Methé B, Fitch A, Morris A, Gaskins HR, Kinross J, Nicholson JK, Thomas TK, O’Keefe SJD. A prospective cohort analysis of gut microbial co-metabolism in Alaska Native and rural African people at high and low risk of colorectal cancer. Am J Clin Nutr. 2020 Feb 1;111(2):406-419. doi: 10.1093/ajcn/nqz301. PMID: 31851298; PMCID: PMC6997097.
Sarkar D, Walker-Swaney J, Shetty K. Food Diversity and Indigenous Food Systems to Combat Diet-Linked Chronic Diseases. Curr Dev Nutr. 2019 Sep 2;4(Suppl 1):3-11. doi: 10.1093/cdn/nzz099. PMID: 32258994; PMCID: PMC7101483.
Native American | Library of Congress
Survival Rates for Colorectal Cancer | American Cancer Society
Cancer and American Indian and Alaska Native People | Centers for Disease Control and Prevention
Key Statistics for Cervical Cancer | American Cancer Society
Risk Factors for Cervical Cancer | American Cancer Society
Find a Screening Program Near You | Centers for Disease Control and Prevention
Stomach Cancer Survival Rates | American Cancer Society
Shin WS, Xie F, Chen B, Yu P, Yu J, To KF, Kang W. Updated Epidemiology of Gastric Cancer in Asia: Decreased Incidence but Still a Big Challenge. Cancers (Basel). 2023 May 6;15(9):2639. doi: 10.3390/cancers15092639. PMID: 37174105; PMCID: PMC10177574.
Tests for Stomach Cancer | American Cancer Society
The Case for Biomarker Testing in Gastroesophageal Cancer | Medscape – January 22, 2024.
Chronic Liver Disease and American Indians/Alaska Natives | Office of Minority Health
Yanai H, Adachi H, Hakoshima M, Iida S, Katsuyama H. Metabolic-Dysfunction-Associated Steatotic Liver Disease-Its Pathophysiology, Association with Atherosclerosis and Cardiovascular Disease, and Treatments. Int J Mol Sci. 2023 Oct 23;24(20):15473. doi: 10.3390/ijms242015473. PMID: 37895151; PMCID: PMC10607514.
Hepatitis C Surveillance 2021 | Centers for Disease Control and Prevention
Hepatitis B | U.S. Department of Health and Human Services
Manns, MP and Maasoumy B. Breakthroughs in hepatitis C research: from discovery to cure. Nat Rev Gastroenterol Hepatol 19, 533–550 (2022). https://doi.org/10.1038/s41575-022-00608-8
American Indian Suicide Rate Increases | National Indian Council on Aging, Inc.
Brave Heart, M.Y.H., Lewis-Fernández, R., Beals, J. et al. Psychiatric disorders and mental health treatment in American Indians and Alaska Natives: results of the National Epidemiologic Survey on Alcohol and Related Conditions. Soc Psychiatry Psychiatr Epidemiol 51, 1033–1046 (2016). https://doi.org/10.1007/s00127-016-1225-4
Mental and Behavioral Health – American Indians/Alaska Natives | Office of Minority Health
Key Substance Use and Mental Health Indicators in the United States: Results from the 2021 National Survey on Drug Use and Health | Substance Abuse and Mental Health Services Administration
Bianca D.M. Wilson BDM, Bouton LJA, and Mallory C. American Indian and Alaskan Native LGBTQ Adults in the U.S.: LGBTQ Well-Being at the Intersection of Race. October 21, 2021.
Emerson MA, Moore RS, Caetano R. Association Between Lifetime Posttraumatic Stress Disorder and Past Year Alcohol Use Disorder Among American Indians/Alaska Natives and Non-Hispanic Whites. Alcohol Clin Exp Res. 2017 Mar;41(3):576-584. doi: 10.1111/acer.13322. Epub 2017 Jan 27. PMID: 28129438; PMCID: PMC5332276.
Hurwitz I, Yingling A, Amirkabirian T, Castillo A, Khan J, Do A, Lundquist D, Barnes O, Lambert C, Fieck A, Mertz G, Onyango C, Anyona S, Teixeira J P, Harkins M, Unruh M, Cheng Q, Leng S, Seidenberg P, Worsham A, Langsjoen J, Schneider K, Perkins D. Disproportionate impact of COVID-19 severity and mortality on hospitalized American Indian/Alaska Native patients, PNAS Nexus, Volume 2, Issue 8, August 2023, pgad259, https://doi.org/10.1093/pnasnexus/pgad259
Mental Health During the COVID-19 Pandemic | National Institutes of Health
Emerson MA, Moore RS, Caetano R. Association Between Lifetime Posttraumatic Stress Disorder and Past Year Alcohol Use Disorder Among American Indians/Alaska Natives and Non-Hispanic Whites. Alcohol Clin Exp Res. 2017 Mar;41(3):576-584. doi: 10.1111/acer.13322. Epub 2017 Jan 27. PMID: 28129438; PMCID: PMC5332276.
Institute of Medicine (US) Committee on the Ethical and Legal Issues Relating to the Inclusion of Women in Clinical Studies; Mastroianni AC, Faden R, Federman D, editors. Women and Health Research. Washington (DC): National Academies Press (US); 1999.
Maillacheruvu SU. The Historical Determinants of Food Insecurity in Native Communities. Center Budget and Policy Priorities. October 2, 2022.
Martin C, Simonds VW, Young SL, Doyle J, Lefthand M, Eggers MJ. Our Relationship to Water and Experience of Water Insecurity among Apsáalooke (Crow Indian) People, Montana. Int J Environ Res Public Health. 2021 Jan 12;18(2):582. doi: 10.3390/ijerph18020582. PMID: 33445579; PMCID: PMC7827827.
Warne D, Frizzell LB. American Indian health policy: historical trends and contemporary issues. Am J Public Health. 2014 Jun;104 Suppl 3(Suppl 3):S263-7. doi: 10.2105/AJPH.2013.301682. Epub 2014 Apr 22. PMID: 24754649; PMCID: PMC4035886.
Dewees S, Marks B, First Nations Development Institute. Research Note—Twice Invisible: Understanding Rural Native America. First Nations Development Institute; 2017. Accessed September 24, 2021.
Brook D. Environmental Genocide: Native Americans and Toxic Waste. The American Journal of Economics and Sociology. Vol. 57, No. 1 (Jan., 1998), pp. 105-113.
Meltzer, G.Y., Watkins, BX., Vieira, D. et al. A Systematic Review of Environmental Health Outcomes in Selected American Indian and Alaska Native Populations. J. Racial and Ethnic Health Disparities 7, 698–739 (2020). https://doi.org/10.1007/s40615-020-00700-2
Our Current Understanding of the Human Health and Environmental Risks of PFAS | United States Environmental Protection Agency
End Colon Cancer in Indian County | American Indian Cancer Foundation
Meltzer GY, Watkins BX, Vieira D, Zelikoff JT, Boden-Albala B. A Systematic Review of Environmental Health Outcomes in Selected American Indian and Alaska Native Populations. J Racial Ethn Health Disparities. 2020 Aug;7(4):698-739. doi: 10.1007/s40615-020-00700-2. Epub 2020 Jan 23. PMID: 31974734.
Strong Heart Study | The University of Oklahoma Health Sciences Center
Everything Toxins 101: Everything You Need to Know | EcoWatch
Home | American Heart Association
Home | Indian Health Service
Mental Health Resources | SAMHSA
Home | 988 Suicide & Crisis Lifeline
Home | Crisis Text Line
Air pollution: How to reduce harm to your health | Harvard Medical School
Heavy Metal Detox Diet | Healthline Media
What is a heavy metal detox? | Healthline Media

